Abstract
The plasma ghrelin has been reported to be elevated in Prader-Willi syndrome (PWS) and modulated by insulin. It was hypothesized that insulin might have a more pronounced effect on reducing plasma ghrelin in PWS patients, which would influence appetite. This study investigated the degree of ghrelin suppression using an euglycemic hyperinsulinemic clamp in children with PWS (n=6) and normal children (n=6). After a 90-min infusion of insulin, the plasma ghrelin level decreased from a basal value of 0.86±0.15 to 0.58±0.12 ng/mL in the controls, and from 2.38±0.76 to 1.12±0.29 ng/mL in children with PWS (p=0.011). The area under the curve below the baseline level over the 90 min insulin infusion was larger in children with PWS than in controls (-92.82±44.4 vs. -10.41±2.87 ng/mL/90 min) (p=0.011). The insulin sensitivity measured as the glucose infusion rate at steady state was similar in the two groups (p=0.088). The decrease in the ghrelin levels in response to insulin was more pronounced in the children with PWS than in the controls. However, the level of ghrelin was always higher in the children with PWS during the clamp study. This suggests that even though insulin sensitivity to ghrelin is well maintained, an increase in the baseline ghrelin levels is characteristic of PWS.
Prader-Willi syndrome (PWS) is a contiguous gene syndrome resulting from the deletion of the paternal copies of the imprinted SNRPN gene and possibly other genes. The condition is characterized by diminished fetal activity, obesity, muscular hypotonia, mental retardation, short stature, hypogonadotropic hypogonadism, and uncontrollable hyperphagia (1-3).
Because neonates with PWS are profoundly hypotonic, hyporeflexia and poor feeding are often encountered due to diminished swallowing and sucking reflexes, which in many cases necessitates gavage feeding during the infantile period. These feeding difficulties generally improve by the age of 6 months. However, from 12 to 18 months onward, uncontrollable hyperphagia causes major somatic and psychological problems (4).
In contrast to infants, adolescents with PWS typically show insatiable hunger (5), and any attempt to reduce food intake in these adolescents often leads to serious psychological and behavioral problems with the home environment becoming intolerable in some children. Patients rarely survive beyond 25 to 30 yr of age due to diabetes and cardiac failure. However, strict weight control can greatly reduce the risk of both diabetes and cardiac failure and slightly affect survival (6). Therefore, proper weight control would substantially improve the quality of life and survival of both adolescents and adults with PWS.
Typically subjects with PWS eat for a longer time than obese or normal weight subjects. In PWS, it has been reported that 56% of the eating curves are non-decelerating, compared with 10% in the normal weight group and 30% in the obese group (7).
Ghrelin is a novel peptide that acts on the growth hormone (GH) secretagogue receptor in the pituitary and hypothalamus. Ghrelin also appears to play a role in energy homeostasis, which is a determinant of plasma ghrelin concentration because ghrelin acutely stimulates the appetite and GH secretion in rodents and humans, and the chronic administration to rodents causes obesity (8-11). The fasting plasma ghrelin levels are lower in obese subjects than in lean controls (12-14), and are elevated in patients with anorexia nervosa (14). Fasting increases the plasma ghrelin level, which then decreases after feeding (15-17). However, grossly elevated plasma ghrelin levels have been demonstrated in PWS adults (4) and children (6, 18), and recently, a 3- to 4- fold increase in the ghrelin levels was reported in PWS patients over a 24-hr period (18, 19).
Insulin is a physiologic and dynamic modulator of plasma ghrelin (20). The inhibitory effect of insulin on ghrelin secretion has been reported to be independent of glucose, even though glucose may have an additional effect (21, 22). Moreover, meal-related ghrelin suppression does not appear to be directly regulated by glucose or insulin (23).
Although the negative correlation between fasting ghrelin levels and obesity in non-PWS subjects may be the result of insulin resistance and hyperinsulinemia suppressing the secretion of ghrelin (21, 22), hyperghrelinemia in PWS cannot be solely explained by the reduced visceral adiposity and relative hypoinsulinemia (24). Therefore, insulin might profoundly lower plasma ghrelin levels, and influence appetite in patients with PWS.
The aim of this study was to clarify the relationship between plasma ghrelin and insulin and to evaluate the potential therapeutic benefit of using insulin to lower plasma ghrelin in children with PWS. Therefore, this study investigated the relationship between plasma ghrelin and insulin in children with PWS (n=6) and normal children (n=6), and compared the degree of ghrelin suppression using an euglycemic hyperinsulinemic clamp.
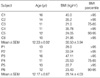
Six children with PWS (all male) aged 12.17±0.87 yr with a mean body mass index (BMI) of 29.14±4.03 kg/m2, and 6 age-, gender-, and BMI matched controls (males, 12.33±0.92 yr with a BMI of 30.50±3.94 kg/m2) were enrolled in this study (Table 1). The subjects were admitted to the Samsung Medical Center at Sungkyunkwan University the day before the clamp procedure. After a 10-hr overnight fast, an intravenous catheter was placed in the antecubital vein to infuse insulin and glucose. Another catheter was placed retrograde in the dorsal vein of the contralateral hand for blood withdrawal. The arm fitted with the insulin/glucose infusing catheter was placed in a heating pad to arterialize the blood. Regular human insulin (40 mIU/m2/min) was infused for two hours and a variable infusion of 20% dextrose was administered to maintain plasma glucose at the fasting level. Subsequently, the insulin infusion was discontinued and the 20% glucose infusion was gradually tapered to maintain the plasma glucose at the same level for another hour. During the procedure, arterial plasma glucose was measured every 5 min to guide the glucose infusion. Blood samples were collected at -15 min (before insulin infusion), and every 15 min during the next 180 min to monitor plasma insulin and ghrelin concentrations. The degree of ghrelin suppression was measured by the difference between 0 min and the measurement time. Insulin sensitivity was defined as glucose infusion rate required to maintain a basal plasma glucose concentration during the final 30 min (90-120 min) of the euglycemic clamp.
The Institutional Review Board approved the experimental protocol and informed consent was obtained from the parents of the patients and controls in all cases.
The plasma glucose was measured using a YSI model 2300 dual analyzer (Yellow Springs Instrument Co., Yellow Springs, OH). The plasma insulin was measured using a commercially available immuno-radiometric assay kit (BioSource Europe S.A.) with a detection limit of 1 uIU/mL and intra-, and inter-assay coefficients of variation of <10%. The plasma ghrelin levels were measured in duplicate using a commercial ELISA kit (Phoenix Pharmaceuticals, Belmont, CA). The inter- and intra-assay coefficients of variance were less than 10%. The lower and upper limits of detection for this assay were 0.75 ng/mL and 100 ng/mL.
All samples from a single participant were measured in the same assay.
The areas under the curve (AUC) below baseline were calculated using the trapezoid method. The AUCs are expressed as units per 90 or 120 min below each subject's fasting baseline level, and were compared using the Mann-Whitney test. The differences in the plasma ghrelin levels between 0 and 90 min in each subject were calculated, and the values from the two groups were compared using the Mann-Whitney test. The glucose infusion rates at steady state (90-120 min) were also compared between groups using the Mann-Whitney test. All statistical analyses were performed using SPSS software (SPSS Inc., Chicago, IL, U.S.A.). The data is expressed as the mean±SEM. p values <0.05 were considered significant.
The mean insulin level during insulin infusion (15 min to 120 min) in the control and PWS group was 92.09±6.36 mIU/mL and 81.48±3.21 mIU/mL, respectively, which was not significantly different (Fig. 1). The plasma ghrelin level in the control and PWS groups over the 90 min period of insulin infusion was reduced from a basal value of 0.86±0.15 to 0.58±0.12 ng/mL and 2.38±0.76 to 1.12±0.29 ng/mL, respectively. The plasma ghrelin levels were relatively constant at these reduced levels until 15 min after the insulin infusion had been discontinued (Fig. 2, 3).
The plasma ghrelin level was suppressed maximally at 90 min after insulin infusion by 26.81±4.66% in the controls and by 47.95±5.15% in the PWS group (Fig. 2, 3). The degree of ghrelin suppression was higher in the PWS group after the 90 min infusion of insulin infusion than in the control (p=0.011) (Fig. 3). However, the ghrelin levels in the PWS patients were not suppressed to a level lower that of the control during the study period (Fig. 2).
The AUC below baseline was higher for the PWS group than in the control during the 90 min of insulin infusion (-92.82±44.4 vs. -10.41±2.87 ng/mL/90 min) (p=0.011) and during the entire insulin infusion period of 120 min (-130.17±59.51 vs. -16.54±4.04 ng/mL/120 min) (p=0.011) (Fig. 4).
The mean glucose infusion rate at steady state (90-120 min) in the PWS patients (5.93±0.93 mg/kg/min) was higher than in the controls (2.59±1.17 mg/kg/min), but this was not significant (p=0.088) (Fig. 5).
The insulin-induced suppression of ghrelin was more profound in the children with PWS after the 90-min infusion of insulin than in the controls even though the mean insulin level was similar in both groups. Therefore, at a given insulin level, the plasma level of ghrelin was reduced more effectively in the children with PWS than in the normal controls. However, it should be noted that the lowest ghrelin level in the PWS group was always higher than in the control group at the corresponding times during the study period. The results of this clamp study are reminiscent of those of a previous 24-hr monitoring study as far as the relationship between ghrelin and insulin are concerned.
In a previous study when insulin and ghrelin were monitored for 24 hr, the peak plasma ghrelin level in the children with PWS was 3-4 times higher than in the normal control, while the peak plasma insulin levels in the children with PWS was similar to that in the controls. After meals, the peaked ghrelin level returned to the baseline in both PWS and control groups. However, the baseline level of ghrelin was always higher in the children with PWS (17).
Recently, it was demonstrated that in the gastric body and fundus, there were 2 to 3 fold increases in the number of ghrelin expressing cells (GECs) (p<0.001) and in the amount of ghrelin (p<0.018) in PWS patients compared with the control groups. Therefore, the baseline increase in ghrelin might be related to the hyperplasia of GECs, which means that the absolute increase in the number of GECs might be related to the baseline increase in the ghrelin level in this study (25).
Overall, the increase in the basal ghrelin levels is a prominent finding in this study and the decrease in ghrelin in response to insulin was more pronounced in the children with PWS than in the controls.
Although the direct orexigenic effect of ghrelin in its physiologic concentration range has not been elucidated in rodents or humans, the link between insulin and ghrelin was demonstrated in type I diabetes patients (26). It was shown that insulin is essential for meal-induced plasma ghrelin suppression, and that basal insulin availability is sufficient to suppress postprandial ghrelin in type 1 diabetic patients. It was concluded that the lack of meal-induced ghrelin suppression caused by a severe insulin deficiency might explain the hyperphagia in uncontrolled type 1 diabetic subjects. Interestingly, the hyperphagia in uncontrolled type 1 diabetics is similar to the incessant eating of PWS patients. Excessive eating in both diseases is associated with an elevated plasma ghrelin level, and a physiologic amount of insulin can effectively suppress the surge in ghrelin within an hour. These results also demonstrate that insulin plays a key role in regulating the postprandial ghrelin concentrations. Therefore, insulin might be a decisive signal that ensures postprandial plasma ghrelin suppression in both diseases. However, insulin-induced ghrelin suppression is more pronounced in PWS patients than in uncontrolled diabetes patients, and the nadir of ghrelin suppression is also higher in PWS patients.
It is evident that ghrelin is released by the consumption of carbohydrate-rich meals, and that a decrease in the plasma ghrelin level is paralleled by an increase in plasma insulin level (13, 16, 17, 27). Supportive evidence on the inhibitory role of insulin on ghrelin secretion was provided by three studies (20-22). On the other hand, two other studies denied the role of insulin in ghrelin control (23, 28). The data in the present study are in line with the data reported in references 20-22, i.e., ghrelin was suppressed by insulin was observed while maintaining euglycemia using an euglycemic clamp technique. Therefore, the suppression of ghrelin appears to be due to insulin, not glucose. Moreover, an increase in the ghrelin level in the absence of hyperglycemia can contribute to the attenuation of postprandial release of insulin, which is supported by several studies (29-31).
Negative relationships have been observed between fasting ghrelin and the measures of insulin resistance (24). Goldstone et al. reported that a selected reduction in visceral adiposity in PWS patients has protective effect against the adverse metabolic consequences of obesity, such as insulin resistance (24). In the present study, an increasing tendency was found with respect to the glucose infusion rate at steady state in PWS patients but this was not significant. However, the lack of significance might have been due to the small number of cases examined.
In conclusion, the insulin-induced suppression of ghrelin was found to be more pronounced in the children with PWS than in the normal controls. Moreover, the baseline levels of ghrelin in the children with PWS were always higher than those of the controls. This suggests that even though insulin sensitivity to ghrelin is well maintained in PWS patients, the increase in the baseline levels of the ghrelin is a characteristic finding of PWS. It appears that the regulatory mechanisms of ghrelin are different in PWS patients, which might be of physiological importance in the obesity associated with PWS. However, more study will be needed to determine the precise regulatory mechanism of ghrelin in normal children and children with PWS.
Figures and Tables
Fig. 1
The mean insulin level during the insulin infusion (15 min to 120 min) in the control and PWS group was 92.09±6.36 mIU/mL and 81.48±3.21 mIU/mL, respectively, which was not statistically different.

Fig. 2
The plasma ghrelin level in the control and PWS groups over the 90 min period of insulin infusion was reduced from a basal value of 0.86±0.15 to 0.58±0.12 ng/mL and 2.38±0.76 to 1.12±0.29 ng/mL, respectively. The plasma ghrelin levels were relatively constant at these reduced levels until 15 min after the insulin infusion had been discontinued. The plasma ghrelin level was suppressed maximally at 90 min after insulin infusion. The plasma ghrelin levels in PWS patients were not suppressed to a level lower that of the control during the study period.

Fig. 3
The plasma ghrelin level was suppressed maximally at 90 min after insulin infusion by 26.81±4.66% in the controls and by 47.95±5.15% in the PWS group. The degree of ghrelin suppression was higher in the PWS group after the 90 min infusion of insulin infusion than in the control (p=0.011).

Fig. 4
The area under the curve (AUC) below the baseline was higher for the PWS group than in the control during the 90 min of insulin infusion (-92.82±44.4 vs. -10.41±2.87 ng/mL/ 90 min) (p=0.011) and during the entire insulin infusion period of 120 min (-130.17±59.51 vs. -16.54±4.04 ng/mL/120 min) (p=0.011).

References
1. Ishikawa T, Kibe T, Wada Y. Deletion of small nuclear ribonucleoprotein polypeptide N (SNRPN) in Prader-Willi syndrome detected by fluorescence in situ hybridization: two sibs with the typical phenotype without a cytogenetic deletion in chromosome 15q. Am J Med Genet. 1996. 62:350–352.

2. MacDonald HR, Wevrick R. The necdin gene is deleted in Prader-Willi syndrome and is imprinted in human and mouse. Hum Mol Genet. 1997. 6:1873–1878.

3. Prader A, Labhart A, Willi H. Ein Syndrom von Adipositas, Kleinwuchs, Kryptorchismus und Oligophrenie nach Myatonieartigem Zustand im Neugeborenenalter. Schweiz Med Wochenschr. 1956. 86:1260–1261.
4. Butler MG, Meaney FJ. An anthropometric study of 38 individuals with Prader-Labhart-Willi syndrome. Am J Med Genet. 1987. 26:445–455.

5. Greenswag LR. Adults with Prader-Willi syndrome: a survey of 232 cases. Dev Med Child Neurol. 1987. 29:145–152.

6. Curfs LM, Verhulst FC, Fryns JP. Behavioral and emotional problems in youngsters with Prader-Willi syndrome. Genet Couns. 1991. 2:33–41.
7. Lindgren AC, Barkeling B, Hagg A, Ritzen EM, Marcus C, Rossner S. Eating behavior in Prader-Willi syndrome, normal weight, and obese control groups. J Pediatr. 2000. 137:50–55.

8. Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999. 402:656–660.

9. Nakazato M, Murakami N, Date Y, Kojima M, Matsuo H, Kangawa K, Matsukura S. A role for ghrelin in the central regulation of feeding. Nature. 2001. 409:194–198.

10. Tschop M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature. 2000. 407:908–913.

11. Wren AM, Seal LJ, Cohen MA, Brynes AE, Frost GS, Murphy KG, Dhillo WS, Ghatei MA, Bloom SR. Ghrelin enhances appetite and increases food intake in humans. J Clin Endocrinol Metab. 2001. 86:5992.

12. Tschop M, Weyer C, Tataranni PA, Devanarayan V, Ravussin E, Heiman ML. Circulating ghrelin levels are decreased in human obesity. Diabetes. 2001. 50:707–709.

13. Shiiya T, Nakazato M, Mizuta M, Date Y, Mondal MS, Tanaka M, Nozoe S, Hosoda H, Kangawa K, Matsukura S. Plasma ghrelin levels in lean and obese humans and the effect of glucose on ghrelin secretion. J Clin Endocrinol Metab. 2002. 87:240–244.

14. Jo DS, Lee JU, Kim SY, Kang CW, Hwang PH, Lee DY. Plasma ghrelin levels and its relationship with obesity in obese children. J Korean Soc Pediatr Endocrinol. 2004. 9:179–185.
15. Ariyasu H, Takaya K, Tagami T, Ogawa Y, Hosoda K, Akamizu T, Suda M, Koh T, Natsui K, Toyooka S, Shirakami G, Usui T, Shimatsu A, Doi K, Hosoda H, Kojima M, Kangawa K, Nakao K. Stomach is a major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab. 2001. 86:4753–4758.

16. Tschop M, Wawarta R, Riepl RL, Friedrich S, Bidlingmaier M, Landgraf R, Folwaczny C. Post-prandial decrease of circulating human ghrelin levels. J Endocrinol Invest. 2001. 24:RC19–RC21.

17. Cummings DE, Purnell JQ, Frayo RS, Schmidova K, Wisse BE, Weigle DS. A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes. 2001. 50:1714–1719.

18. Jin DK. Ghrelin in the Prader-Willi Syndrome. J Korean Soc Pediatr Endocrinol. 2003. 8:119–125.
19. Paik KH, Jin DK, Song SY, Lee JE, Ko SH, Song SM, Kim JS, Oh YJ, Kim SW, Lee SH, Kim SH, Kwon EK, Choe YH. Correlation between fasting plasma ghrelin levels and age, body mass index (BMI), BMI percentiles, and 24-hour plasma ghrelin profiles in Prader-Willi syndrome. J Clin Endocrinol Metab. 2004. 89:3885–3889.

20. Saad MF, Bernaba B, Hwu CM, Jinagouda S, Fahmi S, Kogosov E, Boyadjian R. Insulin regulates plasma ghrelin concentration. J Clin Endocrinol Metab. 2002. 87:3997–4000.

21. Mohlig M, Spranger J, Otto B, Ristow M, Tschop M, Pfeiffer AF. Euglycemic hyperinsulinemia, but not lipid infusion, decreases circulating ghrelin levels in humans. J Endocrinol Invest. 2002. 25:RC36–RC38.

22. Flanagan DE, Evans ML, Monsod TP, Rife F, Heptulla RA, Tamborlane WV, Sherwin RS. The influence of insulin on circulating ghrelin. Am J Physiol Endocrinol Metab. 2003. 284:E313–E316.

23. Schaller G, Schmidt A, Pleiner J, Woloszczuk W, Wolzt M, Luger A. Plasma ghrelin concentrations are not regulated by glucose or insulin: a double-blind, placebo-controlled crossover clamp study. Diabetes. 2003. 52:16–20.

24. Goldstone AP, Thomas EL, Brynes AE, Castroman G, Edwards R, Ghatei MA, Frost G, Holland AJ, Grossman AB, Korbonits M, Bloom SR, Bell JD. Elevated fasting plasma ghrelin in prader-willi syndrome adults is not solely explained by their reduced visceral adiposity and insulin resistance. J Clin Endocrinol Metab. 2004. 89:1718–1726.

25. Choe YH, Song SY, Paik KH, Oh YJ, Chu SH, Yeo SH, Kwon EK, Kim EM, Rha MY, Jin DK. Increased density of ghrelin-expressing cells in the gastric fundus and body in Prader-Willi syndrome. J Clin Endocrinol Metab. 2005. 90:5441–5445.

26. Murdolo G, Lucidi P, Di Loreto C, Parlanti N, De Cicco A, Fatone C, Fanelli CG, Bolli GB, Santeusanio F, De Feo P. Insulin is required for prandial ghrelin suppression in humans. Diabetes. 2003. 52:2923–2927.

27. Kim SY, Shin JY, Jung MJ, Choi BM, Lee JH, Lee KH. Relationship between serum ghrelin and insulin resistance in obese children and adolescents. J Korean Soc Pediatr Endocrinol. 2005. 10:211–217.
28. Caixas A, Bashore C, Nash W, Pi-Sunyer F, Laferrere B. Insulin, unlike food intake, does not suppress ghrelin in human subjects. J Clin Endocrinol Metab. 2002. 87:1902.

29. Broglio F, Koetsveld Pv P, Benso A, Gottero C, Prodam F, Papotti M, Muccioli G, Gauna C, Hofland L, Deghenghi R, Arvat E, Van Der Lely AJ, Ghigo E. Ghrelin secretion is inhibited by either somatostatin or cortistatin in humans. J Clin Endocrinol Metab. 2002. 87:4829–4832.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download