Abstract
We report a case of intolerance to warfarin dosing due to impaired drug metabolism in a patient with CYP2C9*3/*4. A 73-yr-old woman with atrial fibrilation was taking warfarin. She attained a high prothrombin time international normalized ratio (INR) at the standard doses during the induction of anticoagulation and extremely low dose of warfarin (6.5 mg/week) was finally chosen to reach the target INR. Genotyping for CYP2C9 revealed that this patient had a genotype CYP2C9*3/*4. This is the first Korean compound heterozygote for CYP2C9*3 and *4. This case suggests the clinical usefulness of pharmacogenetic testing for individualized dosage adjustments of warfarin.
Warfarin therapy is problematic due to a narrow therapeutic index and frequent bleeding complications (1-5). Due to the significant interpatient variability for warfarin sensitivity, estimation of the optimal warfarin dose for each patient is difficult. The prolongation of the prothrombin time (PT) remains the primary way to measure the anticoagulant effect of warfarin. Therapy is individualized by monitoring patient's international normalized ratio (INR) of PT.
Warfarin metabolism is catalyzed by CYP2C9, which metabolizes S-wafarin to inactive S-7-hydroxywarfarin (4). A genetic polymorphism of CYP2C9 contributes to the variability among patients for the required maintenance doses of warfarin (4). Multiple studies have clearly demonstrated an increased frequency of CYP2C9 allelic variants such as CYP2C9*2 and CYP2C9*3 in patients stabilized on low-dose warfarin therapy. A relationship has been established between genetic deficiency of the CYP2C9 enzyme activity and increased likelihood of extremely elevated INRs and major bleeding events, compared to the general population (6-11).
In this report, we present a case of warfarin therapy in a patient with the genotype CYP2C9*3/*4, which resulted in decreased activity of CYP2C9. Prolonged PT during the induction phase of standard warfarin therapy was found and a marked reduction of warfarin dosage was required to get to the target INR in this case.
A 73-yr-old woman with atrial fibrillation presented to the emergency room complaining of chest discomfort, dyspnea, and agitation. The patient had suffered from atrial fibrillation for the last 2 yr. Her medications for the previous 2 yr included diltiazem 90 mg, metoprorol 25 mg, and aspirin 100 mg twice a day. In addition, she had been taking mirtazapine 30 mg, alprazolam 0.25 mg, and zolpidem 10 mg daily for a 6 yr history of dysthymia.
Physical examination showed a blood pressure of 100/83 mmHg, a heart rate of 100 beats/min, and a normal body temperature. Her body weight was 62.3 kg, and she was 158 cm in height. Initial laboratory results were unremarkable with a normal PT of 12.3 sec (INR 1.0). Routine chemical studies indicated normal values for total protein (6.6 g/dL), albumin (3.9 g/dL), aspartate aminotransferase (17 U/L), alanine aminotransferase (10 U/L), alkaline phosphatase (79 U/L), total bilirubin (0.3 mg/dL) blood urea nitrogen (16.4 mg/dL), creatinine (0.6 mg/dL), and electrolytes. Results of hematological studies including complete blood counts were also normal. Mild cardiomegaly was found on the chest radiography. Electrocardiogram showed atrial fibrillation. Echocardiogram revealed mild aortic, mitral, and tricuspid regurgitation and left atrial enlargement (45 mm).
The patient underwent heparinization with an initial bolus administration of 3,600 IU heparin followed by continuous infusion for 6 days. Then the patient was started on 2 or 3 mg of warfarin daily (16.3 mg/week) to prevent thromboembolism, and was discharged after 3 days with a PT of 37.4 sec (INR 2.81). When she revisited the outpatient clinic after 3 days, her PT was found to be 50.0 sec (INR 3.68). After normalization of the patient's PT with warfarin withdrawal for 3 days, 1 or 2 mg/day (10.5 mg/week) of warfarin was prescribed. The PT after 3 days of treatment was 41.6 sec (INR 3.11). The administration of warfarin dose was changed (6.5-10.5 mg/week) continuously, which resulted in a PT of 20.9-43.1 sec (INR 1.64-3.21). She had to discontinue warfarin therapy temporarily 3 times. The difficulty in finding the optimal treatment dose during the induction period of anticoagulation continued for more than 2 month.
The patient continues to receive warfarin therapy at the outpatient clinic monthly and her PT remains within the recommended target therapeutic range (INR 2.0-3.0), even though her warfarin dose has been reduced to 6.5 mg/week.
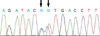
The patient was genotyped for CYP2C9 after informed consent. DNA was isolated from peripheral blood, and all 9 exons of the CYP2C9 gene were amplified by PCR (11-13). The PCR products were sequenced using the ABI PRISIM BigDye terminator Cycle sequencing kit and an ABI Prism 3100 Genetic Analyzer (Applied Biosystems, Foster City, CA, U.S.A.). The patient was found to be an intermediate metabolizer with the genotype of CYP2C9*3/*4 (Fig. 1).
Genetic polymorphisms of CYP2C9 bring about a significant variability among individuals in regard to drug response (1-4). Patients with genetic variants of CYP2C9 are very sensitive to warfarin, and may become overanticoagulated on a standard dose.
More than 20 variant alleles of CYP2C9 have been reported (14). Previous studies have demonstrated that 2 common variants CYP2C9*2 and CYP2C9*3 are associated with a reduced catalytic activity of CYP2C9 (1-11). Therefore, subjects who are homo- or heterozygous for these variant alleles require reduced maintenance doses for CYP2C9 substrates such as warfarin. Allele frequencies of CYP2C9 variants have been shown to be markedly different among populations. Caucasians possess higher frequencies of CYP2C9*3 than Asians (6-10% vs. 2-5%) (1-3). There have been no documented Asian carriers of the CYP2C9*2 variant, while 8-20% of Caucasians appear to have the CYP2C9*2 allele (1-11). Yoon et al. reported that from a pool of 574 Koreans 2.3% were heterozygous for CYP2C9*3 and none were found to be carriers of CYP2C9*2 (15). Caucasian and Asian patients require different warfarin dosages to achieve therapeutic anticoagulation and Asians appear to be more sensitive to warfarin (2, 9). This can only be partly explained by the 2 most common variant alleles of CYP2C9 in Caucasians, and there is a possibility that unknown CYP2C9 alleles exist in Asians.
This is the first report of a Korean patient with the CYP2C9*3/*4 showing warfarin intolerance. The CYP2C9*4 allele including 1076T>C (Ile359Thr) has been reported in only one Japanese subject (16). However, CYP2C9 variants other than CYP2C9*2 and CYP2C9*3 have not been studied in the Korean population. In addition, there has been no reported Korean subject identified as a compound heterozygote for the 2 variant alleles of CYP2C9.
The functional significance of the CYP2C9*4 allele remains unclear. However, it is assumed that this allele causes significant reduction in the CYP2C9 enzyme activity. It is known that CYP2C9*3, *4, and *5 alleles all lie in a putative substrate recognition site, thus providing an explanation for their effects on the Km for CYP2C9 substrates (17). The position of 1076T>C (Ile359Thr) substitution is just close to 1075A>C (Ile359Leu) in CYP2C9*3, which causes decreased enzyme activity. Therefore, 1076T>C (Ile359Thr) in CYP2C9*4 is likely to affect the enzyme activity as 1075A>C (Ile359Leu) in CYP2C9*3 (16). While the usual maintenance dose of warfarin is 4-6 mg/day in most patients (28-42 mg/week), our patient required extremely low doses of warfarin (0.5 or 1 mg/day, 6.5 mg/week) to meet the target INR, suggesting a poor metabolizer phenotype with 2 functionally deficient alleles, rather than an intermediate metabolizer phenotype with 1 deficient allele. Gage et al. reported that homozygotes for CYP2C9*3 or compound heterozygotes of CYP2C9*3 and CYP2C9*2 had an average daily maintenance warfarin dose of 1.5 mg and 2.0 mg, respectively, compared to a daily maintenance dose of 5.1 mg in wildtype (18).
According to the Korean study of Lee et al. (5), 83 patients visited emergency center for 2 yr due to the bleeding complications or high INR related to warfarin therapy. Lee et al. reported that one of the main reasons for non-therapeutic INRs was inadequate dosage adjustment (19) and suggested a dosing guideline for Korean outpatients with prosthetic heart valves (20). However, the current warfarin dosing algorithms still do not incorporate genetic factors that could affect warfarin dose requirements.
Our patient attained a high INR at standard doses and might be at a higher risk for developing severe complications. In this patient, we could not identify any specific pharmacokinetic or pharmacodynamic factors associated with the warfarin response, such as drug interactions or underlying disease conditions. Therefore, a pharmacogenetic test was performed to explore the possible genetic factors contributing to the unusual warfarin response. This patient could have taken appropriate therapeutic measures earlier, and be maintained on a safer regimen with lower doses, if she had been genotyped at the beginning of warfarin therapy.
The CYP2C9 genotype is associated with a risk of overanticoagulation and bleeding complications. Previous studies have suggested that a variant group, compared with patients with the wild-type genotype, require a higher rate of above-range INR, longer time to reach a therapeutic INR, smaller maintenance doses, longer time to stable warfarin dosing, longer hospitalization, and a higher risk of serious bleeding events (1-4, 6, 7, 11).
CYP2C9 genotyping is recommended to complement PT monitoring especially when unusual metabolic activity of warfarin is suspected. Moreover, CYP2C9 genotyping before the initiation of therapy may serve as an important guide for more rapid dosage adjustment and prediction of drug response in each individual in the future.
Figures and Tables
References
1. Kirchheiner J, Brockmoller J. Clinical consequences of cytochrome P450 2C9 polymorphisms. Clin Pharmacol Ther. 2005. 77:1–16.

2. Takahashi H, Echizen H. Pharmacogenetics of CYP2C9 and interindividual variability in anticoagulant response to warfarin. Pharmacogenomics J. 2003. 3:202–214.

3. Takahashi H, Echizen H. Pharmacogenetics of warfarin elimination and its clinical implications. Clin Pharmacokinet. 2001. 40:587–603.

4. Aithal GP, Day CP, Kesteven PJ, Daly AK. Association of polymorphisms in the cytochrome P450 CYP2C9 with warfarin dose requirement and risk of bleeding complications. Lancet. 1999. 353:717–719.

5. Lee JH, Park JS, Chung SW, Sohn DK, Kim SH, Lee HS. Warfarin toxicity patients in the Emergency Department. J Korean Soc Emerg Med. 2003. 14:145–149.
7. Higahi MK, Veenstra DL, Kondo LM, Wittkowsky AK, Srinouanprachanh SL, Farin FL, Rettie AE. Association between CYP2C9 genetic variants and anticoagulation-related outcomes during warfarin therapy. JAMA. 2002. 287:1690–1698.

8. Tabrizi AR, Zehnbauer BA, Borecki IB, McGrath SD, Buchman TG, Freeman BD. The frequency and effects of cytochrome P450 (CYP) 2C9 polymorphisms in patients receiving warfarin. J Am Coll Surg. 2002. 194:267–273.
9. Takahashi H, Kashima T, Nomizo Y, Muramoto N, Shimizu T, Nasu K, Kubota T, Kimura S, Echizen H. Metabolism of warfarin enantiomers in Japanese patients with heart disease having different CYP2C9 and CYP2C19 genotypes. Clin Pharmacol Ther. 1998. 63:519–528.

10. Scordo MG, Pengo V, Spina E, Dahl ML, Gusella M, Padrini R. Influence of CYP2C9 and CYP2C19 genetic polymorphisms on warfarin maintenance dose and metabolic clearance. Clin Pharmacol Ther. 2002. 72:702–710.

11. Lee CR, Goldstein JA, Pieper JA. Cytochrome P450 2C9 polymorphisms: a comprehensive review of the in-vitro and human data. Pharmacogenetics. 2002. 12:251–263.

12. Stubbins MJ, Harries LW, Smith G, Tarbit MH, Wolf CR. Genetic analysis of the human cytochrome P450 CYP2C9 locus. Pharmacogenetics. 1996. 6:429–439.

13. Bhasker CR, Miners JO, Coulter S, Birkett DJ. Allelic and functional variability of cytochrome P4502C9. Pharmacogenetics. 1997. 7:51–58.

14. Ingelman-Sunberg M, Nebert DW, Daly AK. Human cytochrome P450 (CYP) genes. Accession date. 11/25/2005. Available from: URL:
http://www.imm.ki.se/CYPalleles/cyp2c9.htm.
15. Yoon YR, Shon JH, Kim MK, Lim YC, Lee HR, Park JY, Cha IJ, Shin JG. Frequency of cytochrome P450 2C9 mutant alleles in a Korean population. Br J Clin Pharmacol. 2001. 51:277–280.

16. Imai J, Ieiri I, Mamiya K, Miyahara S, Furuumi H, Nanba E, Yamane M, Fukumaki Y, Ninomiya H, Tashiro N, Otsubo K, Higuchi S. Polymorphism of the cytochrome P450 (CYP) 2C9 gene in Japanese epileptic patients: genetic analysis of the CYP2C9 locus. Pharmacogenetics. 2000. 10:85–89.

17. Voora D, McLeod HL, Eby C, Gage BF. Use of pharmacogenetics to guide warfarin therapy. Drugs Today. 2004. 40:247–257.

18. Gage BF, Eby C, Milligan PE, Banet GA, Ducan JR, McLeod HL. Use of pharmacogenetics and clinical factors to predict the maintenance dose of warfarin. Thromb Haemost. 2004. 91:87–94.

19. Lee BK, Lee JY, Jeong YM, Lee MK, Kim KB, Ahn H. Analysis of factors affecting nontherapeutic INRs in Korean outpatients with mechanical heart valves. Korean J Thorac Cardiovasc Surg. 2005. 38:746–760.
20. Lee BK, Lee JY, Jeong YM, Lee MK, Kim KB, Ahn H. Determination of practical dosing of warfarin in Korean outpatients with mechanical heart valves. Korean J Thorac Cardiovasc Surg. 2005. 38:761–772.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download