Abstract
We report a case of pure red cell aplasia (PRCA), which was initially suspected as a result of bone marrow involvement of diffuse large B cell lymphoma. Persistent anemia without an obvious cause was observed in a 47-yr-old man diagnosed with relapsed diffuse large B cell lymphoma. The bone marrow study showed only erythroid hypoplasia without the evidence of bone marrow involvement with lymphoma cells, thus PRCA was suggested. However, parvovirus infection was excluded as a potential cause of PRCA because of negative IgM anti-parvovirus B19 antibody and negative parvovirus PCR in the serum. Latent Epstein-Barr virus (EBV) infection of bone marrow was suggested by in situ hybridization with EBV-encoded small RNA (EBER) that showed a strong positive expression in bone marrow cells. Thus, PRCA was thought to be associated with latent EBV infection in bone marrow cells. Although the finding of unexplained anemia is a possible predictor of bone marrow involvement with lymphoma cells, PRCA as a result of a viral infection including EBV should be considered in lymphoma patients. This is the first report of the occurrence of PRCA associated with latent EBV infection in a patient with non-Hodgkin's lymphoma.
Anemia is one of the most common hematologic manifestations in patients with malignant lymphomas. There are many potential causes, including: chemotherapy-induced myelosuppression, anemia of chronic disease associated with treatment or disease-related morbidity, autoimmune hemolytic anemia, iron deficiency, and neoplastic infiltration of bone marrow. Recently, it was reported that a hemoglobin less than 10 g/dL may be a finding predictive of bone marrow involvement in patients with diffuse large B cell lymphoma (1). Because it is not uncommon to find lymphoma cell infiltation in bone marrow, anemia should be thoroughly evaluated especially when it is found in patients with recurrent non-Hodgkin's lymphoma. However, since the causes of anemia are not always related to lymphoma-related manifestations, other possible causes of anemia must be evaluated especially when the findings of anemia are isolated without any other hematologic findings.
Pure red cell aplasia (PRCA) is a rare hematological condition characterized by an isolated anemia, normocytic normochromic, with reticulocytopenia and erythroid hypoplasia of the bone marrow with normal megakaryocytic and myeloid cell lineages. Although this condition rarely occurs in nonthymic lymphoproliferative disorders, a few cases of PRCA have been reported in patients with diffuse large B cell lymphoma. Most reported cases are due to parvovirus B19 infection after stem cell transplantation or monoclonal antibody treatment (2-5). These cases of infection might be associated with a compromised immune system as a result of treatments. However, latent Epstein-Barr virus (EBV) infection-induced PRCA is uncommon and it has never been reported in a patient with non-Hodgkin's lymphoma. Herein, we report a case of PRCA, which was initially suspected to be a result of bone marrow involvement of diffuse large B cell lymphoma.
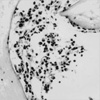
A 43-yr-old male patient was admitted to our hospital because of painless cervical lymph node enlargement in 2000. He was diagnosed with diffuse large B cell lymphoma by evaluations of excisional biopsy of cervical lymph nodes. He was staged as IIA according to the Ann Arbor staging system, and bone marrow aspirates and biopsy revealed absence of lymphoma cell infiltration. The patient achieved complete remission with CEOP-B chemotherapy (cyclophosphamide, epirubicin, oncovin, prednisone, and bleomycin). The patient was readmitted to our hospital because of a painless mass in his right supraclavicular region on 12 November 2004. Chest computerized tomography (CT) scan showed a 2×3 cm-sized lymph node enlargement in the right supraclavicular fossa. In addition, multiple lymph nodes in the right upper mediastinum were observed, which these had not been observed in previous CT scans. Multiple lymph node enlargements of mesentery and left para-aortic areas were also found on the abdomino-pelvic CT scan. Recurrence of diffuse large B cell lymphoma was confirmed by biopsy of a supraclavicular lymph node. Serum LDH and beta-2 microglobulin were elevated up to 507 IU/L and 3.60 mg/L, respectively. Other laboratory studies on admission were within normal ranges except complete blood cell (CBC) counts that showed: hemoglobin 9.7 g/dL (which was 14.1 g/dL 3 months before), reticulocyte 2,600/mL, MCV 103 fl, leukocytes 5.74×109/L, and platelets 326×109/L. Serum vitamin B12, folate, haptoglobin and ferritin levels were within normal ranges; however, serum erythropoietin was elevated at 71.7 mU/mL (normal, 10.2-25.2). There was no evidence of internal bleeding such as gastrointestinal bleeding or autoimmune hemolytic anemia. The Coomb's test was negative. To exclude the possibility of bone marrow infiltration by lymphoma cells, bone marrow aspiration and biopsy were performed on bilateral iliac crest. However, severe paucity of erythroid cells with intact myeloid and megakaryocytic lineages was observed (Fig. 1), and there was no neoplastic cell infiltration in the marrow (Fig. 2). Thus, we suspected anemia associated with other causes including PRCA associated with viral infection especially parvovirus B19. However, there was no evidence supporting parvovirus infection. Laboratory findings revealed negative anti-parvovirus B19 IgM antibody in serum and negative parvovirus B19 DNA in polymerase chain reaction with the patient's blood samples. Serological investigations for an acute infection for cytomegalovirus, hepatitis-A, -B and -C virus were all negative. However, we found that IgG antibody against EBV (EBNA) was positive, although the heterophil antibody and EBV VCA IgM antibody were negative in the patient's serum. Thus, we performed in situ hybridization with EBV-encoded small RNA (EBER) in a bone marrow section from the patient and found a positive expression of EBER in the bone marrow cells, which suggested latent EBV infection in bone marrow (Fig. 3). During two cycles of salvage chemotherapy, the CBC findings showed severe persistent hematologic toxicity confined to anemia; the hemoglobin level was around 4.5 g/dL for several months even after the completion of chemotherapy; however, leukocyte and platelet counts recovered to the normal ranges. After salvage chemotherapy, the patient achieved complete remission again; however, the anemia persisted and required repeated red blood cell transfusions.
Acquired PRCA has a variety of causes. Viral infection is a common cause of PRCA. Among viruses capable of suppressing erythropoiesis, human parvovirus B19 is well-represented. This DNA virus infects erythrocytes by binding to the P antigen on the cell membranes resulting in suppression of erythropoiesis. However, the virus does not attach to the myeloid cells. Suppressed erythropoiesis is transient in healthy hosts who spontaneously recover in a short period of time. However, the suppression of erythropoiesis can persist, leading to PRCA owing to persistent viremia in immunecompromised individuals such as patients with HIV, sarcoidosis, and hematologic malignancy, transplant recipients, and patients treated with chemotherapy or immunosuppresive agents. There have been a few case reports of parvovirus B19 infection-induced PRCA in patients with B-cell lymphoma receiving anti-CD20 monoclonal antibody rituximab (3, 6). This might be related to compromised humoral immunity by B-lymphocyte depletion. PRCA has also been reported to present as an initial manifestation unrelated to treatment in many types of lymphoma (7-10). Co-existence of autoimmune hemolytic anemia and PRCA in malignant lymphoma has also been reported (11-13). Because malignant lymphoma is often associated with immunological disorders such as hemolytic anemia, it is conceivable that warm autoantibody against red blood cells may damage erythroid progenitors resulting in PRCA (14).
However, our case had no evidence of parvovirus B19 infection or hemolytic anemia. Bone marrow invasion by lymphoma was suspected in our case. However, there was no evidence of bone marrow involvement of diffuse large B cell lymphoma. In situ hybridization with EBER in bone marrow suggests occult bone marrow invasion as has been previously reported in a case of extranodal NK/T cell lymphoma (15). However, there is no prior report of positive EBER in situ hybridization as a marker for occult bone marrow involvement of diffuse large B cell lymphoma as in extranodal NK/T cell lymphoma. Therefore, it is unlikely that an occult bone marrow involvement resulted in PRCA in our case.
Occurrence of PRCA in non-Hodgkin's lymphoma is also reported to be associated with the presence of inhibitory factors in the serum, which suppress erythropoiesis in the bone marrow (16). The association of serum IgG inhibitor of bone marrow progenitor cells with the development of PRCA has been reported in patients with follicular small cleaved B cell lymphoma (17). These inhibitory factors might be related to the underlying disease, lymphoma. However, an exact causal relationship remains to be defined.
In our case, EBV infection was suggested as a cause of PRCA based on the results of in situ hybridization with EBER. EBV is also known to be a cause of PRCA, although it is not as common as parvovirus B19. In a case report of PRCA associated with chronic EBV infection, in vitro culture of bone marrow cells from a patient and a healthy control showed that the formation of erythroid colony forming (ECF) units from the patient were reduced by 50% compared to the healthy control (18). However, T-cell depletion from the patient's bone marrow culture resulted in a threefold increase in ECF units. Thus, the findings in this study suggested that PRCA-associated with chronic EBV infection might be related to T-cell mediated suppression of ECF unit proliferation in the bone marrow milieu. EBV usually infects B-lymphocytes via the CD21 receptor. However, there is no active viral replication and the host cells are not killed. Thus, EBV-infected B cells can become immortalized leading to latent EBV infection of the B cell. In situ hybridization with EBER in bone marrow section can localize EBV-infected cells and detect latent EBV infection with a high degree of accuracy (19, 20). Thus, positive EBER expression in bone marrow cells of our case demonstrated latent EBV infection of bone marrow cells and this is suggested as a possible cause of PRCA.
In conclusion, although persistent anemia is a possible predictor of bone marrow involvement with lymphoma cells, PRCA should be considered in lymphoma patients. Furthermore, when there is no evidence supporting parvovirus B19 infection as a cause of PRCA, the presence of EBV infection should be evaluated. This is the first report of the occurrence of PRCA associated with latent EBV infection in a patient with recurrent diffuse large B cell lymphoma.
Figures and Tables
 | Fig. 1Bone marrow aspirate smear (Wright-Giemsa stain, ×400). Marrow cellularity is decreased for the patient's age and severe paucity of erythroid cells is observed. However, myeloid and megakaryocytic lineage is intact. |
References
1. Lim ST, Tao M, Cheung YB, Rajan S, Mann B. Can patients with early-stage diffuse large B-cell lymphoma be treated without bone marrow biopsy? Ann Oncol. 2005. 16:215–218.

2. Arnold DM, Neame PB, Meyer RM, Soamboonsrup P, Luinstra KE, O'Hoski P, Garner J, Foley R. Autologous peripheral blood progenitor cells are a potential source of parvovirus B19 infection. Transfusion. 2005. 45:394–398.

3. Song KW, Mollee P, Patterson B, Brien W, Crump M. Pure red cell aplasia due to parvovirus following treatment with CHOP and rituximab for B-cell lymphoma. Br J Haematol. 2002. 119:125–127.

4. Egerer G, Sauerland K, Ho AD. Remarkable response to rituximab in a 72-year-old patient with refractory non-Hodgkin's lymphoma and marrow aplasia. Leuk Lymphoma. 2001. 42:551–553.

5. Daibata M, Machida H, Nemoto Y, Taguchi H. Pure red cell aplasia in a patient with trisomy X chromosome abnormality and reactivated Epstein-Barr virus infection. Int J Hematol. 2003. 77:354–358.
6. Sharma VR, Fleming DR, Slone SP. Pure red cell aplasia due to parvovirus B19 in a patient treated with rituximab. Blood. 2000. 96:1184–1186.

7. Fink U, Emmerich B, Rastetter J. Simultaneous occurrence of pure red cell aplasia and malignant lymphoma. Med Klin. 1977. 72:1043–1047.
8. Hunt FA, Lander CM. Successful use of combination chemotherapy in pure red cell aplasia associated with malignant lymphoma, histiocytic type. Aust N Z J Med. 1975. 5:469–471.

9. Kiykim AA, Arici M, Altun B, Erdem Y, Yasavul U, Turgan C, Caglar S. Pure red cell aplasia preceding malignant lymphoma in a renal transplant patient. Nephron. 2002. 92:232–234.

10. Sudhoff T, Aul C, Kretschmer S, Sohngen D, Runde V. Severe anemia requiring transfusion in the early stage of low-grade malignant non-Hodgkin's lymphoma. Internist (Berl). 1994. 35:476–479.
11. Suzuki A, Takahashi T, Taniguchi A, Kotake C, Seo T, Toda T, Kobayashi K, Tsukamoto N, Fukumoto M. Pure red cell aplasia associated with non-Hodgkin's lymphoma and hemolytic anemia. Jpn J Clin Oncol. 1991. 21:384–387.
12. Zeidman A, Fradin Z, Barac Y, Bendayan D, Mittelman M, Orlin J. Splenic lymphoma presenting as warm autoimmune hemolytic anemia associated with pure red cell aplasia. Vox Sang. 2000. 78:126–129.

13. Katayama H, Takeuchi M, Yoshino T, Munemasa M, Tada A, Soda R, Takahashi K. Epstein-Barr virus associated diffuse large B-cell lymphoma complicated by autoimmune hemolytic anemia and pure red cell aplasia. Leuk Lymphoma. 2001. 42:539–542.

14. Djaldetti M, Blay A, Bergman M, Salman H, Bessler H. Pure red cell aplasia--a rare disease with multiple causes. Biomed Pharmacother. 2003. 57:326–332.

15. Chim CS, Ma ES, Loong F, Kwong YL. Diagnostic cues for natural killer cell lymphoma: primary nodal presentation and the role of in situ hybridisation for Epstein-Barr virus encoded early small RNA in detecting occult bone marrow involvement. J Clin Pathol. 2005. 58:443–445.

16. Kuramoto K, Oda K, Katsutani S, Fujii T, Abe K, Imamura N, Kimura A. Acquired pure red cell aplasia associated with relapsed non-Hodgkin's lymphoma: a case report-improvement of PRCA after acute hepatitis. Rinsho Ketsueki. 1998. 39:290–296.
17. Alter R, Joshi SS, Verdirame JD, Weisenburger DD. Pure red cell aplasia associated with B cell lymphoma: demonstration of bone marrow colony inhibition by serum immunoglobulin. Leuk Res. 1990. 14:279–286.

18. Socinski MA, Ershler WB, Tosato G, Blaese RM. Pure red blood cell aplasia associated with chronic Epstein-Barr virus infection: evidence for T cell-mediated suppression of erythroid colony forming units. J Lab Clin Med. 1984. 104:995–1006.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download