Abstract
This study was performed to evaluate the efficacy and toxicity of low-dose paclitaxel/cisplatin chemotherapy in patients with metastatic or recurrent gastric cancer that had failed 5-fluorouracil/platinum-based chemotherapy. Thirty-two patients with documented progression on or within 6 months after discontinuing 5-fluorouracil/platinum-based chemotherapy were enrolled. As a second-line treatment, paclitaxel (145 mg/m2) and cisplatin (60 mg/m2) was administered on day 1 every 3 weeks. Among 32 patients enrolled, 8 (25%) responded partially to paclitaxel/cisplatin, 8 (25%) had stable disease, and 14 (44%) had progressive disease. Two patients (6%) were not evaluable. The median time to progression (TTP) and overall survival for all patients were 2.9 months and 9.1 months, respectively. The most common hematologic toxicity was anemia (47%). Grade 3 neutropenia developed in three patients (9%), but no other grade 3/4 hematologic toxicity occurred. The most common non-hematologic toxicities were emesis (31%) and peripheral neuropathy (38%). Three cases (9%) of grade 3/4 emesis and 2 cases (6%) of grade 3 peripheral neuropathy developed. In conclusion, low-dose paclitaxel and cisplatin chemotherapy showed moderate activity with favorable toxicity profiles. However, relatively short TTP of this regimen warrants the development of more effective paclitaxel-based regimens other than combination with cisplatin in these patients as second-line therapies.
Despite its declining incidence in many countries, gastric cancer remains one of the most prevalent malignancies in many countries, and a major international health problem. According to statistics published in 2002, gastric cancer remained the most prevalent cancer in Korea (1). Recently, improvements in early diagnosis have increased the number of patients suitable for curative resection, but tumor recurrence is frequently observed. Moreover, many patients have metastatic disease at the time of initial diagnosis.
Cytotoxic chemotherapy has been demonstrated to be effective in the palliative management of unresectable locally advanced or metastatic gastric cancer. Randomized trials have found that cytotoxic chemotherapy is associated with improvement in overall survival (OS) and quality of life as compared with best supportive care (2-4). Until recently, 5-fluorouracil (5-FU) and platinum-based combination chemotherapy has been commonly used as first-line treatment in unresectable locally advanced or metastatic gastric cancer (5, 6). In a phase III randomized study, Kim et al. reported an overall response rate of 51% and a median OS of 9.0 months in previously untreated gastric cancer patients with 5-FU/cisplatin (FP) chemotherapy (5). However, the overall prognosis of patients failing first-line chemotherapy is poor, and although many of these patients are candidates for second-line chemotherapy at the time of first-line treatment failure, no established second-line chemotherapeutic regimen is available as yet.
Paclitaxel is an anticancer agent that promotes the formation of tubulin dimers and that inhibits microtubule depolymerization. Paclitaxel has broad spectrum antitumor activity and moderate toxicity profiles. It has shown encouraging activity as a single agent (200-225 mg/m2, every 3 weeks) in gastric cancer, with a response rate of 17-28% (7-10). Paclitaxel appears to have a schedule-dependent synergy with platinum compounds, as documented in human gastric cancer cell lines (11), and this observed synergy has led to the development of paclitaxel-platinum combination regimens in a number of solid tumors, including gastric cancer (12-16). In gastric cancer, first-line paclitaxel/cisplatin chemotherapy has shown response rates of 44-46% and median OS of 11.2-13.8 months (13, 15, 16). Although these reports are of phase II studies, treatment outcomes of paclitaxel and cisplatin chemotherapy seem to be at least similar to those of previously commonly used two- or three-drug combination regimens (FAMTX [5-FU, doxorubicin, and methotrexate] (17), ELF [etoposide, leucovorin, and 5-FU] (17), and FP [5-FU and cisplatin] (5, 17)).
We previously conducted a phase II study using low-dose paclitaxel 145 mg/m2 plus cisplatin 60 mg/m2 on day 1 every 3 weeks in non-small cell lung cancer. In that study, this regimen was feasible and seemed to have reduced toxicities and maintain efficacy compared with previously reported other regimens (18). This previous experience and convenience of the scheduling in the outpatient setting prompted us to select the same regimen in gastric cancer. Based on in vitro synergistic effects (11) and feasibility of low-dose paclitaxel and cisplatin regimen (18), a phase II study was performed in gastric cancer patients that had failed previous 5-FU/platinum chemotherapy at three institutions.
To be eligible for this study, patients were required to have: histologically confirmed adenocarcinoma of the stomach (except carcinomas of the esophagogastric junction) that progressed while receiving, or within 6 months after the discontinuation of prior 5-FU/platinum-based chemotherapy used as an adjuvant or palliative treatment. In addition, patients were required to be 18-75 yr old with a life expectancy of >3 months and have an Eastern Cooperative Oncology Group (ECOG) performance status of 0 to 2, adequate hematologic counts (absolute neutrophil count [ANC] ≥1.5×109/L and platelet count ≥100×109/L), and laboratory results within the following limits (serum bilirubin ≤1.25×upper normal limit [UNL], serum aspartate aminotransferase [AST] and alanine aminotransferase [ALT] ≤2.5×UNL, serum alkaline phosphatase ≤5.0×UNL [unless bone metastasis was present in the absence of any liver disease]) and renal function (serum creatinine ≤1.5 mg/dL). All patients were required to have at least one measurable disease (defined as a mass with demarcated dimensions by computed tomography [CT], routine chest radiography, or by physical examination).
Patients were deemed ineligible if they had brain metastasis or a history of a prior or a concomitant malignancy, except for curatively treated non-melanoma skin cancer or in situ cervical cancer. Pre-existing motor or sensory neurologic symptoms of ≥grade 2 according to the National Cancer Institute Common Toxicity Criteria (NCI-CTC) were not permitted, nor were active infections or other serious underlying medical conditions that might have impaired the ability of a patient to receive protocol treatment. All patients provided written informed consent, and this study was approved by institutional review boards.
Hydrocortisone (100 mg), pheniramine maleate, and famotidine were administered intravenously (i.v.) 30 min before paclitaxel for hypersensitivity prophylaxis. The patients then received paclitaxel 145 mg/m2 as a 3-hr i.v. infusion, followed by cisplatin 60 mg/m2 as a 15-min i.v. infusion with a standard hydration method on day 1. All patients received adequate antiemetic therapy prior to chemotherapy. Treatment was administered on an outpatient basis and repeated 3 weekly, provided that patients had recovered from toxic effects. This combination chemotherapy was continued for up to 6 cycles in the absence of disease progression or unacceptable toxicity. Granulocyte colony-stimulating factor (G-CSF) was not routinely administered.
Physical examination, complete blood counts and biochemical tests were carried out before each cycle of therapy. Tumors were measured every 2 cycles by imaging studies. Response was assessed using WHO criteria. Complete response (CR) was defined as the disappearance of all clinical evidence of tumor for a period of at least 4 weeks. Partial response (PR) was defined as a sustained ≥50% decrease in bidimensional tumor measurements for a period of at least 4 weeks, without the appearance of any new lesions or the progression of any existing lesion. Progressive disease (PD) was defined as the development of any new lesion or a greater than 25% increase in the sum of the products of all measurable lesions. Stable disease (SD) was defined as a tumor response that did not meet the above CR, PR or PD criteria.
Toxicities were evaluated using NCI-CTC (version 2.0) before each treatment. Dose modifications and treatment delays were performed as necessary according to the extent of hematological and non-hematological toxicities. Drug doses were reduced by 25% in case of grade 4 neutropenia (ANC <0.5×109/L), grade 4 thrombocytopenia (platelet count <25×109/L) or febrile neutropenic fever. Additional 25% reduction of both drug doses was indicated for recurrent febrile neutropenic fever, grade 4 neutropenia or thrombocytopenia. For patients who experienced grade 1 nephrotoxicity, grade 2/3 peripheral neuropathy or other severe non-hematologic toxicities of NCI-CTC ≥grade 3, drug doses were reduced by 25%. If a patient had ≥grade 2 non-hematological toxicities during chemotherapy (except alopecia), chemotherapy was withheld for a minimum of 1 week until the patient had improved to ≤grade 1, at which time chemotherapy was re-instituted. However, if hematologic or non-hematological toxicities did not improve to ≤grade 1 after 3 weeks, the patient was removed from the study. Both chemotherapeutic drugs were discontinued in the event of transitory ≥grade 2 nephrotoxicity, grade 4 neuropathy, and if severe toxicity recurred despite dose reduction.
The primary endpoint of this trial was the response rate to low-dose paclitaxel/cisplatin treatment. TTP and OS were secondary end points. TTP was calculated from the first day of chemotherapy to the date of disease progression, and OS was calculated from the first day of chemotherapy until death.
This trial was designed to detect a response rate of 20% as compared to a minimal, clinically meaningful response rate of 5%. An optimal Simon two-step design was used (19), with a power of 80% to accept the hypothesis and a 5% significance to reject the hypothesis. Ten patients were initially recruited, with the intention that had no responses been observed, the trial would have been discontinued. However, it was planned to continue with the trial and to recruit a total of 29 patients with measurable disease, if at least one of these 10 patients showed an objective response. Allowing for a follow-up loss rate of 10%, a total sample size of 32 patients was necessary. Analyses of TTP and OS curves were performed using the Kaplan-Meier method.
From October 2002 to January 2005, 32 patients of median age 60.5 yr (29-74 yr) were enrolled from three institutions. Patient characteristics are given in Table 1. The majority of the study population was male (84%, 27 of 32). Eleven patients (34%) had an ECOG performance status of 2. Twenty-four patients (75%) had previously received 5-FU/cisplatin (FP) chemotherapy and 8 patients (25%) 5-FU/leucovorin/oxaliplatin (FOLFOX) chemotherapy. Of these patients, 6 (19%) received FP chemotherapy in an adjuvant setting. At the time of enrollment, 23 patients (72%) had progressive disease during prior 5-FU/platinum-based chemotherapy and 9 (28%) progressed within 6 months of discontinuing previous chemotherapy. All patients had measurable tumor lesions. Lymph nodes (69%), liver (44%) and peritoneum (41%) were the most common metastatic sites.
Of the 32 patients who received second-line chemotherapy, 2 patients (6%) were non-evaluable for response due to early drop-out after the first cycle; one patient withdrew consent and received further treatment at other hospital, and the other patient refused further chemotherapy due to treatment-related toxicity (severe emesis).
A total of 108 treatment cycles were delivered, with a median of 3 cycles per patient (range, 1 to 6). Seven (22%) of the patients received the planned 6 cycles of chemotherapy. Treatment was discontinued prematurely in two patients because of chemotherapy-associated toxicities; one patient, as mentioned above, rejected further treatment due to severe emesis after the first cycle of chemotherapy, and the other patient could not receive further chemotherapy because of severe peripheral neuropathy. Relative dose intensities were calculated for all patients and drugs according to the method described by Hryniuk (20). The calculated mean relative dose intensities of paclitaxel and cisplatin were 93% and 93%, respectively.
Of the 32 patients who received second-line combination chemotherapy, 2 patients (6%) were not evaluable for response. By intent-to-treat analysis, the overall response rate was 25% (95% confidence interval [CI]: 13-42%) and 8 of the 32 patients achieved PR. Eight patients (25%) had SD, and 14 patients (44%) tumor progression. Seven of 24 patients in the FP group (29%) and 1 of 8 in the FOLFOX group (13%) responded to second-line chemotherapy.
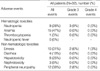
Toxicities were evaluated in all 32 patients, and results are summarized in Table 2. The most common hematologic toxicity was anemia (47%). Of the grade 3 or 4 hematologic toxicities, 3 cases (9%) of grade 3 neutropenia occurred. No grade 3 or 4 anemia or thrombocytopenia was observed, and no patient experienced febrile neutropenia.
Non-hematologic toxicities consisted mainly of emesis and peripheral neuropathy. Nausea and vomiting occurred in 10 patients (31%) and was generally mild or moderate. Grade 3 or 4 emesis was noted in 3 patients (9%). Twelve patients (38%) developed peripheral neuropathy, which was generally mild, but two patients (6%) experienced severe (grade 3) peripheral neuropathy. Liver function test abnormalities were observed in 8 patients (25%), but all were mild and transient. Mild diarrhea and nephrotoxicity were noted in 4 (13%) and 3 patients (9%), respectively. No patient experienced infusion-related hypersensitivity during chemotherapy. Two patients dropped out of the study because of adverse events after chemotherapy. One patient rejected further treatment due to severe emesis, and the other could not receive further chemotherapy due to severe peripheral neuropathy. No treatment-related death occurred.
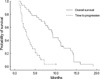
The median follow-up duration was 9.3 months. Median TTP after the initiation of low-dose paclitaxel/cisplatin chemotherapy was 2.9 months (95% CI: 1.8-4.0 months) (Fig. 1), and the median TTP of responders (N=8) was 4.3 months (95% CI: 3.1-5.5 months). After paclitaxel/cisplatin chemotherapy failure, 23 patients received third-line chemotherapy. As of reference date of final analysis (20 December 2005), 31 patients (97%) were found to have died of their disease. The median OS of all patients was 9.1 months (95% CI: 7.7-10.5 months) (Fig. 1), and the median OS of responders (N=8) was 11.2 months (95% CI: 6.2-16.2 months).
The median survival of gastric cancer patients administered palliative chemotherapy has been reported to be longer than that of patients receiving best supportive care (2-4). In addition to the significant survival advantage associated with chemotherapy, the patients that received therapy were observed to have a more stable quality of life. However, the clinical benefit of salvage chemotherapy has not been proven, and no randomized controlled trial data suggest a benefit for second-line chemotherapy. Some studies have suggested that patients who respond to second-line chemotherapy survive longer than non-responders and that symptomatic benefit may be obtained from second-line therapy (8, 21), but other studies have failed to demonstrate the effectiveness of second-line treatment. These different results concerning the benefits of second-line chemotherapy in gastric cancer may be attributable to variability in responsiveness to first-line chemotherapy, and to the chemotherapeutics previously used.
Paclitaxel has a cytotoxic mechanism that is different from those of older chemotherapeutic agents such as 5-FU and platinum. It has been reported that paclitaxel alone attained response rates of 20-22% in patients with gastric carcinoma refractory to prior chemotherapy (8, 22). In previous reports on the dose-response effect of paclitaxel, no obvious benefit was observed for high-dose paclitaxel in various solid tumors, including head and neck (23), lung (24), breast (25, 26), and ovary cancer (27, 28). Moreover, it has been consistently reported that higher-dose paclitaxel has no additional survival benefit in various solid tumors. We previously performed phase II study using low-dose paclitaxel (145 mg/m2) and cisplatin (60 mg/m2) on day 1 every 3 weeks as first-line chemotherapy for gastric cancer. The overall response rate was 44% and median TTP and OS were 4.7 and 12.1 months, respectively. These results also suggested a similar efficacy for low- and high-dose paclitaxel-containing regimens in advanced gastric cancer patients (16). Paclitaxel binding sites on β-tubulin were found to be saturated at the paclitaxel plasma steady-state concentrations achieved by doses ≥135 mg/m2 (24-hr infusion), and cytotoxicity was observed to plateau in vitro on increasing the paclitaxel concentration (29). These observations may explain the lack of additional survival benefit in solid tumors treated with higher doses of paclitaxel.
The present study was performed using a low-dose paclitaxel/cisplatin regimen as a second-line treatment for gastric cancer patients who had failed previous 5-FU/platinum-based chemotherapies at three institutions. To our knowledge, this is the first study to report the efficacy of paclitaxel/cisplatin as second-line chemotherapy in gastric cancer. In the present study, toxicities were generally mild. The major toxicities were anemia, peripheral neuropathy, emesis, and neutropenia, which are similar to those previously reported for higher-dose paclitaxel/platinum-containing regimens. However, grade 3 or 4 neutropenia developed only in 9% of patients, which is substantially lower than those reported for higher-dose paclitaxel/platinum-containing regimens (Table 3). Peripheral neuropathy is the most troublesome toxicity for patients receiving paclitaxel-containing regimens, and paclitaxel dose intensity is related to the occurrence of severe neurotoxicities, especially when combined with cisplatin, therefore cisplatin is commonly replaced with carboplatin. However, the paclitaxel/carboplatin regimen causes more myelosuppression. In this study, grade 3 or 4 neuropathy developed in 6% of patients receiving low-dose paclitaxel and cisplatin as a second-line treatment, though 38% developed peripheral neuropathy. This frequency of peripheral neuropathy for low-dose paclitaxel/cisplatin regimen is similar to those of paclitaxel and carboplatin regimens, which showed 50-85% peripheral neuropathy of all grades and 0-8% grade 3 or 4 peripheral neuropathy, respectively (14, 21, 30). Moreover, compared with docetaxel-containing regimens, the low-dose paclitaxel/cisplatin combination appears to have a favorable toxicity profile, particularly with respect to myelosuppression.
We observed that this combination therapy produced 25% response rate, which is similar to 22-28% in previously treated gastric cancer patients who received higher doses of paclitaxel (175-200 mg/m2) and carboplatin as a second-line therapy (21, 30). TTP was shorter than expected (median, 2.9 months), which may be due to the patients' prior chemotherapy regimens, all of which included platinum-based agents. The median OS for all patients was 9.1 months from the start of second-line chemotherapy, despite a short TTP, which is probably explained in part by the administration of additional salvage chemotherapy (i.e., third-line treatment) in 23 patients (72%). Although the role of third-line chemotherapy is still controversial in gastric cancer, our results suggest that third-line chemotherapy may result in substantial prolongation of survival and warrant further prospective evaluation.
In conclusion, low-dose paclitaxel and cisplatin chemotherapy showed moderate activity with favorable toxicity profiles as a second-line treatment for patients with advanced gastric cancer who had failed 5-FU and platinum-based chemotherapy. However, relatively short TTP of this regimen warrants the development of more effective paclitaxel-based regimens other than combination with cisplatin in these patients as potential second-line therapies.
Figures and Tables
References
1. Shin HR, Ahn YO, Bae JM, Shin MH, Lee DH, Lee CW, Ohrr HC, Ahn DH, Ferlay J, Parkin DM, Oh DK, Park JG. Cancer incidence in Korea. Cancer Res Treat. 2002. 34:405–408.

2. Murad AM, Santiago FF, Petroianu A, Rocha PR, Rodrigues MA, Rausch M. Modified therapy with 5-fluorouracil, doxorubicin, and methotrexate in advanced gastric cancer. Cancer. 1993. 72:37–41.

3. Pyrhonen S, Kuitunen T, Nyandoto P, Kouri M. Randomised comparison of fluorouracil, epidoxorubicin and methotrexate (FEMTX) plus supportive care with supportive care alone in patients with non-resectable gastric cancer. Br J Cancer. 1995. 71:587–591.

4. Glimelius B, Ekstrom K, Hoffman K, Graf W, Sjoden PO, Haglund U, Svensson C, Enander LK, Linne T, Sellstrom H, Heuman R. Randomized comparison between chemotherapy plus best supportive care with best supportive care in advanced gastric cancer. Ann Oncol. 1997. 8:163–168.

5. Kim NK, Park YS, Heo DS, Suh C, Kim SY, Park KC, Kang YK, Shin DB, Kim HT, Kim HJ, Kang WK, Suh CI, Bang YJ. A phase III randomized study of 5-fluorouracil and cisplatin versus 5-fluorouracil, doxorubicin, and mitomycin C versus 5-fluorouracil alone in the treatment of advanced gastric cancer. Cancer. 1993. 71:3813–3818.

6. Min YJ, Bang SJ, Shin JW, Kim DH, Park JH, Kim GY, Ko BK, Choi DH, Cho HR. Combination chemotherapy with 5-fluorouracil and heptaplatin as first-line treatment in patients with advanced gastric cancer. J Korean Med Sci. 2004. 19:369–373.

7. Ajani JA, Fairweather J, Dumas P, Patt YZ, Pazdur R, Mansfield PF. Phase II study of Taxol in patients with advanced gastric carcinoma. Cancer J Sci Am. 1998. 4:269–274.
8. Cascinu S, Graziano F, Cardarelli N, Marcellini M, Giordani P, Menichetti ET, Catalano G. Phase II study of paclitaxel in pretreated advanced gastric cancer. Anticancer Drugs. 1998. 9:307–310.

9. Yamada Y, Shirao K, Ohtsu A, Boku N, Hyodo I, Saitoh H, Miyata Y, Taguchi T. Phase II trial of paclitaxel by three-hour infusion for advanced gastric cancer with short premedication for prophylaxis against paclitaxel-associated hypersensitivity reactions. Ann Oncol. 2001. 12:1133–1137.

10. Yamaguchi K, Tada M, Horikoshi N, Otani T, Takiuchi H, Saitoh S, Kanamaru R, Kasai Y, Koizumi W, Sakata Y, Taguchi T. Phase II study of paclitaxel with 3-h infusion in patients with advanced gastric cancer. Gastric Cancer. 2002. 5:90–95.

11. Vanhoefer U, Harstrick A, Wilke H, Schleucher N, Walles H, Schroder J, Seeber S. Schedule-dependent antagonism of paclitaxel and cisplatin in human gastric and ovarian carcinoma cell lines in vitro. Eur J Cancer. 1995. 31A:92–97.

12. Kim YH, Shin SW, Kim BS, Kim JH, Kim JG, Mok YJ, Kim CS, Rhyu HS, Hyun JH, Kim JS. Paclitaxel, 5-fluorouracil, and cisplatin combination chemotherapy for the treatment of advanced gastric carcinoma. Cancer. 1999. 85:295–301.

13. Kornek GV, Raderer M, Schull B, Fiebiger W, Gedlicka C, Lenauer A, Depisch D, Schneeweiss B, Lang F, Scheithauer W. Effective combination chemotherapy with paclitaxel and cisplatin with or without human granulocyte colony-stimulating factor and/or erythropoietin in patients with advanced gastric cancer. Br J Cancer. 2002. 86:1858–1863.

14. Gadgeel SM, Shields AF, Heilbrun LK, Labadidi S, Zalupski M, Chaplen R, Philip PA. Phase II study of paclitaxel and carboplatin in patients with advanced gastric cancer. Am J Clin Oncol. 2003. 26:37–41.

15. Park SR, Oh DY, Kim DW, Kim TY, Heo DS, Bang YJ, Kim NK, Kang WK, Kim HT, Im SA, Suh JH, Kim HK. A multi-center, late phase II clinical trial of Genexol (paclitaxel) and cisplatin for patients with advanced gastric cancer. Oncol Rep. 2004. 12:1059–1064.

16. Lee KW, Im SA, Yun T, Song EK, Na II, Shin H, Choi IS, Oh DY, Kim JH, Kim DW, Kim TY, Lee JS, Heo DS, Bang YJ, Kim NK. Phase II Trial of Low-dose Paclitaxel and Cisplatin in Patients with Advanced Gastric Cancer. Jpn J Clin Oncol. 2005. 35:720–726.

17. Vanhoefer U, Rougier P, Wilke H, Ducreux MP, Lacave AJ, Van Cutsem E, Planker M, Santos JG, Piedbois P, Paillot B, Bodenstein H, Schmoll HJ, Bleiberg H, Nordlinger B, Couvreur ML, Baron B, Wils JA. Final results of a randomized phase III trial of sequential high-dose methotrexate, fluorouracil, and doxorubicin versus etoposide, leucovorin, and fluorouracil versus infusional fluorouracil and cisplatin in advanced gastric cancer: a trial of the European Organization for Research and Treatment of Cancer Gastrointestinal Tract Cancer Cooperative Group. J Clin Oncol. 2000. 18:2648–2657.

18. Kim BS, Oh DY, Joh YH, Kim DY, Kim JH, Lee SH, Lee DH, Kim TY, Heo DS, Bang YJ, Kim NK. Efficacy of low-dose paclitaxel and cisplatin in patients with advanced non-small cell lung cancer. Cancer Res Treat. 2001. 33:469–473.

19. Simon R. Optimal two-stage designs for phase II clinical trials. Control Clin Trials. 1989. 10:1–10.

20. Hryniuk WM, Goodyear M. The calculation of received dose intensity. J Clin Oncol. 1990. 8:1935–1937.

21. Stathopoulos GP, Rigatos SK, Fountzilas G, Polyzos A, Stathopoulos JG. Paclitaxel and carboplatin in pretreated advanced gastric cancer: a phase II study. Oncol Rep. 2002. 9:89–92.

22. Ohtsu A, Boku N, Tamura F, Muro K, Shimada Y, Saigenji K, Akazawa S, Kitajima M, Kanamaru R, Taguchi T. An early phase II study of a 3-hour infusion of paclitaxel for advanced gastric cancer. Am J Clin Oncol. 1998. 21:416–419.

23. Forastiere AA, Leong T, Rowinsky E, Murphy BA, Vlock DR, De-Conti RC, Adams GL. Phase III comparison of high-dose paclitaxel+cisplatin+granulocyte colony-stimulating factor versus low-dose paclitaxel+cisplatin in advanced head and neck cancer: Eastern Cooperative Oncology Group Study E1393. J Clin Oncol. 2001. 19:1088–1095.
24. Kosmidis P, Mylonakis N, Skarlos D, Samantas E, Dimopoulos M, Papadimitriou C, Kalophonos C, Pavlidis N, Nikolaidis C, Papaconstantinou C, Fountzilas G. Hellenic Cooperative Oncology Group (HeCOG). Paclitaxel (175 mg/m2) plus carboplatin (6 AUC) versus paclitaxel (225 mg/m2) plus carboplatin (6 AUC) in advanced non-small-cell lung cancer (NSCLC): a multicenter randomized trial. Ann Oncol. 2000. 11:799–805.
25. Nabholtz JM, Gelmon K, Bontenbal M, Spielmann M, Catimel G, Conte P, Klaassen U, Namer M, Bonneterre J, Fumoleau P, Winograd B. Multicenter, randomized comparative study of two doses of paclitaxel in patients with metastatic breast cancer. J Clin Oncol. 1996. 14:1858–1867.

26. Winer EP, Berry DA, Woolf S, Duggan D, Kornblith A, Harris LN, Michaelson RA, Kirshner JA, Fleming GF, Perry MC, Graham ML, Sharp SA, Keresztes R, Henderson IC, Hudis C, Muss H, Norton L. Failure of higher-dose paclitaxel to improve outcome in patients with metastatic breast cancer: cancer and leukemia group B trial 9342. J Clin Oncol. 2004. 22:2061–2068.

27. Eisenhauer EA, ten Bokkel Huinink WW, Swenerton KD, Gianni L, Myles J, van der Burg ME, Kerr I, Vermorken JB, Buser K, Colombo N. European-Canadian randomized trial of paclitaxel in relapsed ovarian cancer: high-dose versus low-dose and long versus short infusion. J Clin Oncol. 1994. 12:2654–2666.

28. Omura GA, Brady MF, Look KY, Averette HE, Delmore JE, Long HJ, Wadler S, Spiegel G, Arbuck SG. Phase III trial of paclitaxel at two dose levels, the higher dose accompanied by filgrastim at two dose levels in platinum-pretreated epithelial ovarian cancer: an intergroup study. J Clin Oncol. 2003. 21:2843–2848.

29. Rowinsky EK, Jiroutek M, Bonomi P, Johnson D, Baker SD. Paclitaxel steady-state plasma concentration as a determinant of disease outcome and toxicity in lung cancer patients treated with paclitaxel and cisplatin. Clin Cancer Res. 1999. 5:767–774.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download