Abstract
The purpose of this study was to determine the effect of twin-to-twin delivery interval on umbilical artery acid-base status of the second twin at birth. This was a retrospective cohort study of all live-born twins with measured acid-base status in umbilical arterial blood who were delivered after 34 weeks' gestation from June 2003 to February 2006. Twins with any maternal or fetal complications were excluded. Subjects were divided into two groups based on the mode of delivery of the first twin: normal cephalic vaginal deliveries (n=40) or cesarean deliveries (n=67). The inter-twin differences in umbilical arterial blood pH, PCO2, PO2, and base excess in twin newborns born vaginally were significantly greater than the corresponding differences in those born by cesarean section. A significant positive correlation was found between twin-to-twin delivery interval and inter-twin difference in umbilical arterial blood pH in twin newborns born vaginally. The umbilical arterial blood pH of the second twin was less than 7.0 in 14% (2/14) in cases delivered more than 20 min after the first twin. The umbilical arterial blood gas status of the second twin worsened with increasing twin-to-twin delivery interval, and pathologic fetal acidemia (pH < 7.0) might develop in the second twin when the twin-to-twin delivery interval was greater than 20 min.
Twins complicate approximately 1-2% of all pregnancies and contribute significantly to perinatal morbidity and mortality (1-4). The perinatal mortality rate in second twins born at term is higher than in first twins, and this increased mortality is mainly due to intrapartum hypoxia (5), which may result from premature separation of the placenta after the vaginal delivery of the first twin or a longer period of aortocaval compression for the second twin (6, 7). Therefore, this risk in second twins can theoretically increase with increasing time between the deliveries of twins.
Traditionally it has been considered that the inter-twin delivery interval should be preferably less than 15 min and certainly no more than 30 min, to minimize the risk of hypoxia in the second twin (6-10). On the other hand, several investigators have shown no increased risk in perinatal morbidity or mortality with increasing inter-twin delivery interval if continuous electronic fetal heart monitoring was used (11-14). The reasons for discrepant results among studies may be due to the different outcome variables used for analyses, which have included Apgar scores and mortality rate, and the fact that previous studies have involved heterogeneous twin pregnancies with different modes of delivery for second twins. Apgar scores or perinatal mortality alone provide unsatisfactory means of defining birth asphyxia or predicting the neurologic outcome of newborns (15-17). Moreover, both breech extraction and intrapartum external version are potential confounding variables that clearly affect the clinical condition of newborns (1, 7, 18, 19). Therefore, we focused on the outcome of newborns based on fetal acid-base status as measured in umbilical arterial blood to provide objective evidence of peripartum asphyxial insult and subsequent neonatal outcome, and in addition, we selected twin pregnancies where both twins were delivered in the normal cephalic vaginal mode. The purpose of this study was to determine the effect of twin-to-twin delivery interval on umbilical artery acid-base status of the second twin at birth.
This was a retrospective study conducted at Seoul National University Bundang Hospital between June 2003 and February 2006, using data stored in an electronic medical record system. The study population consisted of all twin deliveries during the study period who met the following criteria: 1) live births of both twins; 2) delivery occurring after 34 completed weeks of gestation; 3) no significant obstetric or medical complications (i.e., discordant growth [defined as a birth weight discrepancy of more than 20%], twin-to-twin transfusion, fetal growth restriction, fetal congenital anomaly, and preeclampsia); 4) with determined umbilical artery acid-base status immediately after the delivery of each twin. Subjects were divided into two groups based on the mode of delivery of the first twin (twin A): normal cephalic vaginal deliveries (n=40) or cesarean deliveries (n= 67). We first compared inter-twin differences in blood gas parameters between these two study groups. In the vaginal delivery cohort, we then examined the relationship between twin-to-twin delivery interval and inter-twin differences in umbilical arterial blood pH. Inter-twin differences in blood gas parameters were calculated by subtracting the values of cord gas variables in the second twin (twin B) from those of the first twin. The twin-to-twin delivery interval was defined as the time between the deliveries of twins. Antenatal, postnatal, and neonatal data were collected from maternal and neonatal charts by one of the authors. This retrospective study was exempted from institutional review board approval because it was performed by chart review only.
Intrapartum twin management was carried out according to the standard protocol used at Seoul National University Bundang Hospital. Twins in a vertex-vertex position were given a trial of labor. Labor was induced in all patients who remained undelivered at 38 weeks' gestation. During labor, both twins were continuously monitored using a dual channel monitor that simultaneously recorded a fetal heart rate tracing of both twins. A large episiotomy was usually made, and twin A was delivered in the same manner as a singleton. After the delivery of twin A, continuous monitoring of the fetal heart rate was undertaken while watching for any excess vaginal bleeding. Oxytocin infusion was started if uterine contractions did not resume within 10 min after the delivery of twin A.
Immediately after the delivery of each twin, segments of umbilical cord were doubly clamped and labeled. Samples of blood from the umbilical artery of each cord were drawn into labeled heparinized syringes, which were then capped with a plastic cover and placed in an iced-filled container. These samples were analyzed immediately for arterial pH, PCO2, PO2, and base excess, using an automatic blood gas analyzer (OMNI, Roche, Swiss).
Univariate analysis was conducted using the χ2 test, the Student's t test or the Mann-Whitney U test. Pearson correlation analysis was used to determine the relationship between twin-to-twin delivery interval and inter-twin difference in umbilical arterial blood pH in twin newborns born vaginally. p values of <0.05 were considered statistically significant.
From June 2003 to February 2006, 2,358 women delivered, of whom 189 (8%) had twins, and among the 158 women with live-born twins born at or beyond 34 weeks' gestation, 27 had a maternal or fetal complication, and 24 did not have cord blood gas results for either of the twins. Thus, these women were excluded from the study, leaving a total of 107 women for the study population. The distribution of twins by presentation included 54 vertex-vertex pairs, 34 vertex-nonvertex pairs, and 19 pairs with a nonvertex twin A. Of the 54 vertex-vertex twin pairs, 39 were born vaginally, 14 were born by cesarean section (because of fetal distress [n=1], a failure to descend [n=6], and previous uterine surgery [n= 7]), and in one case, twin A was born vaginally and twin B by cesarean section because of failure to progress and fetal distress. All pairs with a vertex-nonvertex twin or a nonvertex twin A were delivered by cesarean section.
Table 1 describes the demographic and clinical characteristics of the study population according to the mode of delivery of twin A. No significant differences were found in terms of mean maternal age, the distribution of parous and nonparous women, mean gestational age at delivery, or mean birth weights of twin A and twin B between the two groups. Moreover, the incidences of a low Apgar score at 1 and 5 min for twin A were not significantly different between the two groups, but the incidence of a low Apgar score at 1 min for twin B was significantly higher in twin newborns born vaginally than in those delivered by cesarean section. Moreover, the mean twin-to-twin delivery interval was significantly longer in twin pairs born vaginally than in those delivered by cesarean section.
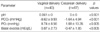
Table 2 presents inter-twin differences in umbilical arterial blood gas parameters according to the mode of delivery of twin A. Inter-twin differences in umbilical arterial blood pH, PCO2, PO2, and base excess in twin newborns born vaginally were significantly greater than the corresponding differences in those born by cesarean section. When analysis included twin newborns born vaginally, a significant positive correlation between twin-to-twin delivery interval and inter-twin differences in umbilical arterial blood pH was noted (r=0.504, p=0.001) (Fig. 1).
Table 3 shows the clinical characteristics of 14 cases where twin B was delivered more than 20 min after twin A. The umbilical arterial blood pH of twin B was less than 7.0 in 14% (2/14) of the cases delivered more than 20 min after twin A. Moreover, there were no cases of pathologic fetal academia (pH <7.0) when twin B was delivered within 20 min of twin A.
Of the 67 cases where twins were both delivered by cesarean section, 54 (81%) were delivered in the absence of labor, whereas the remaining 13 (19%) were delivered during the first or second stage of labor. No significant differences were observed between twin newborns delivered by cesarean section during the first or second stage of labor and those delivered in the absence of labor in terms of median inter-twin differences in umbilical arterial blood pH, PO2, and base excess. However, the inter-twin difference in umbilical arterial blood PCO2 was significantly greater in twin newborns born by cesarean section during the first or second stage of labor than in those born in the absence of labor (median -2.6, range -14.4-2.6 vs. median -1.25, range -13.3-9.1, p< 0.05, Mann-Whitney U test).
The results of our study suggest that umbilical arterial blood gas status of the second twin worsens with increasing twin-to-twin delivery interval, and that pathologic fetal acidemia may develop in the second twin when the twin-to-twin delivery interval is greater than 20 min. These results indicate that active intervention and prompt vaginal delivery of the second twin is necessary to minimize the second stage of delivery of the second twin. A similar observation was made in a population-based study in the setting of fetal distress and low Apgar scores for second twins (20).
Several investigators have reported that umbilical arterial blood gas status is poorer in second twins than in first twins (21-23), and the findings of the present study are consistent with these observations. Moreover, our data indicate that the reason why second twins are at increased risk of hypoxia is due to delayed delivery. The present study is unique in that the outcome variable chosen to draw this conclusion was intertwin difference in umbilical arterial blood gas parameters, rather than umbilical arterial blood gas parameters alone. To our knowledge, this is the first report comparing first twins' umbilical arterial blood gas parameters with those of second twins in the same pregnancy, which utilizes the first twin as a matched control for the second twin. Furthermore, we carefully selected a homogenous group of twin pregnancies without any maternal or fetal complications. Consequently, many of the confounding variables that might affect cord blood gas values, such as, labor, mode of delivery, and epidural anesthesia, were eliminated (24, 25).
Then why do second twins have a potentially greater susceptibility to hypoxia than first twins? After the delivery of a first twin, a sudden reduction in uterine volume may cause either constriction of the uterine vessel or partial separation of the placenta. This view is justified by observations made by other groups (26, 27), which indicated that uterine vascular resistance increases soon after delivery, and that lesser degrees of abruption might develop shortly before delivery of a single fetus when the amniotic fluid has drained from the uterus, the fetus has descended, and the fetal head is on the perineum. An alternative explanation is that the supine and lithotomy position assumed during the birth of the second twin is at increased risk of aortocaval compression, which in turn leads to a reduction in uteroplacental blood flow. Indeed the findings of Gupta and Hofmeyr (28) support this view, i.e., that the use of any upright or lateral position during the second stage of labor, as compared with the supine and lithotomy positions, is significantly associated with fewer abnormal fetal heart rate patterns. Regardless of the underlying cause for placental ischemia after the delivery of the first twin, our findings support the practice of close monitoring and the immediate vaginal delivery of the second twin.
A major finding reported herein is that a significant positive correlation was found between twin-to-twin delivery interval and inter-twin difference in umbilical arterial blood pH in twin newborns born vaginally. This finding is in keeping with the observation made by Leung et al. (29), who demonstrated a significant negative correlation between intertwin delivery interval and umbilical arterial blood pH and base excess of the second twin when delivered vaginally. These findings have important clinical implications because twin-to-twin delivery intervals are potentially under the control of the clinician. Importantly, these observations strongly support active intervention to complete the delivery of the second twin (i.e., oxytocin augmentation and amniotomy, if safe).
It is noteworthy that the present study indicates that pathologic fetal acidemia might develop in the second twin when the twin-to-twin delivery interval exceeded 20 min. This finding supports the traditional view that the inter-twin delivery interval should be preferably less than 15 min and certainly no more than 30 min (6-10). Similarly, Leung et al. reported that the umbilical arterial pH of the second twin was not less than 7.0 in any case delivered within 15 min of the birth of the first twin, and in 5.9% if within 16-30 min and in 27% if more than 30 min (29). Collectively, these observations suggest that the safest interval between delivery of the first and second twins is less than approximately 30 min and that shorter intervals may reduce the risk of fetal acidemia in the second twin. Then, given the above one might ask if the second twin is not delivered by the proposed inter-twin delivery interval time limit, whether or not he or she should proceed immediately with emergency cesarean delivery. However, the outcome of baby should not be assessed by cord blood gas analysis alone. A rigorous definition of severe birth asphyxia should include umbilical artery acidemia (pH <7.0), extremely low Apgar scores for longer than 5 min, the need for resuscitation at birth, and evidence of neonatal end-organ damage, such as, early seizures and cardiac or renal dysfunction (30, 31). In our study, two infants with a pH of less than 7.0 had a 5-min Apgar score of 7 or higher, and did not require resuscitation at birth, and were admitted to the regular newborn nursery. Even in the study by Leung et al. (29), where cord blood gas analysis alone was used to determine baby outcome, it was concluded that the 30-min limit was biochemically and clinically significant. In addition, several investigators have reported that a protracted birth interval is not associated with an adverse outcome provided that continuous, reassuring fetal monitoring is available throughout the inter-twin delivery interval (11, 14, 32, 33). On the basis of these careful observations, even though we do not object to setting an upper limit for the inter-twin delivery interval as a good clinical practice guideline, we believe that it is unwise to decide on cesarean section based entirely on a time limit without considering other favorable factors for the continuation of vaginal delivery, such as, the descent of the fetal head and a normal fetal heart rate pattern. Further large, prospective, randomized studies are required to solve this issue.
Inter-twin differences in umbilical arterial blood pH, PCO2, PO2, and base excess in twin newborns born vaginally were significantly greater than in twins born by cesarean section. Moreover, the incidences of a low Apgar score at 1 and 5 min for the first twin were not significantly different between twin newborns born vaginally and those delivered by cesarean section, but the incidence of a low Apgar score at 1 min for the second twin was significantly higher in twin newborns born vaginally than in those delivered by cesarean section. These findings suggest that cesarean delivery, in which babies are delivered within a few minutes of each other, benefits the second twin more than the first twin in terms of oxygen, pH, and base excess as well as Apgar score. However, the small differences in umbilical arterial blood pH and Apgar scores involved are not large enough to impact clinical management and therefore routine cesarean delivery for all vertex-vertex was not supported. Similarly, numerous observational reports have shown no benefit of cesarean over vaginal delivery with respect to any measure of neonatal morbidity or mortality when the first twin is vertex (34, 35).
This study has several limitations that mainly stem from its small sample size and retrospective study design. However, the degree of agreement between our data and those of other larger studies (20, 29, 36) is reassuring. In conclusion, our data suggest that the umbilical arterial gas status of the second twin worsens with increasing twin-to-twin delivery interval, and that pathologic fetal acidemia may develop in the second twin when the twin-to-twin delivery interval exceeds 20 min.
Figures and Tables
Fig. 1
Twin-to-twin delivery interval and inter-twin difference in umbilical arterial blood pH in twin newborns delivered vaginally. There was a significant positive correlation between twin-to-twin delivery interval and inter-twin difference in umbilical arterial blood pH (r=0.504, p=0.001).

Table 1
The demographic and clinical characteristics of the study population according to the mode of delivery of the first twin

References
1. Ho SK, Wu PY. Perinatal factors and neonatal morbidity in twin pregnancy. Am J Obstet Gynecol. 1975. 122:979–987.

2. McCarthy BJ, Sachs BP, Layde PM, Burton A, Terry JS, Rochat R. The epidemiology of neonatal death in twins. Am J Obstet Gynecol. 1981. 141:252–256.

3. Spellacy WN, Handler A, Ferre CD. A case-control study of 1253 twin pregnancies from a 1982-1987 perinatal data base. Obstet Gynecol. 1990. 75:168–171.
4. Gardner MO, Goldenberg RL, Cliver SP, Tucker JM, Nelson KG, Copper RL. The origin and outcome of preterm twin pregnancies. Obstet Gynecol. 1995. 85:553–557.

5. Smith GC, Pell JP, Dobbie R. Birth order, gestational age, and risk of delivery related perinatal death in twins: retrospective cohort study. BMJ. 2002. 325:1004–1008.

6. Ferguson WF. Perinatal mortality in multiple gestations: a review of Perinatal deaths from 1609 multiple gestations. Obstet Gynecol. 1964. 23:861–870.
9. Langer H. Perinatal mortality in twins. Zentralbl Gynakol. 1972. 94:1288–1296.
10. Farooqui MO, Grossman JH, Shannon RA. A review of twin pregnancy and perinatal mortality. Obstet Gynecol Surv. 1973. 28:144–153.

11. Rayburn WF, Lavin JP, Miodovnik M, Varner MW. Multiple gestation: Time interval between delivery of the first and second twins. Obstet Gynecol. 1984. 63:502–506.
12. Rydhstrom H, Ingemarsson I. Interval between birth of the first and the second twin and its impact on second twin perinatal mortality. J Perinat Med. 1990. 18:449–453.
13. Thompson SA, Lyons TL, Makowski EL. Outcome of twin gestations at the University of Colorado Health Science Center, 1973-1983. J Reprod Med. 1987. 32:328–339.
14. Chervenak FA, Johnson RE, Youcha S, Hobbins JC, Berkowitz RL. Intrapartum management of twin gestation. Obstet Gynecol. 1985. 65:119–124.
15. Sykes GS, Molloy PM, Johnson P, Gu W, Ashworth F. Do Apgar scores indicate asphyxia? Lancet. 1982. 1:494–496.

16. Nelson KB, Ellenberg JH. Apgar scores as predictors of chronic neurologic disability. Pediatrics. 1981. 68:36–44.
17. Freeman JM, Nelson KB. Intrapartum asphyxia and cerebral palsy. Pediatrics. 1988. 82:240–249.
18. Usta IM, Rechdan JB, Khalil AM, Nassar AH. Mode of delivery for vertex-nonvertex twin gestations. Int J Gynaecol Obstet. 2005. 88:9–14.

19. Chauhan SP, Roberts WE, McLaren RA, Roach H, Morrison JC, Martin JN Jr. Delivery of the nonvertex second twin: breech extraction versus external cephalic version. Am J Obstet Gynecol. 1995. 173:1015–1020.
20. Hartley RS, Hitti J. Birth order and delivery interval: analysis of twin pair perinatal outcomes. J Matern Fetal Neonatal Med. 2005. 17:375–380.

21. Brown HL, Miller JM Jr, Neumann DE, Sarpong DF, Gabert HA. Umbilical cord blood gas assessment of twins. Obstet Gynecol. 1990. 75:826–829.

22. Young BK, Suidan J, Antoine C, Silverman F, Lustig I, Wasserman J. Differences in twins: the importance of birth order. Am J Obstet Gynecol. 1985. 151:915–923.

23. Nakano R, Takemura H. Birth order in delivery of twins. Gynecol Obstet Invest. 1988. 25:217–222.

24. Yancey MK, Harlass FE. Extraneous factors and their influences on fetal acid-base status. Clin Obstet Gynecol. 1993. 36:60–72.

25. Yoon BH, Kim SW. The effect of labor on the normal values of umbilical blood acid-base status. Acta Obstet Gynecol Scand. 1994. 73:555–561.

26. Maymon R, Herman A, Halperin R, Bukovsky I, Weinraub Z, Ariely S. Changes in uterine artery Doppler flow velocity waveforms during the third stage of labor. Gynecol Obstet Invest. 1995. 40:24–27.

27. Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC, Hankins GD, Clark SL. Cunningham FG, MacDonald PC, Gant NF, Leveno KJ, Gilstrap LC, Hankins GD, Clark SL, editors. Obstetrical hemorrhage. Williams Obstetrics. 1997. 20th ed. Norwalk (CT): Appleton & Lange;745–782.
28. Gupta JK, Hofmeyr GJ. Position for women during second stage of labour. Cochrane Database Syst Rev. 2004. 1:CD002006.

29. Leung TY, Tam WH, Leung TN, Lok IH, Lau TK. Effect of twin-to-twin delivery interval on umbilical cord blood gas in the second twins. BJOG. 2002. 109:63–67.

30. American college of obstetricians and gynecologists. Committee Opinion, No. 174. Use and abuse of the Apgar score. 1996. July.
31. Gilstrap LC 3rd, Leveno KJ, Burris J, Williams ML, Little BB. Diagnosis of birth asphyxia on the basis of fetal pH, Apgar score, and newborn cerebral dysfunction. Am J Obstet Gynecol. 1989. 161:825–830.

32. Chauhan SP, Roberts WE. Gall SA, editor. Intrapartum management. Multiple pregnancy and delivery. 1996. St. Louis: Mosby-Year Book;243–280.
33. American College of Obstetricians and Gynecologists. Education Bulletin No. 253. Special problems of multiple gestation. 1998. November.
34. Laros RK Jr, Dattel BJ. Management of twin pregnancy: the vaginal route is still safe. Am J Obstet Gynecol. 1988. 158:1330–1338.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download