1. Moos RH, Brennan PL, Mertens JR. Diagnostic subgroups and predictors of one-year readmission among late middle aged and older substance abuse patients. J Stud Alcohol. 1994. 55:173–183.
2. Thomas MA, Alterman AI, Metzger DS, Grissom GR, Woody GE, Luborsky L, O'Brien CP. Similarity of outcome predictors across opiates, cocaine and alcohol treatments: Role of treatment services. J Consulting Clin Psychol. 1994. 62:1141–1158.
3. Kim JS, Park BK, Cho YC, Oh MK, Kim GJ, Oh JK. Influence of alcoholic's insight on their abstinent outcomes for one year after discharge. J Korean Acad Fam Med. 2001. 22:1052–1066.
4. Finney JW, Moos RH. The long-term course of treated alcoholism: I. mortality, relapse and remission rates and comparisons with community controls. J Stud Alcohol. 1991. 52:44–54.

5. Kim JS, Han SI, Kim KS. Clinical variables affecting relapse of alcoholism. J Korean Neuropsychiatr Assoc. 1994. 33:817–824.
6. Irwin M, Schuckit MA, Smith TL. Clinical importance of age at onset in type 1 and type 2 primary alcoholics. Arch Gen Psychiat. 1990. 47:320–324.

7. Project MATCH research group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997. 58:7–29.
8. Kim JS, Park BK, Yu IS, Oh MK. Improvement of insight in patients with alcohol dependence by treatment programs. J Korean Acad Fam Med. 2000. 21:1180–1187.
9. Kim KC, Lee KS, Jung G, Shin SE. The relationship between insight level and defense mechanisms in alcoholic patients. J Korean Acad Addict Psychiat. 2004. 8:115–123.
10. Sung SK, Lee JJ, Kim HO, Lee KH. Effectiveness of inpatient treatment program on the insight and satisfaction of alcoholics. J Korean Acad Addict Psychiat. 2002. 6:20–29.
11. Kim JH, Kim SG, Sung SK, Min YK, Kim JY, Kim SY, Kim MJ. Association of insight level with false-negative alcoholism screening tests in alcohol-dependent patients. J Korean Acad Addict Psychiat. 2004. 8:124–128.
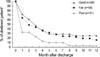
12. Sung SK, Moon WS, Kim HO, Lee KH. A short-term follow-up study of participants in an inpatient alcoholism treatment program. J Korean Acad Addict Psychiat. 2003. 7:123–133.
13. Jeong JI, Han WS, Jun MK, Lee GW, Kim TW, Kim JY, Shin KC. The characteristics of the dropout patients from an alcoholism treatment program. J Korean Acad Addict Psychiat. 2004. 8:99–114.
14. Sadock BJ. Sadock BJ, Sadock VA, editors. Signs and symptoms in psychiatry. Kaplan and Sadock's Comprehensive Textbook of Psychiatry. 2005. 8th Edition. Philadelphia: Lippincott Williams & Wilkins;847–859.
15. Kim JS. Patient education for moderate drinking. J Korean Med Assoc. 2004. 47:556–567.

16. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 2000. 4th Edition, Text Revision. Washington, DC: American Psychiatric Association.
17. Smilkstein G. The Family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract. 1978. 6:1231–1239.
18. Smilkstein G, Ashworth C, Montano D. Validity and reliability of the Family APGAR as a test of family function. J Fam Pract. 1982. 15:303–311.
19. Olson DH. Circumplex Model VII: validation studies and FACES III. Fam Process. 1986. 25:337–351.

20. Selzer ML. The Michigan Alcoholism Screening Test: The quest for a new diagnostic instrument. Am J Psychiat. 1971. 127:1653–1658.

21. Kim JS, Kim GJ, Lee JM, Lee CS, Oh JK. HAIS (Hanil Alcohol Insight Scale): Validation of an insight-evaluation instrument for practical use in alcoholism. J Stud Alcohol. 1998. 59:52–55.

22. Sung SK, Bang YW, Haham U. A follow-up study of alcoholic inpatients by the telephone interview. J Korean Neuropsychiat Assoc. 1993. 32:698–706.
23. Moon YH, Kim GS, Oh DY. A follow-up study of alcoholics inpatients in an alcoholism treatment program. J Korean Acad Addict Psychiat. 1998. 2:227–235.
24. Kim SS, Shin JJ, Whang IB, Chai SH. Relationship between insight level and psychological characteristics in alcoholic patients. J Korean Acad Addict Psychiat. 2002. 6:49–57.
25. Markova IS, Berrios GE. The assessment of insight in clinical psychiatry: a new scale. Acta Psychiatr Scand. 1992. 86:159–164.







 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download