Abstract
Innovative replacement of incontinence surgery (IRIS) is a polypropylene tape that is placed beneath the midurethra to restore urinary continence. We evaluated the long-term efficacy and safety of the IRIS procedure and compared it with tension-free vaginal tape (TVT) for the treatment of female stress urinary incontinence. We included all 66 consecutive women who underwent IRIS (n=34) or TVT (n=32) between February 2002 and April 2003 and followed them up for at least 3 yr postoperatively. The 3-yr success rate was 94.1% for the IRIS and 93.8% for the TVT, and the satisfaction rates were 91.2% and 90.6%, respectively. Intraoperative complications for the IRIS group included 3 cases of bladder perforation, and there were 3 cases of bladder perforation in the TVT group. The postoperative complications for the IRIS group included 2 patients with de novo urgency and one patient with mesh erosion. Three patients with TVT developed de novo urgency. One case of each group showed temporary voiding difficulty. On the basis of our results, the IRIS may be an effective and safe procedure as compared to TVT, with a high success rate and a low complication rate.
Midurethral tension-free sling procedures recreate the suburethral floor under the midurethra, and this enables coaptation of the urethra during increased intraabdominal pressure; this procedure has become popular in recent years for the treatment of stress urinary incontinence. The tension-free vaginal tape (TVT) procedure, based on the integral theory (1-3), was the first midurethral tape procedure and its high success rate was demonstrated by the recent long-term follow-up data (4, 5). The TVT procedure has become the treatment of choice for stress urinary incontinence because it is a minimally invasive operation with a high success rate after long-term follow-up (6, 7).
More recently, the innovative replacement of incontinence surgery (IRIS; B. Braun Korea & Dow Medics Co., Ltd, Seoul, Korea) procedure has been performed, and this procedure has been shown to be effective and safe for treating stress urinary incontinence. However, there have been no previous studies to compare the long-term outcomes of the IRIS and TVT procedures. Therefore, we evaluated the efficacy and safety of the IRIS procedure at the three-year follow-up, and we compared the results with those of the TVT procedure.
This retrospective clinical trial was performed at a single institution. This study included 71 consecutive women who underwent the IRIS or TVT procedure for the treatment of objective stress urinary incontinence at the Urology Department between February 2002 and April 2003. Among these patients, 66 were followed up for at least 3 yr (mean follow-up: 42.5 months, range: 36 to 50 months); the remaining 5 patients could not be followed up because they did not respond when contacted by mail and telephone. The preoperative evaluations included a medical history, physical examination, 3-day voiding diary, uroflowmetry, post-void residual urine measurement, and complete multi-channel urodynamic investigation. The urodynamic evaluation consisted of filling and voiding cystometry, and the valsalva leak point pressure (VLPP) and maximal urethral closing pressure (MUCP) measurements. All the definitions corresponded to those of the International Continence Society (8).
The IRIS and TVT procedures were performed under local, spinal or general anesthesia by one expert surgeon with using the standard technique with some modifications (3). No specific criteria were used in selecting one procedure in favor of the other.
Postoperatively, a Foley catheter was always inserted for bladder drainage and the residual urine volume was evaluated after withdrawal of the Foley catheter. If the post-void residual volume was more than 150 mL, then intermittent catheterization was proposed. Voiding difficulties were defined as a residual urine volume of 150 mL or more, as checked by post-void catheterization. Urgency was defined as the complaint of a sudden compelling desire to pass urine, which was difficult to defer, and urge incontinence was defined as the complaint of involuntary leakage accompanied by or immediately preceded by urgency (8).
All patients visited the clinics 1 yr and 3 yr after surgery, and at each visit they were again evaluated by a medical history, physical examination, uroflowmetry, and post-void residual urine measurement. We asked the patient's overall global satisfaction at 1 yr and 3 yr. We analyzed the success rates of the IRIS and TVT procedures for treatment of stress and mixed urinary incontinence, the patients' perception of satisfaction, the changes in overactive bladder symptoms after surgery, and the complications related to surgery.
The 'cure' of stress urinary incontinence was defined as an absence of any episodes of involuntary urine leakage during stressful activities and a stress cough test. 'Improvement' was defined as a significant reduction of urine leakage, and so the patient didn't require further treatment (9). 'Failure' was defined as unchanged or exacerbated urine leakage. For the success rates, cure or improvement were considered as success. The patients' perception of satisfaction was categorized as 'very satisfied', 'satisfied', 'so-so' and 'dissatisfied', with both 'very satisfied' and 'satisfied' scored as satisfaction. Safety data were collected during the entire follow-up period. In this trial, the success and satisfaction rates were the primary endpoints of the study.
All statistical analyses were performed with the Statistical Package for the Social Sciences (version 12.0), and they are presented as either the mean±standard deviation or the frequency (percentage). The differences between the IRIS and TVT groups in perioperative and postoperative results, including the surgical outcomes were compared using Student's t-test and the chi-square test. A p value below 0.05 was considered statistically significant for all comparisons.
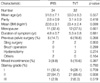
Table 1 shows the characteristics of the 66 patients. No significant baseline differences were found between the IRIS and TVT groups.
No statistical significant difference was found in the follow-up period (41.6±1.7 months vs. 43.2±2.1 months, respectively), the mean operative time (26.6±4.1 min vs. 27.5±2.7 min, respectively), the hospital stay (2.6±0.9 days vs. 2.5±0.9 days, respectively), and the period of catheter indwelling (1.5±0.6 days vs. 1.1±0.4 days, respectively) between the two groups (Table 2).
There was no statistically significant difference in the preoperative and postoperative uroflowmetry results of the two procedures. For both groups, the maximal flow rate dropped significantly at 7-day after the operation (p=0.002 vs. 0.026). Over time, however, the maximal flow rate increased gradually and it was similar to the preoperative flow rate at 3-yr. Residual urine increased significantly at postoperative 7-day and this decreased at 1-yr and 3-yr in both groups (Table 3).
The success rates and satisfaction rates in these 66 women are presented in Table 4. The overall 1-yr and 3-yr success rates were 97.0% and 93.9%, respectively. At 1 yr and 3 yr, the IRIS and TVT had similar success rates (97.1% and 94.1% vs. 96.9% and 93.8%, respectively). Furthermore, at 1 yr and 3 yr, there was no statistical difference in the satisfaction rates of the two procedures (94.1% vs. 93.8% and 91.2% vs. 90.6%, respectively) (Table 4).
Both groups had similar perioperative and postoperative complications. There were no bowel, nerve or major vessel injuries in either groups (Table 5). Three patients in each group (8.8% vs. 9.3%, respectively) had bladder perforation, which was managed with an indwelling urinary catheter for 1-3 days. Two patients (5.8%) in the IRIS group and three (9.3%) in TVT group developed de novo urgency or urge incontinence, and one patient in each group (2.9% vs. 3.1%, respectively) developed transient voiding difficulties. There was one other complication in IRIS group: one patient (2.9%) experienced tape erosion into the vagina that required partial tape removal. After tape removal, the patient experienced recurred urine leakage that was about the same as her preoperative condition.
The mean follow-up period of 5 patients (n=2 vs. 3, respectively), who could not be followed up for 3 yr, was 6 months (range: 3 to 13 months). Until the follow-up, their results were included as successful and there were no complications.
Stress urinary incontinence (SUI) is a common problem among women, particularly after childbearing. The surgical procedures used for the management of women with severe stress urinary incontinence are urethral bulking agents, suburethral sling procedures, and colposuspension such as the Burch operation. The TVT procedure is based on the integral theory and was first described in 1996 (3); it has become popular for the treatment of stress urinary incontinence due to its high success rates (4-7), in addition to its simplicity and minimal invasiveness. Many surgeons have adopted midurethral tape procedures as their primary operation for treating stress urinary incontinence (10). While most of the published literature has focused on TVT, numerous other midurethral systems are presently being introduced for the treatment of stress urinary incontinence. It is important to demonstrate equivalent efficacy and safety for these different procedures.
The instrument of the IRIS system is comprised of a non-disposable metal handle to which two metal needles can be attached. The needles have an outer diameter of 5-6 mm; the non-absorbable polypropylene tape, which is 11 mm wide and 450 mm long with a plastic sheath cover, is fixed to the needles. Polypropylene sling procedures can be differentiated by the implantation technique, and most importantly, by the conformation of the polypropylene mesh that is used (11). Synthetic meshes are characterized on the basis of pore size. Pore sizes larger than 75 µm are known as 'macroporous', whereas those less than 10 µm are known as 'microporous'. The tape of the IRIS system is polypropylene monofilament mesh (Trelex; Meadox Medicals, Oakland, NJ/Boston Scientific, NJ, U.S.A.), and the diameter of the pore size is greater than 75 µm such as the tape of TVT or SPARC (Suprapubic arch) (12). The larger pore size and monofilament nature of this mesh allows connective tissue ingrowth into the mesh with collagen deposition around the polypropylene fiber and this is thought to decrease the risk of infection by allowing easier penetration of inflammatory cells such as leukocytes and macrophages into the graft to phagocytose bacteria (13). Moreover, the IRIS polypropylene monofilament tape is more densely threaded and less extensible than TVT. Accordingly, in the IRIS procedure, the mesh can no longer be moved once in place, and this allows a possibly higher success rate in the long-term results.
The success rate of 93.8% at 3-yr follow-up in the TVT group is comparable to the previously published reports (6, 14). Furthermore, in our study the IRIS and TVT did not have statistically significant differences in the success rates, satisfaction rates, or complication rates. The high long-term success rates and low complication rates of the IRIS procedure show that this procedure was safe and effective, making this technique the optimal surgical treatment for female stress urinary incontinence. For the patients followed for a minimum of 3 yr, we found that the success (cured and improved) rate was maintained from 97.1% at 1 yr to 94.1% at 3 yr.
According to Ulmsten (15), and Lo et al. (16), the number of failures of TVT was increased for the intrinsic sphinctor deficiency (ISD) patients compared to that for the patients with genuine stress incontinence without ISD. In our study, two patients in each group, who were regarded as treatment failures, had low MUCP (14/18/24/26 cmH2O) and VLPP (48/53/57/62 cmH2O) values.
Although the TVT procedure creates dynamic urethral kinking without compressing the urethra at rest (17), 2.8% to 14% of the patients later develop obstructive voiding symptoms (18). According to another paper, the highest obstruction-inducing risk is the surgeon himself according to tensioning the tape too much (19). In our study, one patient in each group has transient voiding difficulties; this resolved within 1-2 weeks without release or resection of the tape. When evaluating the uroflowmetry indices and voiding symptoms after the IRIS or TVT procedures, we found that the maximal flow rate decreased significantly after surgery, but during the 3-yr follow-up, it increased up to the preoperative levels in both groups. This might have been due to a slow, downward displacement of the tape and the surrounding tissues, which resulted in less marked urethral compression, or it may have been due to chronic obstruction that resulted in progressive detrusor hypertrophy and this allowed better emptying function.
Bladder perforation is one of the most frequently observed complications after the TVT procedure. A recent review of the TVT literature showed the bladder perforation rate ranged from 0.7% to 19% (14, 20, 21). We observed that three patients in each group (8.8% vs. 9.3%, respectively) experienced bladder perforation, although most of these patients only needed an indwelling catheter for a short period of time.
For analyzing the changes in urge incontinence and overactive bladder symptoms after the TVT procedure, Segal et al. reported that 4.3% and 9.1% of patients with pure stress urinary incontinence were found to have developed de novo urgency and de novo incontinence, respectively (22). In our study, two patients (5.8%) in the IRIS group and three (9.3%) in the TVT group were found to have developed de novo urgency or de novo urge incontinence. Of the patients with mixed urinary incontinence, the urge component resolved in 66.7% and 60.0% in both groups, respectively. However, there was no long-term voiding dysfunction after surgery, nor were there bowel, nerve or major vessel injuries in either groups.
In conclusion, the objective surgical outcomes and various complications of the IRIS and TVT procedures, at 3-yr follow-up, were not significantly different in this study. The high long-term success rates and low complication rates of the IRIS procedure show that this procedure is effective and safe for the treatment of stress and mixed urinary incontinence.
Figures and Tables
Table 3
Preoperative and postoperative uroflowmetry results

Values are presented as mean±standard deviation. Data were evaluated using Student's t-test.
*p<0.05 compared with Preop; †p>0.05 compared with Preop.
IRIS, Innovative replacement of incontinence surgery; TVT, Tension-free vaginal tape; MFR, maximal flow rate; AFR, average flow rate; PVR, post-void residual urine volume.
References
1. Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand Suppl. 1990. 153:7–31.
2. Petros PE, Ulmsten UI. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol Suppl. 1993. 153:1–93.
3. Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996. 7:81–85.

4. Nilsson CG, Falconer C, Rezapour M. Seven-year follow-up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol. 2004. 104:1259–1262.

5. Tsivian A, Mogutin B, Kessler O, Korczak D, Levin S, Sidi AA. Tension-free vaginal tape procedure for the treatment of female stress urinary incontinence: long-term results. J Urol. 2004. 172:998–1000.

6. Ulmsten U, Johnson P, Rezapour M. A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol. 1999. 106:345–350.

7. Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U. Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001. 12:Suppl 2. S5–S8.

8. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A. Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003. 61:37–49.

9. Stamey TA. Endoscopic suspension of the vesical neck for urinary incontinence in females. Report on 203 consecutive patients. Ann Surg. 1980. 192:465–471.
10. Bemelmans BL, Chapple CR. Are slings now the gold standard treatment for the management of female urinary stress incontinence and if is so what technique? Curr Opin Urol. 2003. 13:301–307.
11. Amid PK. Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia. 1997. 1:15–21.

12. Karlovsky ME, Thakre AA, Rastinehad A, Kushner L, Badlani GH. Biomaterials for pelvic floor reconstruction. Urology. 2005. 66:469–475.

13. Dwyer PL. Evolution of biological and synthetic grafts in reconstructive pelvic surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2006. 17:Suppl 1. S10–S15.

14. Niknejad K, Plazk LS IIIrd, Staskin DR, Loughlin KR. Autologous and synthetic urethral slings for female incontinence. Urol Clin North Am. 2002. 29:597–611.

15. Ulmsten U. An introduction to tension-free vaginal tape (TVT)- a new surgical procedure for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001. 12:Suppl 2. 3–4.
16. Lo TS, Wang AC, Liang CC, Long CY, Lee SJ. Treatment for unsuccessful tension-free vaginal tape operation by shortening pre-implanted tape. J Urol. 2006. 175:2196–2199.

17. Lo TS, Wang AC, Horng SG, Liang CC, Soong YK. Ultrasonographic and urodynamic evaluation after tension free vagina tape procedure (TVT). Acta Obstet Gynecol Scand. 2001. 80:65–70.

18. Klutke C, Siegel S, Carlin B, Paszkiewicz E, Kirkemo A, Klutke J. Urinary retention after tension-free vaginal tape procedure: incidence and treatment. Urology. 2001. 58:697–701.

19. Fischer A, Fink T, Zachmann S, Fickenbusch U. Comparison of retropubic and outside-in transobturator-sling systems for the cure of female genuine stress urinary incontinence. Eur Urol. 2005. 48:799–804.
20. Abouassaly R, Steinberg JR, Lemieux M, Marois C, Gilchrist LI, Bourque JL, Tule M, Corcos J. Complications of tension-free vaginal tape surgery: a multi-institutional review. BJU Int. 2004. 94:110–113.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download