Abstract
Primary malignant melanoma of the esophagus (PMME) is an extremely rare tumor with only scattered cases reported. Although surgical resection has been considered as the best possible option, the prognosis has been nonetheless poor. We report a case of PMME which was treated by surgical resection and additionally followed by chemotherapy. A 60-yr-old man underwent an esophagoscopy due to a 3-month history of dysphagia and upper abdominal discomfort. A pigmented polypoid mass in the lower third of the esophagus was discovered, and a biopsy identified the mass as a malignant melanoma. Consequently, a subtotal esophagectomy and intrathoracic esophagogastrostomy was carried out. At follow-up four months after discharge, lymph node enlargements in the cervical area and celiac axis area were found. As a result, the patients was started on systemic chemotherapy treatment, which included Dacarbazine. The patient has been doing well and is now 35 months post-operative.
Primary malignant melanoma of the esophagus (PMME) is one of the extremely rare tumor and the prognosis is very poor. This tumor has usually been reported as a pedunculated, polypoid lesion in the middle and lower third of the esophagus. According to the reports, hematogenic and lymphogenic metastases are common for PMME cases. Surgical resection has been the preferred method of treatment, despite the poor prognosis. Adjuvant chemotherapy has been employed in some cases, but the effectiveness has not been proved. We report a case of PMME which was treated by surgical resection and post-operative chemotherapy.
A 60-yr-old male presented with a 3-month history of dysphagia and upper abdominal discomfort. He was treated at a private clinic under the impression of gastritis without symptomatic improvement. He had no smoking or drinking history. There were no abnormalities noted on physical examination or within the laboratory reports, and a pre-operative simple chest radiography and electrocardiography showed no abnormal findings. Barium-contrast esophagogram showed irregular luminal narrowing with a 4 cm sized filling defect at the distal esophagus. The proximal esophagus was dilated with markedly delayed dye passage (Fig. 1). Fiberoptic esophagoscopy showed a bell-shaped obstructing black mass with a 4 cm sized central ulcer located between 32 and 36 cm from the incisors. The pathology report of the biopsy specimen diagnosed the mass as malignant melanoma. Chest computerized tomogram showed the mass to be 5 cm in size at the posterior wall of the distal esophagus with evidence of lymph node enlargement in the lesser curvature of the stomach (Fig. 2, 3). Pulmonary function tests, whole body bone scan with TC-99m, and a computerized brain tomogram were all unremarkable, and therefore the pre-operative clinical stage was classified as IVA (cT3N0M1a).
The patient underwent a total esophagectomy and cervical esophagogastric anastomosis via a right thoracotomy, laparotomy and cervical incision. Reconstruction was performed by pulling the gastric tube up through a retro-sternal route. The cervical esophagogastric anastomosis was performed by a standard hand-sewn technique. There was no evidence of mediastinal lymph node enlargement and the post-operative course was uneventful but the patient suffered from post-operative pain. The patient was discharged 24th post-operative day.
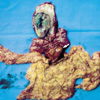
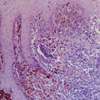
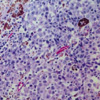
The resected mass was 5.5×4.2×1.3 cm in size, polypoid and pigmented from the distal esophagus with lymph node enlargement along the lesser curvature of the stomach (Fig. 4). Microscopic examination revealed junctional activities of atypical melanocytes around base of the tumor and a definitive diagnosis of PMME was made (Fig. 5, 6). The tumor cells invaded the muscular layer. No regional lymph node was positive for metastasis. Three lymph nodes at the lesser curvature of the stomach were infiltrated by tumor cells. This case was then classified as esophageal cancer, stage IVA:T2-N0M1a, according to the TMN classification of AJCC.
Four months after discharge, at a follow-up, lymph node enlargements in the cervical area and celiac axis area were found and systemic chemotherapy was started. The patient received Dacarbazine 800 mg/m2 intravenously (IV) on day 1, Cisplatin 30 mg/m2 IV on days 2-5, and Vinblastine 1.6 mg/m2 IV on days 1-5. The cycles were repeated every 4 weeks. After the fifth cycle of chemotherapy, the size of the lymph nodes decreased significantly and at 35 months post-operative, the patient is doing well without evidence of recurrence.
Since Baur made the first report of PMME in 1906, scattered cases have been reported in the literature and the incidence of PMME is reported to be less than 0.1% of all esophageal malignancies (1). Chalkiadakis and colleagues, in a review of 110 patients diagnosed with PMME found that men predominated the cases by 2:1, with an overall mean age of 60 yr (2). The tumors were usually located in the middle and lower third of the esophagus (86%). The common symptoms were dysphagia (73%), retrosternal pain (24%), weight loss (16%), and regurgitation (12%).
The diagnosis of PMME is difficult and best deduced by a combination of several examinations including upper gastrointestinal series, endoscopy, computed tomographic scan and biopsy with histopathologic assessment. Macroscopically, the tumor usually presents as a polypoid mass, that is focally ulcerated, but covered for the most part by intact squamous mucosa. According to the diagnostic criteria of primary melanoma proposed by Allen and Spitz, which seems to be widely accepted, the tumor is considered as primary when (a) the mass has a characteristic structure of melanoma containing melanin, (b) the adjacent epithelium contains melanocytes, (c) the tumor is polypoid, and (d) it arises from the area of junctional changes in the squamous epithelium (3). Thus, the proposed criteria for the origin of a tumor in the esophagus depends on the finding of junctional activity adjacent to the tumor mass. Recently, immunohistochemical staining utilizing antibodies specific to HMB-45 and/or S-100 cytoplasmic protein has been used to identify malignant melanoma of the esophagus (4, 5).
Hematogenic and lymphogenic metastasis are commonly associated with PMME and account for the poor prognosis. Widespread metastases with a rapid deterioration in health, followed by an early death is the usual clinical course. The most common site of metastases reported is the liver, followed by the mediastinum, mediastinal lymph nodes, lung and brain (2).
The choice of therapy primarily depends on the functional status and the presence and extent of the metastatic disease at the time of diagnosis. Surgical resection with re-establishment of gastrointestinal continuity is the proposed methods of treatment, and looks like to provide the best result. The median survival rate after surgical resection was 13.4 months and longest reported survival was 12 yr (2, 6). Chemotherapy, radiation therapy, and immunotherapy have been reported, but with limited success (7, 8). Recently, several authors have reported a therapeutic effect of combination chemotherapy including Dacarbazine (9, 10). In this patient, post-operative chemotherapy has thus far been effective in controlling recurrence. This case supports the combination of surgical resection and post-operative adjuvant chemotherapy, with Dacarbazine, and therefore should be considered as another treatment modality.
Figures and Tables
Fig. 1
Pre-operative esophagogram demonstrating a 4 cm sized mass with an irregular surface protruding into the lower esophagus.

Fig. 2
Contrast-enhanced chest CT scan showing a mass lesion from posterior wall of the lower esophagus (arrow).

Fig. 4
Gross appearance of the resected specimen showing the ulcerated, black, sessile polypoid tumor in the lower esophagus with lymph node enlargement along the lesser curvature of the stomach (arrow).
References
1. Turnbull AD, Rosen P, Goodner JT, Beattie EJ. Primary malignant tumors of the esophagus other than typical epidermoid carcinoma. Ann Thorac Surg. 1973. 15:463–473.

2. Chalkiadakis G, Wihlm JM, Morand G, Weill-Bousson M, Witz JP. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1985. 39:472–475.

3. Allen AC, Spitz S. Malignant melanoma: A clinico-pathological analysis of criteria for diagnosis and prognosis. Cancer. 1953. 6:1–45.
4. Stranks GJ, Mathai JT, Rowe-Jones DC. Primary malignant melanoma of the esophagus: case report and review of surgical pathology. Gut. 1991. 32:828–830.
5. DiCostanzo DP, Urmacher C. Primary malignant melanoma of the esophagus. Am J Surg Pathol. 1987. 11:46–52.

6. Hamdy FC, Smith JH, Kennedy A, Thorpe JA. Long survival after excision of a primary malignant melanoma of the oesophagus. Thorax. 1991. 46:397–398.

7. Caldwell CB, Bains MS, Burt M. Unusual malignant neoplasms of the esophagus. Oat cell carcinoma, melanoma, and sarcoma. J Thorac Cardiovasc Surg. 1991. 101:100–107.
8. Joob AW, Haines GK III, Kies MS, Shields TW. Primary nalignant melanoma of the esophagus. Ann Thorac Surg. 1995. 60:217–222.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download