Abstract
The objectives of the present study were to evaluate the efficacy and safety of an outpatient-basis chemotherapy of oxaliplatin, 5-fluorouracil, and leucovorin as the first-line treatment for patients with advanced colorectal cancer. Forty-three histologically confirmed patients with metastatic or recurrent colorectal cancer were enrolled. The chemotherapy consisted of oxaliplatin 85 mg/m2 as a 2-hr infusion on day 1, plus leucovorin 30 mg/m2 over 10 min, followed by bolus 5-fluorouracil 400 mg/m2 and an 8-hr infusion of 5-fluorouracil 600 mg/m2 on days 1 and 2 (modified FOLFOX4), all of which were administered on an outpatient basis every 2 weeks. The median age was 58 yr (range 33-72 yr), and 25 (58.1%) patients had metastatic diseases. Eventually, 39 patients were assessable for efficacy and all assessable for toxicity. Four (9.3%) complete responses and 11 (25.6%) partial responses were confirmed, giving an overall response rate of 34.9% (95% CI; 20.0-49.7%). The median time to progression and median overall survival for all patients was 6.1 months and 17.4 months, respectively. Grade 3/4 neutropenia occurred in 2 patients (4.7%) and febrile neutropenia was observed in 1 patient (2.3%). Modified FOLFOX4, an outpatient-basis regimen, was found to be well-tolerated and effective as the first-line chemotherapy in patients with advanced colorectal cancer.
Although surgery is potentially curative for colorectal cancer, about 50% of all newly diagnosed patients ultimately develop a metastatic disease (1). Intravenous 5-fluorouracil (FU) has been the mainstay of chemotherapy for metastatic or recurrent colorectal cancer for many years. Prolonged infusion of 5-FU in combination with the biomodulator leucovorin (LV) has an improved safety and efficacy profile when compared with bolus 5-FU/LV (2, 3), although there is an inconvenience and morbidity associated with long-term central venous access.
In 1990s, two additional agents, irinotecan and oxaliplatin, were found to exhibit activity against metastatic colorectal cancer. Infused 5-FU/LV in combination with oxaliplatin, a third generation platinum analog, proved more effective than 5-FU/LV alone in the first- and second-line treatment of metastatic colorectal cancer. As such, the addition of oxaliplatin to 5-FU/LV therapy significantly increased the response rates and time to disease progression (TTP) compared with 5-FU/LV in the first-line treatment of colorectal cancer in three randomized studies (4, 5) and as second-line therapy versus 5-FU/LV (6). Recently, a large cooperative group trial (N9741) showed significant improvements in the response rate, TTP, and overall survival (OS) with oxaliplatin plus infused 5-FU/LV versus irinotecan plus bolus 5-FU/LV (7).
Among various combination regimens of oxaliplatin plus 5-FU/LV, the FOLFOX4 regimen (oxaliplatin 85 mg/m2, LV 200 mg/m2, 5-FU 400 mg/m2 bolus, and 5-FU 600 mg/m2 continuous infusion) is the most extensively studied oxaliplatin-containing regimen, with consistently high levels of antitumor activity against advanced colorectal cancer in phase III clinical trials (4). Yet, despite the increased efficacy associated with the FOLFOX4 regimen, the continuous infusion schedule of 5-FU remains inconvenient and requires frequent hospitalization or central venous catheterization.
Accordingly, the present study evaluated the efficacy and safety of outpatient-basis chemotherapy with oxaliplatin plus 5-FU/LV as the first-line treatment for patients with advanced colorectal cancer.
All patients enrolled in the present study had histologically confirmed metastatic or recurrent colorectal cancer. The patients' age ranged from 18 to 75, with a performance status of 0 to 2 on the Eastern Cooperative Oncology Group (ECOG) scale. Plus, adequate hematological (WBC count ≥4×109/L, platelet count ≥100×109/L, hemoglobin ≥9 g/dL), renal (serum creatinine ≤1.5 mg/dL and creatinine clearance ≤50 mL/min), and hepatic (total bilirubin ≤2.0 mg/dL and serum transaminase level ≤3 times the upper limit of the normal range) functions were also required. Patients who had received adjuvant chemotherapy completed 4 weeks before entry were eligible (8, 9). However, patients were ineligible if they had previously received palliative chemotherapy or radiation therapy. Patients with CNS metastases, secondary malignancies, or other severe medical illnesses were also excluded. The institutional review board of the authors' institution approved the protocol, and written informed consent was obtained from all patients before enrollment.
On day 1, oxaliplatin (85 mg/m2) was given as a 2-hr infusion in 500 mL of a 5% dextrose solution. On days 1 and 2, LV (30 mg/m2) was administered as a 10-min infusion immediately followed by 5-FU (400 mg/m2/d) given as a 10-min iv bolus, and 5-FU (600 mg/m2/d) as a continuous 8-hr infusion with a light shield (Fig. 1). Treatment was repeated every 2 weeks. All patients received a 5-HT3 receptor antagonist as a routine emesis prophylaxis. Treatment was continued until disease progression, unacceptable toxic effects, or patient refusal.
The next course of treatment only began when neutrophil count was ≥1.5×109/L, the platelet count was ≥75×109/L, and any other treatment-related toxicities were less than or equal to grade 1; otherwise, treatment was withheld for up to 2 weeks. If adverse events did not improve to grade 0 or 1 after 3 weeks, the patients were excluded from the study.
Treatment was continued at the same dose if patients experienced grade 1 toxicities or other toxicities considered by the investigator unlikely to become serious or life threatening (e.g. alopecia). For all other treatment-related adverse events with a grade 2 intensity or higher, the dose modification scheme described below was implemented. No dose reduction was required after the first appearance of a grade 2 toxicity, although treatment was interrupted until the toxicity was resolved to grade 0 to 1. The doses of oxaliplatin and 5-FU were reduced by 25% in patients who experienced a second occurrence of a given grade 2 non-hematologic toxicity or any grade 3 hematologic or non-hematologic toxicity.
The dose of oxaliplatin was reduced by 25% in subsequent cycles in the case of persistent (≥14 days) or temporary (7 to 14 days) painful paresthesia, or functional impairment. If patients experienced a third occurrence of a given grade 2 non-hematologic toxicity, a second occurrence of a given grade 3 hematologic or non-hematologic toxicity, or any grade 4 toxicity, both doses were reduced by 50%. The oxaliplatin and 5-FU were both discontinued if, despite a dose reduction, a given toxicity occurred for a fourth time at grade 2, a third time at grade 3, or a second time at grade 4. If adverse events did not improve to grade 0 or 1 after 3 weeks, the patients were excluded from the study
A screening assessment, including a medical history, physical examination, electrocardiogram (ECG), chest radiography, and tumor assessment, was conducted within 2 weeks before starting treatment. Further assessments conducted within 7 days before starting treatment included vital signs, an ECOG performance status, and laboratory tests. Complete blood counts were performed weekly during the first cycle and every cycle thereafter, and biochemical tests performed before each cycle. The computed tomography (CT) of measurable lesions was assessed as a baseline and repeated every 3 cycles. The tumor responses were classified according to the response evaluation criteria in solid tumors (RECIST) guidelines (10). Patients with a complete response (CR) or partial response (PR) required a confirmatory disease assessment at least 4 weeks later. Adverse events were graded according to NCI-CTC version 3.0.
An optimal, two-stage Simon design (11) was used to determine the exact number of patients included in the current trial. The hypotheses was that H0: P≤P0 (0.15) versus H1: P≥P1 (0.35) with α=0.05, and β=0.10 (90% power). Allowing for a follow-up loss rate of 10%, the total sample size was 42 patients with a measurable disease. All enrolled patients were included in the intention-to-treat analysis of efficacy. The TTP and OS analyses were all estimated using the Kaplan-Meier method. The TTP was calculated from the initiation of chemotherapy to the date of disease progression, and OS was measured from the initiation of chemotherapy to the date of the last follow-up or death. The statistical data were obtained using an SPSS software package (SPSS 11.5 Inc. Chicago, IL, U.S.A.).
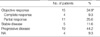
The patient characteristics are summarized in Table 1. From December 2003 to July 2005, a total of 43 biopsy-proven patients were enrolled in the current study. The median age was 58 yr (range, 33-72 yr), and there were 22 males and 21 females. The primary tumor location was the colon in 21 patients (49%) and the rectum in 22 patients (51%). Eighteen patients (42%) received chemotherapy for recurred diseases and 25 patients (58%) for metastatic diseases. The most common metastatic site was the liver in 30 patients (70%). Before chemotherapy, 40 patients (93%) received operative therapy, which was curative in the case of 16 patients and palliative in the other 24 cases. Fourteen patients (10 patients: 5-FU/LV, 4 patients: capecitabine) received adjuvant chemotherapy after surgery. There was no significant difference in baseline characteristics between chemotherapy naive group and adjuvant chemotherapy group.
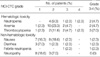
Thirty-nine of the original 43 patients were assessable for response, with the remaining 4 being lost to follow-up or patient refusal. All relevant data are reported using the intention-to-treat patient population. Four cases of CR and 11 cases of PR were confirmed, giving an overall response rate of 34.9% (95% CI; 20.0-49.7%) (Table 2). The median duration of response in the 15 responding patients was 185 days (range, 50-417 days). The median TTP for all patients was 6.1 months (95% CI; 3.3-8.9 months) with a median follow-up duration of 9.4 months (95% CI; 0.3-25.3 months) (Fig. 1). In the case of progression, 2nd-line chemotherapy was recorded for 20 patients, where 17 received FOLFIRI (irinotecan 180 mg/m2, LV 30 mg/m2, 5-FU 400 mg/m2 bolus, and 5-FU 600 mg/m2 continuous infusion) and 3 received capecitabine (2,500 mg/m2). The median OS was 17.4 months (95% CI; 10.9-23.8 months) with an estimated 1-yr survival rate of 68.4% (95% CI; 60.0-76.8%) (Fig. 2). There was no significant difference in the overall response rate, TTP, and between chemotherapy naive group and adjuvant chemotherapy group (data not shown).
A total of 284 cycles of chemotherapy were administered to the 43 patients. The median number of cycles was 9, ranging from 2 to 12 cycles. All patients were assessable for toxicities. The hematologic and non-hematologic toxicities that occurred during the current study are summarized in Table 3. Grade 3/4 neutropenia occurred in 2 patients (4.7%), while febrile neutropenia was observed in one patient (2.3%). All cases were successfully treated with the granulocyte colonystimulating factor (G-CSF) and empirical antibiotics. Nausea was the most common non-hematologic toxicity. Grade 1/2 nausea was observed in 15 patients (34.9%), and only one patient experienced grade 3 nausea. Nonetheless, no grade IV non-hematologic toxicity was observed. Peripheral neuropathy appeared in the form of transient cold exacerbated paresthesia or dysesthesia, yet no grade 3/4 neuropathy was observed. There was no case of death attributed to chemotherapy-induced toxicity. The dose intensity of 5-FU and oxaliplatin was 94.5% and 93.4%, respectively.
In the current study, the modified FOLFOX4 regimen, which can be administered on an outpatient basis, was shown to have effective antitumor activity and a safe toxicity profile in patients with metastatic or recurrent colorectal cancer. The overall response rate (34.9%), median TTP (6.1 months), and median OS (17.4 months) following treatment with the present regimen were comparable with previous results reported for the original FOLFOX4 regimen (3-5, 12, 13). For example, Antre et al. (13) reported that the FOLFOX4 regimen produced an overall response rate of 23.5%, median TTP of 5.1 months, and median overall survival of 11.1 months. Plus, the recent phase II studies, which also adopted a low dose of LV (modified FOLFOX4 regimen; oxaliplatin 85 mg/m2, LV 20 mg/m2, 5-FU 400 mg/m2 bolus, and 5-FU 600 mg/m2 continuous infusion) demonstrated a similar efficacy and toxicity to the original FOLFOX4 regimen (14-16). For patients with metastastic colorectal cancer, where treatment is essentially palliative, the protracted infusion times represent a significant portion of the patient's remaining life span. In addition, patients are exposed to potential complications resulting from central venous access. Therefore, the simplified FOLFOX4 regimen is likely to have important implications for the patient's quality of life.
One of the major toxicities related to 5-FU/LV is myelosuppression. Chemotherapy-induced severe neutropenia can also result in treatment-related hospitalization or mortality, thereby compromising the quality of life and increasing medical expenditure. In a previous study with the FOLFOX4 regimen, grade 3/4 neutropenia and febrile neutropenia occurred in 36.9% and 7% of the patients, respectively (13). However, in the current study, grade 3/4 neutropenia was only observed in 2 patients (4.7%) and febrile neutropenia only in one (2.3%). Furthermore, all these cases improved after treatment with G-CSF and empirical antibiotics. These results seemed to be due to reduced dose of LV (30 mg/m2) compared to that (200 mg/m2) of the original FOLFOX4 regimen. Another major toxicity related to oxaliplatin is peripheral neuropathy. In the present study, grade 1/2 neuropathy was observed in 25.6% of patients, and was effectively treated with conservative therapies. Of the other non-hematologic adverse effects, grade 1/2 nausea occurred in 34.9% of patients, yet grade 3 nausea was only observed in 2.3% of patients.
In conclusion, the outpatient-basis regimen of oxaliplatin plus 5-FU/LV was found to be well-tolerated and effective in patients with metastatic or recurrent colorectal cancer. Accordingly, the current regimen can be regarded as an important outpatient treatment option for advanced colorectal cancer.
Figures and Tables
References
1. American Cancer Society. Cancer Facts and Figures-2000. 2000. Atlanta, GA: American Cancer Society.
2. de Gramont A, Bosset JF, Milan C, Rougier P, Bouche O, Etienne PL, Morvan F, Louvet C, Guillot T, Francois E, Bedenne L. Randomized trial comparing monthly low-dose leucovorin and fluorouracil bolus with bimonthly high-dose leucovorin and fluorouracil bolus plus continuous infusion for advanced colorectal cancer: a French intergroup study. J Clin Oncol. 1997. 15:808–815.

3. Andre T, Colin P, Louvet C, Gamelin E, Bouche O, Achille E, Colbert N, Boaziz C, Piedbois P, Tubiana-Mathieu N, Boutan-Laroze A, Flesch M, Buyse M, de Gramont A. Semimonthly versus monthly regimen of fluorouracil and leucovorin administered for 24 or 36 weeks as adjuvant therapy in stage II and III colon cancer: results of a randomized trial. J Clin Oncol. 2003. 21:2896–2903.
4. de Gramont A, Figer A, Seymour M, Homerin M, Hmissi A, Cassidy J, Boni C, Cortes-Funes H, Cervantes A, Freyer G, Papamichael D, Le Bail N, Louvet C, Hendler D, de Braud F, Wilson C, Morvan F, Bonetti A. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol. 2000. 18:2938–2947.

5. Giacchetti S, Perpoint B, Zidani R, Le Bail N, Faggiuolo R, Focan C, Chollet P, Llory JF, Letourneau Y, Coudert B, Bertheaut-Cvitkovic F, Larregain-Fournier D, Le Rol A, Walter S, Adam R, Misset JL, Levi F. Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil-leucovorin as first-line treatment of metastatic colorectal cancer. J Clin Oncol. 2000. 18:136–147.

6. Rothenberg ML, Oza AM, Bigelow RH, Berlin JD, Marshall JL, Ramanathan RK, Hart LL, Gupta S, Garay CA, Burger BG, Le Bail N, Haller DG. Superiority of oxaliplatin and fluorouracil-leucovorin compared with either therapy alone in patients with progressive colorectal cancer after irinotecan and fluorouracil-leucovorin: interim results of a phase III trial. J Clin Oncol. 2003. 21:2059–2069.

7. Goldberg RM, Sargent DJ, Morton RF, Fuchs CS, Ramanathan RK, Williamson SK, Findlay BP, Pitot HC, Alberts SR. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004. 22:23–30.

8. Nancy K, Carlos AG, Jayne G, Howard H, Peter K, Al B, Debra SB, Jonathan P, Michael W, Grace S, Doreen H, Brent B, Sunil G. Randomized multicenter phase II trial of bolus plus infusional fluorouracil/ leucovorin compared with fluorouracil/leucovorin plus oxaliplatin as third-line treatment of patients with advanced colorectal cancer. J Clin Oncol. 2004. 22:4753–4761.
9. Yves B, Erick G, Bruno C, Sylvie N, Jean-Yves P, Jean-Luc R, Jocelyne P, Olivier R, Claude K, Caroline G, Mohamed B, Dominique M, Mireille M. Randomized multicenter phase II study comparing a combination of fluorouracil and folinic acid and alternating irinotecan and oxaliplatin with oxaliplatin and irinotecan in fluorouracil-pretreated metastatic colorectal cancer patients. J Clin Oncol. 2001. 19:4195–4201.
10. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000. 92:205–216.
11. Simon R. Optimal two-stage designs for phase II clinical trials. Control Clin Trials. 1989. 10:1–10.

12. Ramanathan RK, Clark JW, Kemeny NE, Lenz HJ, Gococo KO, Haller DG, Mitchell EP, Kardinal CG. Safety and toxicity analysis of oxaliplatin combined with fluorouracil or as a single agent in patients with previously treated advanced colorectal cancer. J Clin Oncol. 2003. 21:2904–2911.

13. Andre T, Bensmaine MA, Louvet C, Francois E, Lucas V, Desseigne F, Beerblock K, Bouche O, Carola E, Merrouche Y, Morvan F, Dupont-Andre G, de Gramont A. Multicenter phase II study of bimonthly high-dose leucovorin, fluorouracil infusion, and oxaliplatin for metastatic colorectal cancer resistant to the same leucovorin and fluorouracil regimen. J Clin Oncol. 1999. 17:3560–3568.
14. Kwon HC, Kim KT, Lee SA, Park JS, Kim SH, Kim JS, Kim HJ. Oxaliplatin with biweekly, low dose leucovorin and bolus and continuous Infusion 5-fluorouracil (Modified FOLFOX 4) as First-line therapy for patients with metastatic colorectal cancer. Cancer Research Treatment. 2004. 36:115–120.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download