Abstract
Lichen nitidus (LN) is an uncommon chronic inflammatory skin disease composed of numerous, tiny, shiny, flesh-colored papules that are predominantly observed on the chest, abdomen, glans penis and upper extremities. The distribution of LN is most often localized, but in some cases it can become generalized. Because LN tends to be asymptomatic and presents spontaneous resolution within several years, it usually does not require treatment except in symptomatic, persistent and generalized cases. We describe a 28-yr-old man and a 7-yr-old boy with generalized LN where both cases improved with narrow-band ultraviolet B (NB-UVB) phototherapy plus topical steroid ointment. Both patients noted improvement within the first three treatments and showed almost complete resolution after 18 and 20 treatments, respectively. NB-UVB phototherapy may be an effective alternative therapy for the treatment of generalized LN, even for those patients in their childhood.
Lichen nitidus (LN) is a chronic inflammatory disorder that is characterized by numerous, 1-2 mm sized, flesh to pink-colored papules. Usually the lesions are asymptomatic but pruritus can occur. LN preferentially involves the abdomen, chest, penis and the flexural surfaces of the extremites. The tiny papules tend to be localized, although the eruption can be generalized (1). Although LN tends to be asymptomatic and usually resolves spontaneously in a year, the clinical course of the generalized form is unpredictable. Many therapeutic modalities including topical or systemic corticosteroid, astemizole, psoralen ultraviolet A (PUVA) and dinitrochlorobenzene immunotherapy have been attempted for the purpose of treating generalized LN; however, there is no effective or tolerable treatment enough to treat the generalized LN of children.
We describe here two patients with generalized lichen nitidus whose lesions were rapidly improved with narrow-band ultraviolet B (NB-UVB) irradiation plus topically applied steroid.
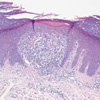
A 28-yr-old man had a 10-yr history of asymptomatic pinhead-sized papules that involved the trunk, upper extremities and palms including the fingers. The lesions first appeared on the abdomen and gradually spread over the chest and extremities. The physical examination showed multiple, discrete, 1 to 2 mm sized, flesh-colored papules on the abdomen, trunk and extremities, especially on the flexural surfaces and palms (Fig. 1A). No nail or mucosal involvement were found. The biopsy specimens from the abdomen and finger showed a focal well-circumscribed infiltrate of lymphocytes and histiocytes closely attached to the epidermis. The overlying epidermis was flattened and the granular layer was absent. The rete ridges on the margins of the granuloma were elongated to create the image of a 'claw clutching a ball' (Fig. 2). On the basis of the clinical and histopathologic findings, he was diagnosed with generalized lichen nitidus. A trial of NB-UVB phototherapy twice a week was initiated at 0.25 J/cm2, along with the application of topical methylprednisolone aceponate 0.1% ointment. The skin lesions of abdomen flattened after only 3 treatment sessions, and the majority of the lesions completely cleared after 20 sessions with a cumulative dose of 5.36 J/cm2 (Fig. 1B). Not surprisingly, the truncal lesions cleared before the acral ones. After a further 12-month period without treatment, there has been no recurrence at any site.
A 7-yr-old boy is herein presented with an asymptomatic flesh-colored glistening papular eruption that had been present on the trunk for 9 months. The lesions had gradually progressed until they were almost generalized. He also suffered from atopic dermatitis and allergic rhinitis. A physical examination revealed numerous dome-shaped shiny papules predominantly on the trunk, the extensor surface of the upper limbs and the postauricular area (Fig. 3A). A skin biopsy from the elbow revealed a well-circumscribed lymphohistiocytic infiltrate in the papillary dermis, which was surrounded bilaterally by elongated rete ridges; all of which constituted the typical configuration of lichen nitidus. Thus, he was diagnosed with generalized lichen nitidus. The patient also received NB-UVB phototherapy twice a week with the initial dose of 0.15 J/cm2. After 3 sessions of NB-UVB phototherapy, the papules on the anterior chest started to decrease in size and they were almost completely resolved after the eighteenth treatment, with a cumulative dose of 3.05 J/cm2 (Fig. 3B). The patient has been followed up on for 1 yr with no evidence of lesion recurrence.
Since LN is usually asymptomatic and resolves without sequelae, no treatment is necessarily required in most cases. However, medical treatment is required when the lesions are persistant, generalized, and when they are considered cosmetically undesirable or accompanied by symptoms such as pruritus. Many therapeutic modalities including topical and systemic corticosteroid, PUVA (2), ultraviolet A/ultraviolet B (UVA/UVB) with systemic corticosteroid (3), dinitrochlorobenzene (DNCB) or diphenylcyclopropenone immunotherapy (4), selective H1 antagonist (5), and even itraconazole (6) and isoniazide (7) have been used to treat LN patients. Especially, PUVA therapy and astemizole have been effective for generalized LN, whereas acitretin demonstrated a reduction in the palmoplantar forms (8). However, the application of etretinate, actiretin, PUVA and DNCB seems to be contraindicated for children. There are only a few reports about phototherapy for LN. Randle and Sander (2) treated a 29-yr-old woman with generalized LN with PUVA scheduled 3 times/week. She was completely responsive to the therapy, with an initial response being seen at the 27th treatment and the lesions going into complete remission after the 46th treatment with a total dose of 290 J/cm2. Chen et al. (3) described an 80-yr-old woman with generalized LN that was successfully treated with UVA/UVB combined with low-dose systemic prednisolone. Since NB-UVB (311 nm, TL-01) has fewer sideeffects and less carcinogenic potential than broadband UVB or PUVA, it has recently been used for almost every type of dermatosis which is known to be efficiently treated with PUVA (9). As seen in the above cases, since NB-UVB provides a lower cumulative dose than PUVA for disease remission, it seems to be safe and usable for children.
Although the exact mechanism of NB-UVB phototherapy in LN is unknown, the functional impairment of cellular immunity is thought to play a central role. The pathophysiology of LN suggests that an allergen may cause antigen-presenting cell (e.g. the Langerhans cell) to activate a cell-mediated response. It initiates the lymphocyte accumulation and forms the discrete inflammatory papules that contain large numbers of Langerhans cells. The cutaneous immunologic effects of NB-UVB therapy are to deplete the number of epidermal Langerhans cells, as measured by CD-1a expression, and to induce the production of anti-inflammatory factors like interleukin-10, alpha-melanocyte stimulating hormone and prostaglandin E2, in addition to down-regulating the expression of intercellular adhesion molecule-1 (9).
The effectiveness of systemic therapy for LN is difficult to evaluate because of the propensity for the disease being resolved spontaneously. However the generalized and persistent lesions observed in case 1 were relatively resolved after only three sessions of NB-UVB irradiation. Thus, it is most probable that the NB-UVB phototherapy was responsible for their resolution.
We conclude that NB-UVB phototherapy is an effective alternative treatment for generalized LN, even for children to whom physicians are generally hesitant to prescribe systemic or potent topical steroid and PUVA.
Figures and Tables
Fig. 1
(A) Numerous flesh-colored, flat, shiny papules are distributed on the abdomen. (B) After only 3 sessions of NB-UVB irradiation, the papules show marked flattening.

References
1. Lapins NA, Willoughby C, Helwig EB. Lichen nitidus: A study of forty-three cases. Cutis. 1978. 21:634–637.
2. Randle HW, Sander HM. Treatment of generalized lichen nitidus with PUVA. Int J Dermatol. 1986. 25:330–331.

3. Chen W, Schramm M, Zouboulis CC. Generalized lichen nitidus. J Am Acad Dermatol. 1997. 36:630–631.

4. Lee SD, Kim MY, Baek SC, Houh D, Byun DG. Two cases of lichen nitidus treated with diphenylcyclopropenone immunotherapy. Korean J Dermatol. 2001. 39:1432–1434.
5. Ocampo J, Torne R. Generalized lichen nitidus -report of two cases treated with astemizole. Int J Dermatol. 1989. 28:49–51.
6. Libow LF, Coots NV. Treatment of lichen planus and lichen nitidus with itraconazole. Cutis. 1998. 62:247–248.
7. Kubota Y, Kiryu H, Nakayama J. Generalized lichen nitidus successfully treated with an antituberculous agent. Br J Dermatol. 2002. 146:1081–1083.

8. Lucker GP, Koopman RJ, Steijlen PM, Valk PG. Treatment of palmoplantar lichen nitidus with acitretin. Br J Dermatol. 1994. 130:791–793.

9. El-Ghorr AA, Norval M. Biological effects of narrow-band (311nm TL01) UVB irradiation. a review. J Photochem Photobiol B. 1997. 38:99–106.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download