Abstract
C1q nephropathy is a proliferative glomerulopathy with extensive mesangial deposition of C1q. A three-year old boy presented with a nephrotic-range proteinuria during an acute phase of Epstein-Barr virus (EBV) infection, and he had a family history of Dent's disease. The renal biopsy findings were compatible with C1q nephropathy. However, EBV in situ hybridization was negative. The CLCN5 gene analysis revealed an R637X hemizygous mutation, which was the same as that detected in his maternal cousin, the proband of the family. The causal relationship between EBV infection and C1q nephropathy remains to be determined. Moreover, the effects of underlying Dent's disease in the process of C1q nephropathy has to be considered.
C1q nephropathy is a proliferative glomerulopathy characterized by extensive C1q mesangial deposition in the clinical setting of steroid-resistant proteinuria (1). So far, its etiology is not well-known, and the case reports associated with infection have been rare. Epstein-Barr virus (EBV) is a ubiquitous human herpes virus that causes infectious mononucleosis. In addition to the classic triad of fever, pharyngitis, and lymphadenopathy, patients with infectious mononucleosis due to acute EBV infection may develop various complications in various organs including hemolytic anemia, granulocytopenia, hepatitis, pericarditis, encephalitis, and acute interstitial nephritis (2, 3). In addition, development of glomerulonephritis in a patient with chronic active EBV infection has been also reported (4).
A three-year old boy with proteinuria during acute phase of infectious mononucleosis went through a renal biopsy, and the pathologic findings were compatible with C1q nephropathy. There has been no report of C1q nephropathy developing in association with EBV infection. Furthermore, the family history of Dent's disease incurred more confusion into the evaluation of proteinuria.
A three-year old, previously healthy boy was brought to us because of intermittent fever for seven days and foamy urine for five days. On admission, his body temperature was 39.5℃ and blood pressure was 100/60 mmHg. The throat was mildly injected without exudate or ulceration. A few thumb tip-sized cervical lymph nodes were detected bilaterally, which were non-tender and movable. Both liver and spleen were palpable with three finger-breaths. The edge of the liver was sharp, and the surface was smooth without tenderness. The urogenital examination was normal. One of his maternal cousins had proteinuria since age of three and was diagnosed as having Dent's disease by genetic testing. His maternal grandfather also had a history of proteinuria since childhood, and developed chronic renal failure several years before.
Initial laboratory investigations revealed: hemoglobin 10.4 g/dL, platelet 191,000/µL, and WBC 24,710/µL (neutrophils 21%, lymphocytes 44%, atypical lymphocytes 28%, and monocytes 7%). The blood biochemistry results were as follows; blood urea nitrogen 11 mg/dL, creatinine 0.4 mg/dL, total protein 7.4 g/dL, albumin 4.2 g/dL, and aspartate aminotransferase, alanine aminotransferase, and alkaline phosphatase were 98, 153, and 565 IU/L, respectively. EBV VCA IgM Ab was positive, and other viral markers including hepatitis B virus, hepatitis C virus, hepatitis A virus and cytomegalovirus were all negative. Urinalysis revealed two positive albuminuria with some hyaline and granular casts, but hematuria was not detected. Urinary protein excretion was 2,780 mg/day, and urinary calcium excretion was 2.7 mg/kg/day. Urinary β2-microglobulin was 163 µg/mL. The urinary protein electrophoresis revealed: albumin 34.9% and total globulin 65.1%. The SDS-PAGE of urine protein showed a mixed glomerular and tubular pattern of proteinuria. Serum C3 and C4 were 213.8 and 71.5 mg/dL, respectively. Serum IgG, IgA, and IgM were 1,590, 153, and 230 mg/dL, respectively. ASO titer, anti-double strands-DNA, and rheumatoid factor were negative. Renal ultrasonography revealed no abnormal findings.
Initially, EBV infection was easily diagnosed on the basis of typical clinical features and the positive serologic test. In addition, severe low-molecular weight proteinuria supported the possibility of underlying Dent's disease. However, nephrotic range proteinuria with a considerable proportion of albuminuria could not be explained by EBV infection and/or underlying Dent's disease. Thus, kidney biopsy was carried out to rule out a superimposing glomerular disease.
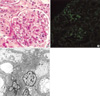
Total nineteen glomeruli were identified by light microscopic examination of the biopsied renal tissue. The glomeruli, tubules, interstitium, and blood vessels looked almost normal. However, electron microscopic examination disclosed a small amount of mesangial deposits with focal moderate effacement of epithelial foot processes. Immunofluorescence microscopic examination revealed mesangial C1q (++) and IgG (+) deposits with a granular pattern (Fig. 1). In situ hybridization of EBV was negative (data not shown).
The mutational analysis of the CLCN5 gene revealed a C-to-T point mutation that replaces the 637th codon of arginine to a stop codon. This nonsense mutation was the same one detected in his maternal cousin previously (the patient 1 in reference 5).
Leukocytosis and abnormal liver function were normalized within seven days with conservative management, and atypical lymphocytosis disappeared completely within three weeks. However, proteinuria persisted, and enalapril (2 mg/kg/day) was started by the twentieth day of hospitalization, which decreased the urine protein/creatinine ratio by approximately 50% a after six months.
Follow-up of EBV serologic markers after a month revealed positive VCA-IgM, VCA-IgG, and EA(DR)-IgG antibodies. About five months later, negative conversion of VCA-IgM Ab and positive conversion of EBNA-IgG Ab were noted.
C1q nephropathy is a controversial disease entity that was first defined by its unusual immunopathologic characteristics (1). Mostly acceptable diagnostic criteria of C1q nephropathy are mesangial immune deposits that stain dominantly or co-dominantly for C1q, corresponding mesangial electron dense deposits on electron microscopic examination, and the clinical setting of steroid-resistant proteinuria without evidence of systemic lupus erythematosus (1, 6, 7). The light microscopic findings are traditionally accepted by focal segmental glomerulosclerosis in most patients and minimal change lesion in others (7). However, some recent studies suggested that C1q nephropathy was an entity that histologically is within the minimal change disease or a Focal Segmental Glomeanlosclerosis (FSGS) and appears to show the full spectrum of histological variants seen in FSGS (8, 9).
Our patient fully met the above diagnostic criteria. The pathogenesis of C1q nephropathy is mostly unclear. Although there was a case report (10) of de novo C1q nephropathy in a graft kidney in association with human polyoma (BK) virus interstitial nephritis, association with other virus including EBV was absent. Lee et al. (11) reported a case of C1q nephropathy in a 23-month-old girl with steroid-dependent nephrotic syndrome as the first case in Korea.
EBV infection may induce renal diseases, most frequently acute interstitial nephritis during the course of infectious mononucleosis. Occasional occurrences of glomerular diseases such as IgA nephropathy, steroid-dependent minimal change nephrotic syndrome, and hemolytic uremic syndrome in patients with infectious mononucleosis have also been reported (12). In addition, post-transplant lymphoproliferative disorders caused by EBV frequently involve the graft (13). Although there have been no previous case report of C1q nephropathy in association with infectious mononucleosis and a the in situ hybridization result was negative, the causal relationship between EBV infection and C1q nephropathy cannot be completely excluded in our patient on the basis of coincidental onset of infectious mononucleosis and the foamy urine and the frequent negative result of in situ hybridization in EBV-induced nephritis (3).
There has been controversies about the effect of steroid treatment for C1q nephropathy (1, 6, 14, 15). In our patient, steroid therapy was not undertaken due to active EBV infection. Instead, enalapril treatment resulted in partial reduction of proteinuria.
Dent's disease, a renal tubular disorder caused by inactivating mutations in the CLCN5 gene encoding the ClC-5 chloride channel expressed in tubular epithelial cells, is characterized by low-molecular-weight proteinuria, hypercalciuria, nephrocalcinosis/nephrolithiasis, and progressive renal failure (5, 16, 17). The tubular component of proteinuria in our patient was thought to have resulted from underlying Dent's disease. The possible harmful influence of underlying Dent's disease on the course of C1q nephropathy should be determined by a long-term follow-up of the patient.
Figures and Tables
Fig. 1
(A) Light microscopic finding of the renal biopsy shows a glomerulus of normal size and cellularity (periodic acid-Schiff stain; original magnification, ×400). (B) Immunofluorescence microscopic examination reveals dominant mesangial staining of C1q (original magnification, ×200). (C) Electron microscopic examination shows some mesangial electron-dense deposits (original magnification, ×3,500).
References
1. Jennette JC, Hipp CG. C1q nephropathy: a distinct pathologic entity usually causing nephrotic syndrome. Am J Kidney Dis. 1985. 6:103–110.
2. Macsween KF, Crawford DH. Epstein-Barr virus-recent advances. Lancet Infect Dis. 2003. 3:131–140.

3. Cataudella JA, Young ID, Iliescu EA. Epstein-Barr virus-associated acute interstitial nephritis: infection or immunologic phenomenon? Nephron. 2002. 92:437–439.

4. Kano K, Yamada Y, Sato Y, Arisaka O, Ono Y, Ueda Y. Glomerulonephritis in a patient with chronic active Epstein-Barr virus infection. Pediatr Nephrol. 2005. 20:89–92.

5. Cheong HI, Lee JW, Zheng SH, Lee JH, Kang JH, Kang HG, Ha IS, Lee SJ, Choi Y. Phenotype and genotype of Dent's disease in three Korean boys. Pediatr Nephrol. 2005. 20:455–459.

6. Iskandar SS, Browning MC, Lorentz WB. C1q nephropathy: a pediatric clinicopathologic study. Am J Kidney Dis. 1991. 18:459–465.
7. Lau KK, Gaber LW, Delos Santos NM, Wyatt RJ. C1q nephropathy: features at presentation and outcome. Pediatr Nephrol. 2005. 20:744–749.

8. Markowitz GS, Schwimmer JA, Stokes MB, Nasr S, Seigle RL, Valeri AM, D'Agati VD. C1q nephropathy: a variant of focal segmental glomerulosclerosis. Kidney Int. 2003. 64:1232–1240.

9. Fukuma Y, Hisano S, Segawa Y, Niimi K, Tsuru N, Kaku Y, Hatae K, Kiyoshi Y, Mitsudome A, Iwasaki H. Clinicopathologic correlation of C1q nephropathy in children. Am J Kidney Dis. 2006. 47:412–418.

10. Isaac J, Shihab FS. De Novo C1q nephropathy in the renal allograft of a kidney pancreas transplant recipient: BK virus induced nephropathy? Nephron. 2002. 92:431–436.
11. Lee JW, Cho SJ, Lee SJ, Sung SH. A case of C1q nephropathy in steroid-dependent nephrotic syndrome. J Korean Soc Pediatr Nephrol. 2001. 5:206–209.
12. Verma N, Arunabh S, Brady TM, Charytan C. Acute interstitial nephritis secondary to infectious mononucleosis. Clin Nephrol. 2002. 58:151–154.

13. Nadasdy T, Park CS, Peiper SC, Wenzl JE, Oates J, Silva FG. Epstein-Barr virus infection-associated renal disease: diagnostic use of molecular hybridization technology in patients with negative serology. J Am Soc Nephrol. 1992. 2:1734–1742.

14. Davenport A, Maciver AG, Mackenzie JC. C1q nephropathy: do C1q deposits have any prognostic significance in the nephrotic syndrome? Nephrol Dial Transplant. 1992. 7:391–396.
15. Shappell SB, Myrthil G, Fogo A. An adolescent with relapsing nephrotic syndrome: minimal-change disease versus focal-segmental glomerulosclerosis versus C1q nephropathy. Am J Kidney Dis. 1997. 29:966–970.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download