Abstract
The aims of this study were to analyze lymphocyte and eosinophil counts in consecutive peripheral blood samples taken during immunotherapy for metastatic renal cell carcinoma (mRCC) and to correlate the findings with objective response and survival. A total of 40 patients with mRCC who received immunotherapy with interleukin-2, interferon-α, and 5-fluorouracil were analyzed. Objective responses were observed in 14 patients, including 2 (5%) who showed a complete response (CR) and 12 (30%) who showed a partial response (PR). Eleven patients (27%) achieved stable disease (SD), and 15 patients (38%) had progressive disease (PD). Changes from baseline in the total lymphocyte counts were significantly higher in the responding patients (CR+PR+SD) than in the non-responding patients (PD) (p=0.017), but no difference was seen in the total eosinophil counts (p=0.275). Univariate analysis identified the Eastern Cooperative Oncology Group (ECOG) performance status (p=0.017), the presence of a primary renal tumor (p<0.001) and the peripheral lymphocyte counts at week 4 (p=0.034) as prognostic factors, but a low ECOG performance status (p=0.003) and the presence of a primary renal tumor (p=0.001) were identified as independent poor prognostic factors by multivariate analysis. This study provides further evidence that changes in blood lymphocyte counts may serve as an objective indicator of objective responses.
Renal cell carcinoma is characterized by a lack of early warning signs, resulting in a high proportion of metastasis at diagnosis. Relapse occurs in 30% to 50% of patients with completely resected renal cell carcinoma after a radical nephrectomy. Metastatic renal cell carcinoma (mRCC) is a disease with a poor prognosis and a 5-yr survival rate of less than 10% and is resistant to chemotherapy or radiotherapy (1).
Many immunotherapy protocols have been investigated since Rosenberg and colleagues discovered the clinical efficacy of high-dose bolus interleukin-2 (IL-2) in the treatment of patients with mRCC (2). With an overall response rate of approximately 20% and a durable complete response, the use of high-dose bolus IL-2 has been the best treatment for mRCC. Thus, it remained as the only U.S. Food and Drug Administration-approved drug for the treatment of metastatic renal cancer for more than a decade before the introduction of new drugs (3). However, some investigators have encountered significant multi-system toxicities resulting in treatment-related mortality, and consequently, its application has been limited to the highly selected patients treated at specialized centers (4).
The pronounced toxicities of high-dose bolus IL-2 treatment prompted the development of regimens with subcutaneous injections of IL-2. In addition, attempts were also made to improve treatment efficacy by adding interferon-α (IFN-α) and combinations of low-dose IL-2 and other chemotherapeutic agents (5-8).
Given the toxicity and expense, treatment should be limited to patients most likely to benefit from immunotherapy. Therefore, many groups have attempted to determine the immunologic prognostic factors as well as to establish clinical prognostic factors for patients with mRCC who receive immunotherapy (9-12).
It is believed that antitumor effects of IL-2 are due to several mechanisms: it stimulates the generation of natural killer (NK) cells; it enhances not only the cytotoxic activities of T cells but also the T-helper cells and eosinophils (13-15). IL-2 based immunotherapy results in varying degrees of lymphocytosis and eosinophilia in each patient.
The aims of the present study were to evaluate the clinical effectiveness of an IL-2, IFN-α, and 5-fluorouracil (5-FU) combination immunotherapy regimen and to correlate the objective response and survival with the changes in the blood lymphocyte and eosinophil counts during treatment.
From August 2001 to July 2006, 40 patients with histologically confirmed and measurable progressive mRCC were recruited for this study. Patient assessment at entry into the study consisted of a clinical evaluation, a complete blood cell count, blood chemistry studies, urinary status, radionuclide bone scan, abdominal, thoracic and cranial computerized tomography (CT), and electrocardiography. Of these patients, nephrectomy was performed in 37 patients before treatment with immunotherapy. Three patients did not wish to undergo surgery and embolization was performed following the biopsy.
The eligibility criteria included an Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1, a life expectancy of at least 3 months, adequate blood counts (hemoglobin greater than 10 g/dL, a white blood cell count greater than 4,000/mL and a platelet count greater than 100,000/mL), adequate renal and hepatic functions (serum creatinine 1.4 mg/dL or less, serum total bilirubin 1.2 mg/dL or less, and serum alanine aminotransferase 40 IU/L or less), and adequate cardiac and pulmonary function. Exclusion criteria included cardiovascular disease, hematopoietic, pulmonary, hepatic or renal dysfunction, ECOG performance status >1, active infection, autoimmune disease, HIV and hepatitis, concomitant therapy with drugs influencing immunity, and prior malignancies or brain metastases. All patients provided written, informed consent before study entry.
Immunotherapy was given with the initial 4 weeks consisting of treatment with subcutaneous IL-2 (weeks 1 and 4: 20×106 U/m2 on day 1, 3 and 5; weeks 2 and 3: 5×106 U/m2 on days 1, 3 and 5) and treatment with subcutaneous IFN-α (weeks 1 and 4: 6×106 U/m2 on day 1; weeks 2 and 3: 6×106 U/m2 on days 1, 3 and 5) injections, followed by 4 weeks of injections of subcutaneous IFN-α (weeks 5 to 8: 9×106 U/m2 on days 1, 3 and 5) and intravenous bolus injections of 5-FU (weeks 5 to 8: 750 mg/m2 on day 1) (16). The doses in weeks 1 and 4 were administered on an inpatient basis, with the rest of the treatment administered on an outpatient basis, except in cases of excessive toxicity.
Blood samples were obtained at baseline and on day 6 of every week throughout the treatment. Total and differential white blood cell counts were determined for all patients.
Patients were assessed by radiological evaluation or by physical measurement of all sites of disease following the completion of the immunotherapy regimen. The clinical response was evaluated according to the World Health Organization (WHO) criteria (17). After immunotherapy, metastasectomy was considered for patients with residual disease and who presented with solitary or a few respectable metastases with an acceptable performance status. Response duration was measured from the first observation, and time to survival was counted from the beginning of treatment.
Systemic toxicity of the treatment regimen was determined every week using a grading system according to the WHO classification, namely blood cell count and serum biochemical tests of hepatic and renal function (17). Thyroid stimulating hormone (TSH), triiodothyronine (T3), thyroxine (T4), and human anti-thyroid antibodies were assayed in all patients before and after immunotherapy to quantify possible adverse effects on thyroid function.
The primary end-points of the study were therapeutic response and overall survival after immunotherapy. The absolute number of blood lymphocyte and eosinophil counts were analyzed as the dependent variables in a general linear model repeated measures methods to evaluate the associations of these variables and the clinical response following immunotherapy. To evaluate the predictive value of measured blood lymphocyte counts at each time (baseline and weeks 1 to 4) for therapeutic response, receiver operating characteristic (ROC) curves were generated and areas under the curves (AUC) were calculated for the measured lymphocyte counts at each time. Kaplan-Meier survival curves for overall survival were generated, and the log-rank test was used to compare survival according to the variable. The Cox proportional hazards regression model was used to estimate the relative importance of the variables. For all statistical analyses p<0.05 was considered significant.
Demographic and clinical characteristics are summarized in Table 1. The median age of the 40 patients was 56 yr (range, 36-72). All patients included in this study showed a clear cell histology, and sarcomatoid differentiation was seen in 2 patients. The overall response rate was 35% (2 complete responses and 12 partial responses), stable disease was achieved in 11 (27%) patients, and progressive disease occurred in 15 (38%). Complete responses were found only in patients with a single lung metastasis, and the duration of complete remission was 33 and 36 months, respectively.
Total lymphocyte counts were significantly higher in responding patients (CR+PR+SD) than in non-responding patients (PD) (Fig. 1). No difference was seen in the total eosinophil counts (Fig. 2). Among the serial blood lymphocyte counts at baseline and for each week, the total lymphocyte count at week 4 was the most predictive of therapeutic response. The ROC curve for the lymphocyte count at week 4 demonstrated the most significant predictive ability (AUC 0.84, 95% confidence interval [CI] 0.76 to 0.91). The AUC for the baseline, and weeks 1, 2, and 3 were 0.68 (95% CI 0.60 to 0.77), 0.49 (95% CI 0.40 to 0.59), 0.74 (95% CI 0.66 to 0.82), and 0.68 (95% CI 0.60 to 0.77), respectively.
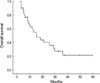
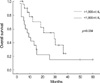
The median follow-up period after the start of the immunotherapy was 16 months. The overall survival rate was 61% (95% CI 53% to 70%), 39% (95% CI 31% to 49%), and 27% (95% CI 18% to 36%) at 1, 2, and 3 yr, respectively, and median survival was 15 months (Fig. 3). On univariate analysis unfavorable prognostic variables for overall survival were low ECOG performance status, the presence of a primary renal tumor, and a low peripheral lymphocyte count at week 4. In patients with a lymphocyte count higher than 1,900 n/µL, the 3-yr survival rate was 36%, compared to 15% when the lymphocyte count was 1,900 n/µL or less (Table 2 and Fig. 4). On multivariate analysis low ECOG performance status and the presence of a primary renal tumor were associated with decreased overall survival (Table 3).
The most common side effects were flu-like symptoms, fatigue, mucositis, diarrhea, vesicle, changes in leukocyte, hemoglobin, and platelet levels, and nausea during the treatment. Table 4 shows a detailed description of systemic toxicities and their severity. In all patients treatment-related systemic toxicity resolved after the end of the therapeutic regimen. No patient had grade 4 toxicity, and there were no treatment-related deaths.
Because of the significant toxicity and its high cost, it is very important to select patients with mRCC who may benefit mostly from immunotherapy prior to treatment. With regard to the histologic subtype, responses to immunotherapy are most frequently seen in patients with renal cell carcinoma of clear cell histology. Among the clear cell subtypes, the response to IL-2 was associated with the presence of alveolar features and the absence of granular or papillary features (11). Gez and colleagues identified good performance status, absence of bone metastases, and no other concomitant comorbidity as important predictors of response in patients receiving immunochemotherapy. A prior nephrectomy had no influence on response to treatment in their study (18). Recent data from the Cytokine Working Group phase III trial have suggested that patients with bone or liver metastasis or a primary tumor in place might little benefit minimally from a lower-dose IL-2 regimen. Based on their study, it was believed that high-dose IL-2 therapy was superior to a low-dose IL-2 regimen in selected patients with an access to such treatment (19). In our study, ECOG performance status and a prior nephrectomy were independent predictors of survival in patients receiving immunotherapy.
The results from the present study demonstrated a higher response rate of 35% and three-year survival rate of 27% for this regimen, which are similar to those described by other investigators (18, 20). There may be a possible explanation for the satisfactory results of this study. First of all, the majority of patients had an excellent ECOG performance status (0 to 1). In addition, all of the patients had a clear cell histology, which was regarded as a good predictor of response to IL-2 therapy, and a large number of patients had undergone a prior nephrectomy. Even though a higher response rate was observed in the present study, the long-term survival of patients was poor. Possible explanation for poor survival is that in this study the response to treatment was assessed following the completion of the first cycle. Subsequently, many of responding patients to the first cycle of immunotherapy progressed eventually.
Considering the anti-tumor activity of host immune cells, it has been speculated that the host immune system plays an important role in immunotherapy for the treatment of patients with mRCC. Most recently, Donskov and colleagues identified clinical and immunologic independent predictors of survival for patients with mRCC receiving IL-2. In this study, lactate dehydrogenase, lymph node metastases, hemoglobin, Karnofsky performance status, and bone metastases were identified as clinical independent prognostic factors. Furthermore, a high blood neutrophil count, the presence of intratumoral neutrophils, and a low intratumoral CD57+ NK cell count were also identified as independent poor prognostic immunologic factors (12).
After the administration of IL-2, the number of lymphocytes in the peripheral blood increases following transient lymphocytopenia for about 36 to 48 hr. The degree of lymphocytosis is variable (21). It is known that a greater lymphocyte increase has been observed after IL-2 therapy in patients with mRCC who achieve an objective response, as seen in several studies. Furthermore, elevated baseline inflammatory markers prevent IL-2-induced lymphocytosis and results in tumor progression (22). With regard to the role of lymphocytosis in predicting the response to IL-2, a significant positive correlation between the absolute number of peripheral blood lymphocytes after 2 weeks of treatment and an objective response was demonstrated (9). Similarly, Fumagalli and colleagues also found that the baseline and the maximum lymphocyte count on therapy were associated with overall survival (10).
Our understanding of the mechanism by which IL-2 mediates its antineoplastic actions is incomplete. Published studies have demonstrated an increased number of CD3+ T cells and CD57+ NK cells in responding patients during immunotherapy. Moreover, these studies have found that intratumoral CD3+, CD8+ T cells and CD57+ NK cells were associated with an objective response (9, 23).
In our study, ROC analysis showed that the total lymphocyte counts at weeks 2 and 4 were significantly more predictive of a therapeutic response. Because a relatively high-dose of IL-2 (20×106 U/m2) was administrated at weeks 1 and 4, it is possible that the difference in the predictive value is related to differences in the administrated dose of IL-2. Transient lymphocytopenia may be considered as a possible cause of the low predictive value of the lymphocyte count at week 1. However, the multivariate Cox model using a cutoff for a total lymphocyte count at week 4 of 1,900 n/µL failed to predict the survival.
It has been reported that blood eosinophil counts as well as lymphocyte counts significantly increased after immunotherapy with low-dose IL-2 and IFN-α for mRCC (15). So far, an exact role of eosinophil in immunotherapy using IL-2 remains unclear. Rodgers and colleagues studied the properties of eosinophils from 16 patients with renal cell carcinoma who received low-dose IL-2 therapy, and in their study, the maximum eosinophil count achieved during IL-2 therapy is of prognostic significance (24). Moroni and colleagues also showed that a large eosinophil number predicts the failure of IL-2 treatment (25). In our study, the absolute number of eosinophils in peripheral blood increased following immunotherapy in both responding and non-responding patients. Although the degree of increase showed a trend that it was higher in the responding patients, the difference was not statistically significant.
Several investigators have attempted to confirm the relationship between changes in blood lymphocyte count and response to immunotherapy. However, the limitations of previous studies were the use of heterogeneous immunotherapy protocols and static analysis on the count at a single point of time (10, 22). In agreement with previous reports, our study showed that the blood total lymphocyte count had an important role in predicting the responses to low-dose IL-2 therapy. On the other hand, in contrast to their studies, all patients included in our study were homogeneous with regard to the immunotherapy protocol, and we analyzed the dynamic change of blood lymphocyte and eosinophil counts.
A lymphocyte subset was not determined in our study. Thus, it is difficult to know which of the lymphocyte subsets correlates with the response to immunotherapy. However, if we can easily predict the responding patients from the changes in their blood lymphocyte counts, this will be a useful way to sub-classify patients treated with immunotherapy because of its non-invasiveness. In addition, we verified that the degree of increase in the blood eosinophil counts did not differ between the responding and non-responding patients during immunotherapy. Further studies are needed to confirm whether the changes in the blood lymphocyte count during immunotherapy are associated with long-term survival.
In summary, we observed a significant increase in blood lymphocyte and eosinophil counts during immunotherapy for mRCC. Total lymphocyte counts were significantly higher in responding patients than in non-responding patients, but no difference was observed in the total eosinophil counts. This study provides further evidence that changes in blood lymphocyte counts may serve as an objective indicator of the objective responses when treating patients with mRCC using immunotherapy.
Figures and Tables
Fig. 3
Overall survival of the 40 patients with metastatic renal cell carcinoma treated with immunotherapy.
References
1. Bukowski RM. Natural history and therapy of metastatic renal cell carcinoma: the role of interleukin-2. Cancer. 1997. 80:1198–1220.
2. Rosenberg SA, Lotze MT, Muul LM, Leitman S, Chang AE, Ettinghausen SE, Matory YL, Skibber JM, Shiloni E, Vetto JT. Observations on the systemic administration of autologous lymphokine-activated killer cells and recombinant interleukin-2 to patients with metastatic cancer. N Engl J Med. 1985. 313:1485–1492.

3. Rosenberg SA, Yang JC, White DE, Steinberg SM. Durability of complete responses in patients with metastatic cancer treated with high-dose interleukin-2: identification of the antigens mediating response. Ann Surg. 1998. 228:307–319.

4. Parkinson DR, Abrams JS, Wiernik PH, Rayner AA, Margolin KA, Van Echo DA, Sznol M, Dutcher JP, Aronson FR, Doroshow JH. Interleukin-2 therapy in patients with metastatic malignant melanoma: a phase II study. J Clin Oncol. 1990. 8:1650–1656.

5. Atzpodien J, Lopez Hanninen E, Kirchner H, Bodenstein H, Pfreundschuh M, Rebmann U, Metzner B, Illiger HJ, Jakse G, Niesel T. Multiinstitutional home-therapy trial of recombinant human interleukin-2 and interferon alfa-2 in progressive metastatic renal cell carcinoma. J Clin Oncol. 1995. 13:497–501.

6. Negrier S, Escudier B, Lasset C, Douillard JY, Savary J, Chevreau C, Ravaud A, Mercatello A, Peny J, Mousseau M, Philip T, Tursz T. Groupe Francais d'Immunothérapie. Recombinant human interleukin-2, recombinant human interferon alfa-2a, or both in metastatic renal-cell carcinoma. N Engl J Med. 1998. 338:1272–1278.

7. Atzpodien J, Hoffmann R, Franzke M, Stief C, Wandert T, Reitz M. Thirteen-year, long-term efficacy of interferon 2alpha and interleukin 2-based home therapy in patients with advanced renal cell carcinoma. Cancer. 2002. 95:1045–1050.
8. Yang JC, Sherry RM, Steinberg SM, Topalian SL, Schwartzentruber DJ, Hwu P, Seipp CA, Rogers-Freezer L, Morton KE, White DE, Liewehr DJ, Merino MJ, Rosenberg SA. Randomized study of high-dose and low-dose interleukin-2 in patients with metastatic renal cancer. J Clin Oncol. 2003. 21:3127–3132.

9. Donskov F, Bennedsgaard KM, Von Der Maase H, Marcussen N, Fisker R, Jensen JJ, Naredi P, Hokland M. Intratumoural and peripheral blood lymphocyte subsets in patients with metastatic renal cell carcinoma undergoing interleukin-2 based immunotherapy: association to objective response and survival. Br J Cancer. 2002. 87:194–201.

10. Fumagalli LA, Vinke J, Hoff W, Ypma E, Brivio F, Nespoli A. Lymphocyte counts independently predict overall survival in advanced cancer patients: a biomarker for IL-2 immunotherapy. J Immunother. 2003. 26:394–402.

11. Upton MP, Parker RA, Youmans A, McDermott DF, Atkins MB. Histologic predictors of renal cell carcinoma response to interleukin-2-based therapy. J Immunother. 2005. 28:488–495.

12. Donskov F, von der Maase H. Impact of immune parameters on long-term survival in metastatic renal cell carcinoma. J Clin Oncol. 2006. 24:1997–2005.

13. Parmiani G. An explanation of the variable clinical response to interleukin 2 and LAK cells. Immunol Today. 1990. 11:113–115.

14. Forni G, Giovarelli M, Santoni A, Modesti A, Forni M. Interleukin 2 activated tumor inhibition in vivo depends on the systemic involvement of host immunoreactivity. J Immunol. 1987. 138:4033–4041.
15. Buzio C, Andrulli S, Santi R, Pavone L, Passalacqua R, Potenzoni D, Ferrozzi F, Giacosa R, Vaglio A. Long-term immunotherapy with low-dose interleukin-2 and interferon-alpha in the treatment of patients with advanced renal cell carcinoma. Cancer. 2001. 92:2286–2296.
16. Hofmockel G, Langer W, Theiss M, Gruss A, Frohmuller HG. Immunochemotherapy for metastatic renal cell carcinoma using a regimen of interleukin-2, interferon-alpha and 5-fluorouracil. J Urol. 1996. 156:18–21.

17. Miller AB, Hoogstraten B, Staquet M, Winkler A. Reporting results of cancer treatment. Cancer. 1981. 47:207–214.

18. Gez E, Rubinov R, Gaitini D, Meretyk S, Best LA, Native O, Stein A, Erlich N, Beny A, Zidan J, Haim N, Kuten A. Interleukin-2, interferon-alpha, 5-fluorouracil, and vinblastine in the treatment of metastatic renal cell carcinoma: a prospective phase II study: the experience of Rambam and Lin Medical Centers 1996-2000. Cancer. 2002. 95:1644–1649.
19. McDermott DF, Regan MM, Clark JI, Flaherty LE, Weiss GR, Logan TF, Kirkwood JM, Gordon MS, Sosman JA, Ernstoff MS, Tretter CP, Urba WJ, Smith JW, Margolin KA, Mier JW, Gollob JA, Dutcher JP, Atkins MB. Randomized phase III trial of high-dose interleukin-2 versus subcutaneous interleukin-2 and interferon in patients with metastatic renal cell carcinoma. J Clin Oncol. 2005. 23:133–141.

20. Atzpodien J, Kirchner H, Jonas U, Bergmann L, Schott H, Heynemann H, Fornara P, Loening SA, Roigas J, Muller SC, Bodenstein H, Pomer S, Metzner B, Rebmann U, Oberneder R, Siebels M, Wandert T, Puchberger T, Reitz M. Interleukin-2- and interferon alfa-2a-based immunochemotherapy in advanced renal cell carcinoma: a Prospectively Randomized Trial of the German Cooperative Renal Carcinoma Chemoimmunotherapy Group (DGCIN). J Clin Oncol. 2004. 22:1188–1194.

21. Konrad MW, Hemstreet G, Hersh EM, Mansell PW, Mertelsmann R, Kolitz JE, Bradley EC. Pharmacokinetics of recombinant interleukin 2 in humans. Cancer Res. 1990. 50:2009–2017.
22. Fumagalli L, Lissoni P, Di Felice G, Meregalli S, Valsuani G, Mengo S, Rovelli F. Pretreatment serum markers and lymphocyte response to interleukin-2 therapy. Br J Cancer. 1999. 80:407–411.

23. Donskov F, Bennedsgaard KM, Hokland M, Marcussen N, Fisker R, Madsen HH, Fode K, von der Maase H. Leukocyte orchestration in blood and tumour tissue following interleukin-2 based immunotherapy in metastatic renal cell carcinoma. Cancer Immunol Immunother. 2004. 53:729–739.

24. Rodgers S, Rees RC, Hancock BW. Changes in the phenotypic characteristics of eosinophils from patients receiving recombinant human interleukin-2 (rhIL-2) therapy. Br J Haematol. 1994. 86:746–753.

25. Moroni M, Porta C, De Amici M, Quaglini S, Cattabiani MA, Buzio C. Eosinophils and C4 predict clinical failure of combination immunotherapy with very low dose subcutaneous interleukin-2 and interferon in renal cell carcinoma patients. Haematologica. 2000. 85:298–303.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download