Abstract
The spleen may be preserved during distal pancreatectomy (DP) for benign disease. The aim of this study was to compare the perioperative and postoperative courses of patients with conventional DP and spleen-preserving distal pancreatectomy (SPDP) for benign lesions or tumors with low-grade malignant potential occurred at the body or tail of the pancreas. A retrospective analysis was performed for the hospital records of all the patients undergoing DP and SPDP between January 1995 and April 2006. One-hundred forty-three patients underwent DP and 37 patients underwent SPDP. There were no significant differences in age, sex, indications of operation, estimated blood loss, operative time, and postoperative hospital stay between the two groups. Pancreatic fistula occurred in 21 (13.3%) patients following DP and in 3 (8.1%) following SPDP without a significant difference (p=0.081). Portal vein thrombosis occurred in 4 patients after DP. Splenic infarction occurred in one patient after SPDP. Overwhelming postosplenectomy infection was observed in one patient after DP. SPDP can be achieved with no increase in complication rate, operative time, or length of postoperative hospitalization as compared to conventional DP. Additionally, it has the advantage of reducing the risk of overwhelming postsplenectomy infection and postoperative venous thrombosis.
Distal pancreatectomy (DP) is the operation of choice for benign or malignant disease in the body or tail of the pancreas. Splenectomy in conjunction with distal pancreatectomy is clearly indicated in most patients with adenocarcinoma of the pancreas, as splenic preservation may compromise the oncologic resection. However, for benign lesions or tumors with low-grade malignant potential, the issue of splenic preservation remained controversial. To reduce the risk of post-splenectomy sepsis and hematologic disorders, several authors have emphasized the benefits of spleen preservation (1-3). On the other hand, some authors suggest that splenic preservation is more difficult, time-consuming, and is associated with increased blood loss from small venous tributaries (4).
Thus, the aim of this study was to evaluate the clinical efficacy of spleen-preserving distal pancreatectomy (SPDP) by comparing the perioperative factors and postoperative courses between DP and SPDP for benign lesions or tumors with low-grade malignant potential of the body and tail of the pancreas.
From January 1995 to April 2006, 143 patients underwent DP and the 37 patients underwent SPDP for benign or low-grade malignant disease at Seoul National University Hospital, Seoul, South Korea. Spleen preservation was achieved in which the pancreas was dissected off the splenic vessels. The medical records were reviewed to evaluate the clinical outcomes such as surgical factors (operation time, estimated blood loss, transfusion), postoperative complications, and postoperative long-term outcomes (endocrine/exocrine function, and recurrence).
Of these, laparoscopic DP was performed in 14 patients and laparoscopic SPDP in one patient.
Vaccination against Pneumococcus, Haemophilus influenza b and Neisseria meningitides was not performed routinely.
DP was performed in a standard fashion. Division of the pancreatic parenchyma was conducted via electrocautery and mass. Direct ligation of the main pancreatic duct was done with non-absorbable suture. The pancreatic stump was oversewn with suture reinforcement using 4-0 black silk or 4-0 polypropylene (prolene*, Ethicon, Somerville, NJ, U.S.A.). For the laparoscopic DP, the pancreas was transected using the 48- or 35-mm vascular endoscopic linear stapler (Endo-GIA stapler with vascular cartridge; Autosuture Corp., Norwalk, CT, U.S.A.). In SPDP, both splenic artery and vein were preserved. One closed suction drain was positioned in the splenic fossa close to the transected pancreas. In SPDP, both the splenic artery and vein were preserved.
A pancreatic fistula was defined as drainage of more than 30 mL of fluid with an amylase level higher than 600 U/dL on or after postoperative week 1 (5). Postoperative octreotide was given subcutaneously (dose 100 mg every 8 hr) for the patients considered high risk for pancreatic fistula based on the gland texture and duct size.
Comparison of outcomes between the two groups was performed using the chi-square test and Student's t-test where appropriate. Results are reported as mean±standard deviation. Statistical significance was accepted at p<0.05.
Clinical features of patients and indications for DP with or without splenectomy are shown in Table 1. There were no significant differences in age, sex, preoperative diabetes mellitus, preoperative WBC count, platelet count, and indications.
SPDP was successfully performed in all 37 patients. Conservation of the splenic artery and vein during SPDP was possible in all patients.
Four patients in the DP group and one patient in the SPDP group underwent pancreaticojejunostomy due to the stricture of proximal pancreatic duct caused by chronic pancreatitis.
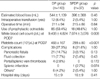
There were no postoperative deaths. Operative details and postoperative complications are shown in Table 2. There were no significant differences in estimated blood loss, intraoperative transfusion and operative time between the two groups. The white blood cells (WBC) and the platelet counts examined one week after operation were significantly higher in the DP group than the SPDP group (p<0.05). The incidence of complications was 27.3% (39/143) in the DP group comparing 21.6% (8/37) in the SPDP group, and this was not statistically significant. The incidence of pancreatic fistula in the DP group was 14.7% (21/143) and 8.1% (3/37) in the SPDP group. There was no significant difference between the two groups. For 85 patients in the DP group and 18 patients in the SPDP group, prophylactic octreotide was used. Of these patients, pancreatic fistula occurred in 10 patients (11.8%, 10/85) of the DP group and in one patient (5.6%, 1/18) of the SPDP group. The mean duration of hospital stay was 15±9 days for patients in the DP group and 16±9 days for the SPDP group. Splenic vein thrombosis occurred in one patient who underwent DP. He received anticoagulation treatment and there was no more progression of the thrombosis. Portal vein thrombosis occurred in three patients after DP. They received no specific treatment, and spontaneous resolution of the thrombosis occurred as detected by radiologic imaging studies. Splenic infarction occurred in one patient of the SPDP group. On the CT scan 4 yr after surgery, the appearance of volume loss with multifocal low attenuated lesions of the spleen with an intact splenic artery was detected without any overt symptoms. The patient is still alive with no issues 7 yr after surgery. There was one patient who was suspected of overwhelming postsplenectomy sepsis (OPSI) and this was the only patient who experienced septic shock in our study. A 65-yr-old male patient who was previously healthy underwent DP with splenectomy due to intraductal papillary mucinous neoplasm. On the 9th postoperative day, fever developed and on ultrasonography, small fluid collection was observed near the DP site. Percutaneous drainage was performed and 30 mL of pus-like fluid was aspirated. Next day, he became suddenly hypotensive but no additional finding was detected on abdominal CT comparing ultrasonographic images received the previous day. Shewanella algae was cultured from peripheral blood. Intravenous antibiotics treatment was performed and his medical condition had been improved.
The mean follow-up period was 36±33 months in the DP group and 41±30 months in the SPDP group (Table 3). The WBC and the platelet counts examined at 6 months after the operation were significantly higher in the DP group than the SPDP group (p<0.05). Regarding endocrine function, 16 and 4 patients had diabetes mellitus in the DP group and SPDP group, respectively. Diabetes did not get worse in any patient following DP or SPDP. Among the patients with preoperative normoglycemia, newly developed diabetes mellitus was noted in 16 patients in the DP group and 4 patients in the SPPD group. There was no significant difference between the two groups. Recurrence occurred in one patient 5 yr later after undergoing DP due to intraductal papillary mucinous neoplasm. Total pancreatectomy was performed and the permanent pathologic report showed intraductal papillary mucinous carcinoma.
Splenectomy during a DP is performed frequently because of its technical simplicity and clear indication in the majority of patients with adenocarcinoma of the pancreas, as splenic preservation may compromise the oncologic resection. However SPDP has been performed because of increasing interest in splenic salvage because of the increased risk of infection, changes in peripheral blood counts (6-8) and consideration of overwhelming postsplenectomy sepsis (6-8).
There are currently four retrospective reviews comparing outcomes after DP with or without splenectomy (4, 9-11). Richardson and Scott-Conner (9) reported on 21 patients, who underwent surgery for trauma, and found no differences in complication rates between groups, concluding that splenectomy could be accomplished in selected cases. Aldridge and Williamson (10) reported on 77 patients, who underwent surgery for chronic pancreatitis, and also concluded that the spleen can be preserved safely. Benoist et al. (11) found in 40 patients with benign lesions other than pancreatitis that the complication rate was twice as high in the splenic preservation group as compared to the splenectomy patients. They concluded that DP with splenectomy is the best procedure for benign disease of the tail and body of the pancreas. In the largest series in the literature, Shoup et al. (4) evaluated 125 patients who underwent DP for benign or low-malignant potential tumors. In this series from Memorial Sloan-Kettering Cancer Center, 79 patients underwent splenectomy and 46 underwent splenic preservation. The overall complication rates were similar between the two groups; however, patients undergoing splenectomy had a significantly higher rate of infectious complications (28% for splenectomy, 9% for splenic preservation, p=0.01) and severe complications (11% vs. 2%, p=0.05) compared with those who had splenic preservation. Their conclusion was that splenic preserving DP is safe and can be performed with decreased perioperative morbidity compared with conventional pancreatectomy with splenectomy and should be the operation of choice, when feasible, for distal pancreatic disease other than adenocarcinoma.
In our study, splenic preservation has not increased the operative time, intraoperative bleeding, complication rate including pancreatic fistula, or length of hospital stay associated with DP. However, there was only one patient who was suspected of overwhelming postsplenectomy sepsis (OPSI). OPSI had been defined as septicemia and/or meningitis, usually fulminant but not necessarily fatal, occurring at any time after removal of the spleen (12). Although the incidence of infection after splenectomy in adults ranging from 0.28% to 1.9% with a 2.2% mortality rate (13, 14) may be low, the infections are fatal. Therefore, distal pancreatectomy with splenectomy should be the operation of choice, when feasible.
In the present study, there were 3 patients who experienced portal vein or splenic vein thrombosis after DP with splenectomy due to non-hematologic disease. Their platelet counts were less than 300×103/µL at the time of diagnosis of venous thrombosis. Fortunately, in all three patients, the extent of venous thrombosis was reduced without specific treatment. The presentation of portal vein thrombosis is vague, without defining signs or symptoms. Unless the surgeon has a high index of suspicion, this complication may go undetected. The progression of the thrombus to occlude the portal and mesenteric veins could cause acute hypertension in the splanchnic circulation resulting in intestinal infarction. Although the reported incidence of this complication is low (15, 16), even vague symptoms must be considered seriously following splenectomy.
Our results show that SPDP with the preservation of the splenic vessels can be safely performed without increasing operative time, and length of postoperative hospitalization, or increasing the postoperative complication rate. Additionally, SPDP has the advantage of reducing the risk of overwhelming postsplenectomy infection and postoperative venous thrombosis. Therefore, SPDP is worth considering for the treatment of benign or low-grade malignant potential lesions of the body or tail of the pancreas.
Figures and Tables
Table 1
Preoperative findings in patients undergoing distal pancreatectomy with splenectomy (DP group) and without splenectomy (SPDP group)
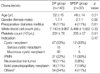
*, Others include pseudocyst, chronic pancreatitis, benign cyst, cystic lymphangioma, lymphoepithelial cyst, SMA aneurysm, arteriovenous malformation, pleuropancreatic fistula, accessory spleen, splenic artery rupture, splenic hematoma.
DP, distal pancreatectomy; SPDP, spleen-preserving distal pancreatectomy; IPMN, intraductal papillary mucinous neoplasm.
References
2. Kimura W, Inoue T, Futakawa N, Shinkai H, Han I, Muto T. Spleen-preserving distal pancreatectomy with conservation of the splenic artery and vein. Surgery. 1996. 120:885–890.

4. Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg. 2002. 137:164–168.

5. Kim SW, Youk EG, Park YH. Comparison of pancreatogastrostomy and pancreatojejunostomy after pancreatoduodenectomy performed by one surgeon. World J Surg. 1997. 21:640–643.

6. Leonard AS, Giebink GS, Baesl TJ, Krivit W. The overwhelming postsplenectomy sepsis problem. World J Surg. 1980. 4:423–432.

8. Malangoni MA, Dillon LD, Klamer TW, Condon RE. Factors influencing the risk of early and late serious infections in adults after splenectomy for trauma. Surgery. 1984. 96:775–783.
9. Richardson DQ, Scott-Conner CE. Distal pancreatectomy with and without splenectomy: a comparative study. Am Surg. 1989. 55:21–25.
10. Aldridge MC, Williamson RC. Distal pancreatectomy with and without splenectomy. Br J Surg. 1991. 78:976–979.

11. Benoist S, Dugue L, Sauvanet A, Valverde A, Mauvais F, Paye F, Farges O, Belghiti J. Is there a role of preservation of the spleen in distal pancreatectomy? J Am Coll Surg. 1999. 188:255–260.

12. Waghorn DJ. Overwhelming infection in asplenic patients: current best practice preventive measure are not being followed. J Clin Pathol. 2001. 54:214–218.
13. Holdsworth RJ, Irving AD, Cuschieri A. Postsplenectomy sepsis and its mortality rate: actual versus perceived risks. Br J Surg. 1991. 78:1031–1038.

14. Lynch A, Kapila R. Overwhelming postsplenectomy infection. Infect Dis Clin North Am. 1996. 10:693–707.

15. Kunin N, Desjardins JF, Letoquart JP, La Gamma A, Lebois E, Mambrini A. Mesenteric-portal thrombosis after hematologic splenectomy. J Chir (Paris). 1996. 133:453–458.
16. van't Riet M, Burger JW, van Muiswinkel JM, Kazemier G, Schipperus MR, Bonjer HJ. Diagnosis and treatment of portal vein thrombosis following splenectomy. Br J Surg. 2000. 87:1229–1233.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download