Abstract
Hypothyroidism has various cardiovascular manifestation and exhibits electrocardiographic change. The QT dispersion on surface ECG reflects regional variations in myocardial repolarization. The effect of L-thyroxine treatment on ECG parameters, such as QT dispersion, in patients with primary hypothyroidism were investigated. This study involved 18 patients (3 men, 15 women, ages: 48±18 yr) with primary hypothyroidism. All patients were checked with a standard 12-lead ECG before and after L-thyroxine treatment. Various ECG parameters were then measured twice. The mean L-thyroxine treatment duration was 22±2.7 months. The mean thyroid-stimulating hormone levels of patients before and after therapy were 40.2±29.8 µU/mL, 3.6±4.6 µU/mL (p<0.001) and free-T4 levels were 0.44±0.38 ng/dL, 1.51±0.39 ng/dL (p<0.001). After L-thyroxine treatment, QT interval (395±42 vs. 380±24 msec, p<0.05), QTc interval (434±32 vs. 417±23 msec, p<0.05), QT dispersion (45±23 vs. 30±13 msec, p=0.008), QTc dispersion (49±23 vs. 32±14 msec, p=0.005) significantly decreased. There were no significant changes in the PR and RR intervals, as well as the QRS duration. Our findings suggest that the thyroid hormone affects ventricular inhomogenicity, and that L-thyroxine replacement therapy may reduce malignant ventricular arrhythmia and sudden cardiac death in primary hypothyroidism.
Hypothyroidism has various cardiovascular manifestations including impaired diastolic function, reduced contractility and infrequently pericardial effusion and heart failure (1-3). Electrocardiographic (ECG) changes in hypothyroidism were bradycardia, RBBB, flat or inverted T wave, QRS prolongation, QT prolongation and infrequently ventricular arrhythmia, torsades de pointes (1-3). The QT interval reflects traditional electrocardiographic parameter of the duration of ventricular repolarization. The QT dispersion is the interlead variability of QT interval on surface ECG that reflects regional variations in myocardial repolarization. Increased the QT dispersion has been linked to the occurrence of malignant ventricular arrhythmias and sudden cardiac death (4-6). However, it was reported that the deficiency of thyroid hormone did not affect ECG findings of congenitally hypothyroid neonates (7). Therefore, the effects of L-thyroxine treatment on ECG parameters, such as QT dispersion, in patients with primary hypothyroidism were examined.
This retrospective study involved 18 patients (3 men, 15 women, age: 48±18 yr) with primary hypothyroidism. The patient taking the QT-prolonging drugs or who had histories of cardiac disease were excluded. All patient were checked with serum free T4, thyroid-stimulating hormone (TSH) and standard 12-lead ECGs before and after L-thyroxine treatment.
After a rest period, the electrocardiogram had been checked with 12-lead by electrocardiography recorder (25 mm/sec, Marquette, Fairfield, Connecticut, U.S.A.). All measurements were obtained manually by 1 observer unaware of patient identity, diagnosis, and therapy. The QT interval was measured as the distance between onset of the QRS complex and the end of the T wave in all 12-lead. When the U wave interrupted, the end of the T wave was estimated by extrapolation of the descending T-wave lined down to the baseline. Leads without visible T waves were excluded from the analysis. The QTc was calculated from Bazzett's formula (QTc=QT/√RR). The QTd was defined as the difference between the maximum QT and the minimum QT across all 12 leads.
The data were analyzed using a statistical package (SPSS Window 10.0 ver). Whenever the data could be paired, these were analyzed using paired t-tests. The correlation was examined by the calculation of Pearson's coefficient. A p value <0.05 was considered statistically significant.
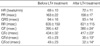
Of the 18 patients, 3 were men and 15 were women. The mean age was 48±18 yr at the study baseline. The mean follow-up duration was 22 months. The thyroid function test, before and after L-thyroixine treatment, is shown in Table 1.
The QT prolongation was detected in 6 patients (33%) at the study baseline. After the L-thyroxine treatment, 5 patients were normalized. The T-inversion appeared in 3 patients, and after the L-thyroxine treatment, all patients were normalized (Fig. 1). The QTc prolongation correlated positively with the baseline TSH level (r=0.484, p=0.042).
It was found that after the L-thyroxine treatment, the QT interval (p<0.05), QTc interval (p<0.05), QT dispersion (p=0.008), and the QTc dispersion (p=0.005) significantly decreased. There were no significant changes in the PR interval, RR interval, nor the QRS duration (Table 2).
The thyroid hormone affects the function of several human organs even the heart. It is well documented that hypothyroidism affects cardiac functions and have various cardiovascular manifestations including impaired diastolic functions, reduced contractility and infrequently pericardial effusion and heart failure. Hypothyroidism classically has been associated with bradycardia, but the degree of slowing heart rate is often modest. Other electrocardiographic changes in hypothyroidism were RBBB, flat or inverted T waves, QRS prolongation, QT prolongation and infrequently ventricular arrhythmia, torsades de pointes (1-3). The function of the atrial pacemaker is normal and atrial ectopy is rare, but premature ventricular beats and occasionally ventricular tachycardia can occur (8). This is in contrasts to thyrotoxicosis, in which atrial tachyarrhythmias are common and ventricular arrhythmias are rare. The syndrome of torsade de pointes with a long QT interval and ventricular tachycardia can occur with hypothyroidism and be resolved with T4 treatment alone (3, 9).
The duration of the action potential may be prolonged, perhaps reflecting a decrease in voltage-gated potassium channels. Nathaniel et al. reported that significant prolongation of the QTc interval occurred in inadequately treated hypothyroidism and the degree of the QTc prolongation was directly related to the severity of hypothyroidism (2). Altun et al. showed that QT prologation and increased QTd were directly related to the TSH levels in hypothyroidism (10). The QTd reflects regional variations in myocardial repolarization. Increased QTd has been found to be associated with an increased incidence of malignant ventricular arrhythmias and sudden death (4-6). The QTd provides a potentially simple, inexpensive, noninvasive method of measuring underlying dispersion recovery of ventricular excitability, and should be defined in a way that most accurately reflects this state (11). Clinical observations showed that ventricular arrhythmias and sudden death are uncommon in hypothyroidism, despite the marked lengthening of the QT interval (3, 12, 13). However, increased QTd in hypothyroidism may facilitate ventricular arrhythmias with hypokalemia, hypomagnesemia, long QT syndrome or drugs.
Abnormal changes of heart rate variability measurements and its improvement after treatment in hypothyroidism were reported (14). However, the deficiency of the thyroid hormone did not affect ECG findings of congenitally hypothyroid neonate (7). It was necessary to clarify the effects of L-thyroxine treatment on ECG parameters in primary hypothyroidism. In this study, our results showed that the QTc and QT dispersions improved after the L-thyroxine treatment in patients with primary hypothyroidism. This suggests that the thyroid hormone affects ventricular inhomogenicity, and subsequent L-thyroxine replacement therapy may reduce malignant ventricular arrhythmia and sudden cardiac death in primary hypothyroidism.
Figures and Tables
References
1. Serma JS, Venkataraman K, Nicod P, Polikar R, Smith J, Schoenbaum MP, Singh BN. Circadian rhythmicity of rate-normalized QT interval in hypothyroidism and its significance for development of class III antiarrhythmic agents. Am J Cardiol. 1990. 66:959–963.
2. Nathaniel C, Caleb L, Azrin MA. QTc prolongation in hypothyroidism. J Am Coll Cardiol. 1994. 23:36A.
3. Schenck JB, Rizvi AA, Lin T. Severe primary hypothyroidism manifesting with torsades de pointes. Am J Med Sci. 2006. 331:154–156.

4. Hii JT, Wyse DG, Gillis AM, Duff HJ, Solylo MA, Mitchell LB. Precordial QT interval dispersion as a marker of torsade de pointes. Circulation. 1992. 86:1376–1382.
5. Yunus A, Gillis AM, Duff HJ, Wyse DG, Mitchell LB. Increased precordial QTc dispersion predicts ventricular fibrillation during acute myocardial infarction. Am J Cardiol. 1996. 78:706–708.
6. Zareba W, Moss AJ, Le Cessie S. Dispersion of ventricular repolarization and arrhythmic cardiac death in coronary artery disease. Am J Cardiol. 1994. 74:550–553.

7. Asami T, Suzuki H, Yazaki S, Sato S, Uchiyama M. Effects of thyroid hormone deficiency on electrocardiogram findings of congenitally hypothyroid neonates. Thyroid. 2001. 11:765–768.

8. Burack R, Edwards RH, Green M, Jones NL. The response to exercise before and after treatment of myxedema with thyroxine. J Pharmacol Exp Ther. 1971. 176:212–219.
9. Fredlund B, Olsson SB. Long QT interval and ventricular tachycardia of "torsade de pointe" type in hypothyroidism. Acta Med Scand. 1983. 213:231–235.

10. Altun A, Altun G, Ozkan B, Kaya M, Ozbay G. The relationship between ventricular repolarization and thyroid stimulating hormone. Ann Noninvasive Electrocardiogr. 1998. 3:19.
11. Inukai T, Takanashi K, Kobayashi H, Fujiwara Y, Tayama K, Aso Y, Takemura Y. Power spectral analysis of variations in heart rate in patients with hyperthyroidism on hypothyroidism. Horm Metab Res. 1998. 30:531–535.
12. Singh BN. When is QT prolongation antiarrhythmic and when is it proarrhythmic? Am J Cardiol. 1989. 63:867–869.

13. Venkatesh N, Lynch JJ, Uprishard AC, Kitzen JM, Lucchesi DR. Hypothyroidism renders protection against lethal ventricular arrhythmias in a conscious canine model of sudden death. J Cardiovasc Pharmacol. 1991. 18:703–710.

14. Xing H, Shen Y, Chen H, Wang Y, Shen W. Heart rate variability and its response to thyroxine replacement therapy in patients with hypothyroidism. Chin Med J (Engl). 2001. 114:906–908.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download