Abstract
The goal of this study was to compare the effects of different reperfusion methods on N-terminal B-type natriuretic peptide (NT-proBNP) in percutaneous transluminal coronary angioplasty (PTCA) or off-pump coronary artery bypass (OPCAB) patients. Fifty subjects were enrolled in the study, 32 patients received PTCA and 18 OPCAB. An NT-proBNP measurement was performed before intervention and at 1, 3, and 7 days after the procedures. NT-proBNP levels were not significantly different before intervention (PTCA group 297±147.3 vs. OPCAB group 235±167.8 pg/mL, p>0.05). However, 1 day after the procedures, NT-proBNP levels were higher in the OPCAB group (PTCA 375±256.4 vs. OPCAB 1,415±737.6 pg/mL, p<0.05), after 3 days NT-proBNP reached peak levels (PTCA 480±363.0 vs. OPCAB 2,119±818.4 pg/mL, p<0.05), and levels were reduced after 7 days (PTCA 292±243.7 vs. OPCAB 522±334.0 pg/mL, p>0.05). PTCA induced a mild and transient increase in NT-proBNP concentration, but OPCAB caused sustained high NT-proBNP levels during the 7 day postoperatively. However, differences between NT-proBNP levels associated with these two modalities showed a tendency to decrease rapidly postoperatively.
B-type natriuretic peptide (BNP) has been isolated from porcine brain, and shares remarkable sequence homology with and has physiologic effects similar to atrial natriuretic peptide (ANP) (1). Under conditions of sustained ventricular expansion and volume overload, proBNP is released into blood, where it is cleaved into BNP, the physiologically active hormone, and an N-terminal fragment (NT-proBNP), an inactive metabolite (2). Therefore, increased plasma concentrations of proBNP, BNP and NT-proBNP are markers of left ventricular systolic dysfunction since they are synthesized and secreted primarily by the myocardium during a period of increased work (3). More recently, plasma BNP concentrations have been reported to be increased after acute myocardial infarction (4) and in patients presenting with acute coronary syndromes (5).
Percutaneous transluminal coronary angioplasty (PTCA) and coronary artery bypass grafting (CABG) are widely used to treat ischemic heart disease; however, it has been reported that these procedures can increase plasma BNP (6, 7). It was reported that PTCA increases BNP levels mildly and transiently, but that CABG with cardioplegic arrest causes major tissue injury and persistently high hormonal levels (8). Therefore, plasma BNP might act as a myocardial stress marker after the coronary artery reperfusion. However, little data comparative information is available about NT-proBNP behavior immediately after coronary artery angioplasty or bypass without cardiopulmonary bypass (CPB). Thus this study was undertaken to compare the effects of different reperfusion methods on plasma NT-proBNP in patients with coronary artery disease who received PTCA or off-pump coronary artery bypass (OPCAB).
From December 2003 to December 2004, all patients were evaluated for functional angina class according to the Canadian Classification, and for heart failure status according to the New York Heart Association classification. All patients received a pre-operative echocardiographic examination to evaluate left ventricular systolic function, and all had one or more compromised vessels with stenosis exceeding 70% of the luminal diameter of a major coronary artery by selective coronary angiography.
Patients were excluded if they fulfilled one or more following criteria: 1) significant valvular heart disease; 2) previous myocardial infarction or unstable angina; 3) acute or chronic heart failure; 4) cardiomyopathy; 5) left ventricular aneurysm or hypertrophy; 6) systolic dysfunction with an ejection fraction of <45%; 7) perioperative myocardial infarction; and 8) a renal or a hepatic pathology. The protocol used was approved by our hospital's ethics committee and all patients provided written informed consent prior to participating in the study.
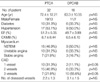
The subjects were 50 patients, 30 men and 20 women (mean age 68.7±12.2, range 46 to 88 yr) with coronary artery disease and underwent elective PTCA or OPCAB at Korea University Medical Center. Thirty-two of the patients were received PTCA and 18 OPCAB (Table 1). Mean patient age was marginally higher in PTCA group than in OPCAB group (p=NS), and the number of diseased coronary arteries tended to be greater in the OPCAB group (p=NS). One vessel disease was more common in the PTCA group and three vessels disease in OPCAB group. No significant difference was observed between the two groups in terms of combined diseases, ejection fraction (EF), or myocardium status.
Blood samples for NT-proBNP measurements were taken within 24 hr before and 1, 3, and 7 days after the procedures. Blood (15 mL) samples were taken from an antecubital vein and distributed in tubes containing ethylenediaminetetraaceticacid (EDTA). The specimens were then centrifuged for less than 1 hr, and the plasma obtained was frozen at -80℃ until analysis. NT-proBNP was measured using a double antibody sandwich technique and electrochemiluminescence immunoassay (Elecsys proBNP, Roche Diagnostics, Mannheim, Germany), the intra-assay coefficient of variation was <6% at both normal and elevated levels. Normal subject reference values are dependent on age and sex; mean values vary from 88 pg/mL in men under 50 yr of age to 334 pg/mL in women between 50 and 65 yr of age (data from manufacturer).
In the PTCA group, coronary balloon angioplasty and stent implantation was performed in fasted patients using standard techniques. In all PTCA patients sirolimus-eluting stents (Cyper®, Cordis, a Johnson & Johnson company, Roden, The Netherlands) or paclitaxel-eluting stents (Taxus®, Boston Scientific Corporation, Galway, Ireland) were used. High-pressure balloon inflation was used in order to avoid stent underexpansion.
In the OPCAB group, anesthetic technique is predicated upon the avoidance of high-dose narcotics and the use of short- and intermediate-acting anesthetic agents. During the operation, continuous nitroglycerine and intermittent esmolol infusion were used for ischemic prophlyaxis and slowing the heart rate. During the cardiac manipulation, the decreased pump function was managed by volume overloading and use of Trendelenberg positioning. The left internal mammary artery (IMA) was attached to the left anterior descending artery, and right IMA or saphenous vein grafts to other coronary arteries as appropriate in all patients. Distal end anastomosis was constructed with the help of an intracoronary shunt (AXIUS™, Guidant Co. Cardiac Surgery, CA, U.S.A.). Stabilization of the target coronary artery was accomplished using the Genzyme Immobilizer™ system (Genzyme Corp., MA, U.S.A.).
The patients were divided in two groups according to the reperfusion procedure used and groups were compared by the Mann-Whitney test. Changes in the plasma levels of NT-proBNP were investigated by a nonparametric repeated measure of analysis of variance (Friedman test) within a group and by the Mann Whitney test across groups on the same day; all values are expressed as means±S.D. Linear regression analysis was used to assess the relation between NT-proBNP levels and the various parameters. Statistical analyses were performed using Statistica 6.0 (Statsoft Tulsa, OK, U.S.A.), and p values of <0.05 were considered statistically significant.
The number of reperfused coronary arteries was significantly greater in the OPCAB group (PTCA group 1.5±0.6 vs. OPCAB group 3.2±1.3, p<0.05). No hospital mortality occurred in either group.
NT-proBNP levels in the two groups were not significantly different before intervention (PTCA group 297±147.3 pg/mL vs. OPCAB group 235±167.8 pg/mL, p=NS). One day after PTCA or OPCAB, NT-proBNP levels were higher in the OPCAB group than in the PTCA group (PTCA group 375±256.4 pg/mL vs. OPCAB group 1,415±737.6 pg/mL, p<0.05) and after 3 days, NT-proBNP concentrations peaked in both groups and the difference between the two had widened (PTCA group 480±363.0 pg/mL vs. OPCAB group 2,119±818.4 pg/mL, p<0.05). However, a reducing temporal trend of NT-proBNP values was observed in both groups after 7 days and no significant difference was apparent between the two groups (PTCA group 292±243.7 pg/mL vs. OPCAB group 522±334.0 pg/mL, p=NS) (Fig. 1).
Cardiac natriuretic peptides are being used as diagnostic and prognostic markers in a variety of cardiovascular conditions, e.g., hypertension, congestive heart failure, and acute coronary syndrome, because of their unique characteristics and their role in cardiovascular physiology (9). Moreover, recent reports have shown that BNP concentrations increase during uncomplicated coronary angioplasty despite stable cardiac filling pressures, and during nuclear stress testing in patients with stable coronary heart disease (6). The underlying mechanism of elevated BNP secretion has been suggested to be transient myocardial hypoxia induced by coronary artery occlusion, which inevitably is introduced by such procedures. Under these conditions BNP stimulation may be due to the augmented regional wall stretch occurred by ischemic attacks even in the absence of pump dysfunction (10), or the source of BNP appears to be ischemic and necrotic tissue (6, 11).
In addition, many authors have presented evidence that plasma BNP concentrations become acutely elevated after conventional CABG and that this elevation reflects left ventricular function (12-14).
Palazzuoli et al. reported that PTCA increases BNP levels mildly and transiently, but that conventional CABG causes major tissue injury and persistently high hormonal levels (8). However, CPB in conventional CABG was found to cause an increase in circulating catecholamines and endothelins, and to augment oxidative stress, electrolyte imbalance and coagulative cascade activation, and to increase inflammatory molecule levels (15). These results suggest that the gene expression, metabolism, and biological activity of BNP may be altered after extracorporeal circulation. Moreover, Bail et al. reported that a postoperative peak BNP at 24 hr does not reflect a state of acute perioperative heart failure or myocardial damage (12).
In the present study we compared effects on NT-proBNP concentration according to reperfusion methods (PTCA and OPCAB) in patients with CAD without CPB. NT-proBNP has the comparable clinical utility because of the longer half life, lower intra-individual variation and better in vitro stability comparing to BNP (16).
We found that NT-proBNP levels were higher in the OPCAB group than in the PTCA. Some authors have inferred that events such as general anesthesia, cardiac herniation, stabilizer compression, blood flow blockage, reperfusion injury, and systemic inflammation can cause substantial stress (17, 18). In addition, OPCAB can cause direct myocardial manipulation, fluid overload to meet blood loss and rather longer operation time which can be stress to myocardium.
In addition, we did not compare the OPCAB group with non-cardiac surgical group. However, Tayama et al. said that BNP may be associated with the right ventricular dysfunction noted after pneumonectomy, owing to the decrease in the volume of the pulmonary vascular bed (19). Therefore, it was inferred that the non-cardiac surgery without damaging right ventricular function might not affect plasma BNP concentration.
In our hospital, during OPCAB we used a temporary intracoronary shunt which resulted in reduced acute ischemia and wall motion abnormalities, and maintained left ventricular function comparing to the occlusion technique (20). Palazzuoli et al. demonstrated lowering of the BNP levels after 90 days, but the difference between on-pump CABG and PTCA groups was still significant (8). In the present study, NT-proBNP level in OPCAB group was so rapidly decreased that there was no difference between two groups in the 7 days postoperatively. These results revealed that OPCAB leads to sustained elevations of NT-proBNP relative to that observed with PTCA, and in addition, cardiopulmonary bypass can be a major factor to increase and keep the BNP level high for longer postoperative period.
In conclusion, PTCA was found to induce a mild and transient increase in NT-proBNP concentration, whereas OPCAB induced sustained high hormonal levels during the 7 day postoperative period, which does not mean that OPCAB damages the myocardium more severely. In this study, we do not measure any other specific biochemical markers of myocardial damage including creatinine kinase MB isoforms, troponin-T, and myoglobin. Therefore, other specific cardiac markers should be added for NT-proBNP to act as a myocardial stress marker.
Because our study was based on a short time interval, we did not evaluate the relations between temporal changes in the levels of these hormones and long-term prognosis, or between the overall impact of the procedure and mortality, for which longitudinal studies are advisable in a larger group of patients. The major limitation of this study is that relatively small patients were included.
Figures and Tables
References
1. Sudoh T, Kangawa K, Minamino N, Matsuo H. A new natriuretic peptide in porcine brain. Nature. 1988. 332:78–81.

3. Cowie MR, Struthers AD, Wood DA, Coats AJ, Thompson SG, Poole-Wilson PA, Sutton GC. Value of natriuretic peptides in assessment of patients with possible new heart failure in primary care. Lancet. 1997. 350:1349–1353.

4. Richards AM, Nicholls MG, Yandle TG, Frampton C, Espiner EA, Turner JG, Buttimore RC, Lainchbury JG, Elliott JM, Ikram H, Crozier IG, Smyth DW. Plasma N-terminal pro-brain natriuretic peptide and adrenomedullin: new neurohormonal predictors of left ventricular function and prognosis after myocardial infarction. Circulation. 1998. 97:1921–1929.
5. Omland T, Persson A, Ng L, O'Brien R, Karlsson T, Herlitz J, Hartford M, Caidahl K. N-terminal pro-B-type natriuretic peptide and long-term mortality in acute coronary syndromes. Circulation. 2002. 106:2913–2918.

6. Tateishi J, Masutani M, Ohyanagi M, Iwasaki T. Transient increase in plasma brain (B-type) natriuretic peptide after percutaneous transluminal coronary angioplasty. Clin Cardiol. 2000. 23:776–780.

7. Watanabe M, Egi K, Hasegawa S, Tanaka H, Ohshima H, Sakamoto T, Sunamori M. Significant of serum atrial and brain natriuretic peptide release after coronary artery bypass grafting. Surg Today. 2003. 33:671–673.
8. Palazzuoli A, Carrera A, Calabria P, Pastore M, Quatrini I, Vecchiato L, Campagna MS, Palazzuoli V, Nuti R. Brain natriuretic peptide levels during cardiac reperfusion: comparison between percutaneous coronary angioplasty and aorto-coronaric bypass. Clin Chim Acta. 2004. 342:87–92.

9. Mark DB, Felker GM. B-type natriuretic peptide: a biomarker for all seasons. N Engl J Med. 2004. 350:718–720.
10. Kikuta K, Yasue H, Yoshimura M, Morita E, Sumida H, Kato H, Kugiyama K, Ogawa H, Okumura K, Ogawa Y, Nakao K. Increased plasma levels of B-type natriuretic peptide in patients with unstable angina. Am Heart J. 1996. 132:101–107.

11. Marumoto K, Hamada M, Hiwada K. Increased secretion of atrial and brain natriuretic peptides during acute myocardial ischemia induced by dynamic exercise in patients with angina pectoris. Clin Sci. 1995. 88:551–556.
12. Bail DH, Kofler M, Ziemer G. Brain natriuretic peptide (BNP) in patients undergoing coronary artery bypass grafting. Thorac Cardiovasc Surg. 2004. 52:135–140.

13. Morimoto K, Mori T, Ishiguro S, Matsuda N, Hara Y, Kuroda H. Perioperative changes in plasma brain natriuretic peptide concentrations in patients undergoing cardiac surgery. Surg Today. 1998. 28:23–29.

14. Chello M, Mastroroberto P, Perticone F, Cirillo F, Bevacqua E, Olivito S, Covino E. Plasma levels of atrial and brain natriuretic peptides as indicators of recovery of left ventricular systolic function after coronary artery bypass. Eur J Cardiothorac Surg. 2001. 20:140–146.

15. Mair P, Mair J, Bleier J, Hormann C, Balogh D, Puschendorf B. Augmented release of brain natriuretic peptide during reperfusion of the human heart after cardioplegic cardiac arrest. Clin Chim Acta. 1997. 261:57–68.

16. Suttner SW, Boldt J. Natriuretic peptide system: physiology and clinical utility. Curr Opin Crit Care. 2004. 10:336–341.

17. Matsushita Y, Okamura Y, Iida H, Mochizuki Y, Mori H, Yamada Y, Shibasaki I, Shimada K. Usefulness of OPCAB from the viewpoint of fluctuation level of blood natriuretic peptides. Kyobu Geka. 2001. 54:321–325.
18. Kerbaul F, Giorgi R, Oddoze C, Collart F, Guidon C, Lejeune PJ, Villacorta J, Gouin F. High concentrations of N-BNP are related to non-infectious severe SIRS associated with cardiovascular dysfunction occurring after off-pump coronary artery surgery. Br J Anaesth. 2004. 93:639–644.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download