Abstract
Ceramides are the main lipids in the stratum corneum and are generated during cellular stress and apoptosis by de novo synthesis or by the action of sphingomyelinase. In addition, they are lipid second messengers produced by sphingolipid metabolism and trigger important cell responses, including protein kinase C-alpha (PKC-α) activation and the stimulation of signal transduction pathways with apoptosis and stress-activated protein kinases (SAPK), such as c-jun N-terminal kinase (JNK). Thus, ceramides have anti-proliferative and apoptotic effects. This study measured the changes in the levels of epidermal ceramides and ceramide-related apoptotic signaling molecules in psoriasis patients. Samples from lesional and non-lesional epidermis were obtained from psoriasis patients. Total ceramides were fractionated using thin-layer chromatography, and the levels of PKC-α and JNK expression were measured using Western blot analysis with specific antibodies. The ceramide level was reduced significantly, and this was associated with the downregulation of apoptotic signaling molecules, such as PKC-α and JNK, in the lesional epidermis of psoriasis patients. These results suggest that the decreased level of ceramides downregulates the apoptotic pathway, leading to epidermal proliferation in psoriasis.
Ceramides are the main lipids in the stratum corneum (1). The depletion of ceramides in the stratum corneum is thought to be one of the etiological factors producing dryness and barrier disruption in skin conditions (2-4). Marked depletion of ceramides in the stratum corneum has been reported in patients with psoriasis.
Ceramides are generated during cellular stress and apoptosis by de novo synthesis or by the action of sphingomyelinase. Ceramides have antiproliferative and apoptotic effects (5). These are lipid second messengers produced by sphingolipid metabolism, and they trigger important cell responses, including protein kinase C-alpha (PKC-α) activation (6). Ceramides stimulate the signal transduction pathway with apoptosis and activate stress-activated protein kinases (SAPK), such as c-jun N-terminal kinase (JNK) (7).
Several investigators have already reported decreased levels of epidermal ceramides in psoriasis. However, only limited information is available on the alterations in the apoptotic pathway related to ceramides in skin diseases with epidermal proliferation, including psoriasis. Therefore, this study examined the alterations in the levels of epidermal ceramides and ceramide-related apoptotic signaling molecules in patients with psoriasis.
Five Korean patients with psoriasis (2 women, 3 men) ranging in age from 19 to 33 yr gave informed consent and took part in this study. All the subjects had psoriasis vulgaris as identified through clinical and histological assessment and had not been treated either systemically or topically for at least 1 month before punch biopsies were obtained.
Using a 4-mm punch, biopsies were taken from lesional and non-lesional skin on the lower extremities, back, or arms. The epidermis was separated as described previously (8). Specifically, the epidermis was separated from whole-skin biopsies by overnight incubation at 4℃ in a 1:1 (v/v) mixture of Dispase solution (Roche Molecular Biochemicals, Manheim, Germany) and Hank's balanced salt solution (HBSS; Gibco BRL, Life Technologies, Rockville, MD, U.S.A.).
The clinical severity was assessed using the PASI score, which is calculated as follows:
PASI=0.1 (Eh+Ih+Dh)Ah+0.2 (Eu+Iu+Du)Au+0.3 (Et+It+Dt)At+0.4 (El+Il+Dl)Al, where E=erythema, I=infiltration, D=desquamation, A=area, h=head, u=upper extremities, t=trunk, and l=lower extremities. A numerical value is given to the extent of the lesions in each area: 1=<10%, 2=10-30%, 3=30-50%, 4=50-70%, 5=70-90%, and 6=90-100%. E, I, and D are scored on a five-point scale (0=no symptoms, 1=slight, 2=moderate, 3=marked, and 4=very marked) to obtain a final PASI score between 0 and 72. The PASI scores of the patients who took part in this study ranged between 4.9 and 20.7; this range corresponds to mild and moderate psoriasis. Only patients with PASI scores <25 were enrolled in this study in order to determine whether alterations in the levels of ceramides and ceramide-related apoptotic signaling molecules are closely correlated to the clinical severity in mild to moderate psoriasis.
The frozen skin samples were added to 600 µL of Folch solution (CHCl3: MeOH [2:1, v/v] mixture) and were homogenized using a polytron homogenizer, and 200 µL of 0.1 M KCl were added. The mixture was centrifuged at 12,000 rpm twice for 5 min each. The lower phase containing the extracted lipids was fractionated by thin-layer chromatography (TLC) on 0.20 mm silica gel 60-coated plates (10×10 cm plate, Whatman Inc., Clifton, NJ, U.S.A.) using a modification of the method reported by Uchida et al. (8-10). Specifically, after depositing each sample on the plate, it was developed first up to 5.0 cm using a mobile phase consisting of CHCl3:MeOH:H2O (57:12:0.6, v/v/v) and then up to 14.0 cm using 1,2-dichloroethane:CHCl3:acetic acid (46:6:0.05, v/v/v). The latter step was repeated using the same mobile phase. Finally, the chromatogram was developed to the top using a mobile phase consisting of n-hexane:diethylether:acetic acid (98:1:1, v/v/v). All these solvents were obtained from Sigma-Aldrich. Each stage of development was carried out after the plate was air-dried completely. The UV absorbance of the fractions containing total ceramides was measured at 254 nm using a TLC scanner. The data were analyzed using the program winCAT (TLC scanner; CAMAG winCATS TLC scanner 3, 254 nm).
To allow for variation in the absolute value among subjects, the ceramide content was normalized according to the protein content. The upper phase of the lipid extraction stage was centrifuged at 800×g for 5 min to remove tissue debris, and the protein concentration was determined according to the modified Lowry method using bovine serum albumin as a standard (11). The levels of ceramides were assessed as cpm/µg protein.
The primary antibodies against PKC-α, ceramidase, and JNK were isotype mouse IgG2b, IgG1, and isotype rabbit IgG, respectively. Anti-PKC-α and anti-ceramidase were obtained from BD Bioscience, and anti-JNK was from Santa Cruz Biotechnology. All secondary antibodies were obtained from Amersham Biosciences.
Soluble fractions were prepared from psoriatic epidermis, and equal amounts of protein (50 µg) were resolved on 8% gels by using sodium dodecylsulfate-polyacrylamide gel electrophoresis (SDS-PAGE). The proteins were transferred to nitrocellulose membranes and blotted with specific antibodies to PKC-α, JNK, and ceramidase, using standard procedures. PKC, JNK, and ceramidase/antibody complexes were visualized by autoradiography using a chemiluminescent substrate. The optical densities were measured using a densitometer and were normalized using a control. All procedures were performed in triplicate.
The statistical significance of the differences in the levels of ceramides, PKC-α, JNK, and ceramidase between lesional and non-lesional samples of psoriasis patients was assessed using a paired t-test. The correlations between the levels of ceramides, PKC-α, JNK, and ceramidase and the PASI scores were determined using the Pearson correlation test. p-values <0.05 were considered statistically significant.
The levels of ceramides in lesional and non-lesional epidermis and the PASI scores of the psoriasis patients are shown in Table 1. Although the absolute level of ceramides differed among the patients, the level of ceramides in the lesional epidermis was always significantly lower (n=5, p<0.05) than that in the non-lesional epidermis, with the percentage reduction ranging from 21.7 to 75.8. A highly significant positive correlation was observed between the percentage reduction of the ceramide level and the PASI score (r=0.944, p=0.016), as shown in Fig. 1, indicating that the ceramide level is inversely correlated with the PASI score in mild to moderate psoriasis.
The expression levels of PKC-α, JNK, and ceramidase were measured in both lesional and non-lesional epidermis. The expression of PKC-α was not detected in lesional epidermis, in contrast to the expression in non-lesional epidermis (Fig. 2). The expression level of JNK was lower in lesional epidermis than in non-lesional epidermis. Although the absolute level of JNK expression differed among the subjects, the expression levels in lesional epidermis were always significantly lower than those in non-lesional epidermis (p<0.05) (Fig. 3). However, no correlation was observed between the reductions in the PKC-α and JNK levels and the PASI score (data not shown). The expression of ceramidase was much lower in both lesional and non-lesional epidermis, and the differences between the two were insignificant (data not shown).
Decreased levels of ceramides have been reported in skin conditions involving dryness and barrier disruption, such as psoriasis. Moreover, the importance of ceramides in the epidermal lipid barrier has been documented repeatedly (1, 3-5). In terms of the apoptotic pathway, however, there are few investigations of ceramides and related apoptotic signals in psoriatic epidermis. This study showed that the level of ceramides was significantly reduced with concomitant decreases in PKC-α and JNK in lesional epidermis of patients with psoriasis.
Decreased levels of ceramides have been associated with skin conditions involving dryness and barrier disruption, such as psoriasis, atopic dermatitis, and xerosis (12, 13). In this study, the levels of ceramides were decreased significantly in psoriatic epidermis. The level of ceramides in the epidermis results from the balance between the activities of ceramide-generating enzymes, such as serine palmitoyl transferase in the de novo synthesis pathway and sphingomyelinase, and the activities of degradative enzymes, such as ceramidase (14-17). Previously, we observed that the levels of ceramides were decreased, while those of diacylglycerol were increased (13). In addition, no alteration in the ceramidase level was detected. It is understood that the sphingomyelin pathway is initiated by the hydrolysis of sphingomyelin by sphingomyelinase (18). Together with these findings, the present data suggest that the dramatic reduction in the ceramide level, which is significantly correlated with the clinical severity, is caused by a decrease in the activity of sphingomyelinase. However, the complete relationship between the ceramide content and the activity of ceramide-metabolizing enzymes in the psoriatic skin remains to be clarified.
We observed decreased levels of PKC-α and JNK expression in lesional epidermis with psoriasis, together with decreased levels of ceramides. This suggests that the decreased level of ceramides induced downregulation of the apoptotic signaling pathway in the psoriatic epidermis. These results are in concordance with the findings of earlier studies, in which the level of PKC-α expression was decreased in psoriatic epidermis (19, 20). However, no correlation was observed between the expression levels of PKC-α and JNK and the PASI score in mild to moderate psoriasis.
Ceramides induce the activation of apoptotic cell-signaling molecules, such as PKC-α and JNK. In addition, sphingomyelinase-induced ceramide generation is stimulated by PKC-α and JNK activation (20, 21). Hence, this suggests that decreased ceramide levels lead to the downregulation of PKC-α and JNK, which in turn downregulates sphingomyelinase-induced ceramide generation and ultimately induces the anti-apoptotic and proliferative characteristics of psoriatic epidermis.
In conclusion, we demonstrated that 1) the level of ceramides was reduced significantly in lesional epidermis with psoriasis, 2) this decrease was associated with the downregulation of apoptotic signaling molecules, such as PKC-α and JNK, and 3) there was a significant correlation between the ceramide level and the clinical severity in mild to moderate psoriasis. We are not certain whether this finding is a primary or secondary event in psoriasis. However, we suggest that the reduction in the ceramide level not only induces a defect in water retention and barrier function but also associates with downregulation of the apoptotic pathway resulting in epidermal proliferation in psoriasis.
Figures and Tables
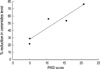 | Fig. 1Correlation between the percentage reduction in the ceramide level in lesional epidermis and the PASI scores of psoriasis patients. A highly significant positive correlation was observed between the percentage reduction of the ceramide level and the PASI score (r=0.944, p=0.016). |
 | Fig. 2Western blot analysis of PKC-α in lesional and non-lesional epidermis of psoriasis patients. Western blotting was performed using mouse anti-PKC-α antibodies, as described in the Materials and Methods. The level of PKC-α expression was quantified by densitometry (optical density, OD) and is expressed as the percentage of the expression of the control β-actin (normalized OD). |
 | Fig. 3Western blot analysis of JNK in lesional and non-lesional epidermis of psoriasis patients. Western blotting was performed using rabbit anti-JNK antibodies, as described in the Materials and Methods. The level of the JNK expression was quantified by densitometry (optical density, OD) and is expressed as the percentage of the expression of the control β-actin (normalized OD).
*Significant differences between lesional epidermis and non-lesional epidermis (p<0.05).
|
References
1. Elias PM, Menon G. Elias PM, editor. Structural and lipid biochemical correlates of the epidermal permeability barrier. Adv Lipid Research. 1991. 24:1–26.

2. Imokawa G, Abe A, Jin K, Higaki Y, Kawashima M, Hidano A. Decreased level of ceramides in stratum corneum of atopic dermatitis: an etiologic factor in atopic dry skin. J Invest Dermatol. 1991. 96:523–526.

3. Matsumoto M, Umemoto N, Sugiura H, Uehara M. Difference in ceramide composition between "dry" and normal skin in patients with atopic dermatitis. Acta Derm Venereol (Stockh). 1999. 79:246–247.
4. Chung S, Kong S, Seong K, Cho Y. γ-Linolenic acid in borage oil reverses epidermal hyperproliferation in guinea pigs. J Nutr. 2002. 132:3090–3097.

5. Aschrafi A, Franzen R, Shabahang S, Fabbro D, Pfeilschifter J, Huwiler A. Ceramide induces translocation of protein kinase C-alpha to the Golgi compartment of human embryonic kidney cells by interacting with the C2 domain. Biochim Biophys Acta. 2003. 1634:30–39.
6. Huwiler A, Fabbro D, Pfeilschifter J. Selective ceramide binding to protein kinase C-alpha and -delta isoenzymes in renal mesangial cells. Biochemistry. 1998. 37:14556–14562.
7. Ruvolo PP. Ceramide regulates cellular homeostasis via diverse stress signaling pathways. Leukemia. 2001. 15:1153–1160.

8. Macheleidt O, Kaiser HW, Sandhoff K. Deficiency of epidermal protein-bound ω-hydroxyceramides in atopic dermatitis. J Invest Dermatol. 2002. 119:166–173.

9. Tohyama J, Oya Y, Ezoe T, Vanier MT, Nakayasu H, Fujita N, Suzuki K. Ceramide accumulation is associated with increased apoptotic cell death in cultured fibroblasts of sphingolipid activator protein-deficient mouse but not in fibroblasts of patients with Farber disease. J Inherit Metab Dis. 1999. 22:649–662.

10. Uchida Y, Hara M, Nishio H, Sidransky E, Inoue S, Otsuka F, Suzuki A, Elias PM, Holleran WM, Hamanaka S. Epidermal sphingomyelins are precursors for selected stratum corneum ceramides. J Lipid Res. 2000. 41:2071–2082.

11. Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the folin phenol reagent. J Biol Chem. 1951. 193:265–275.

12. Motta S, Monti M, Sesana S, Mellesi L, Ghidoni R, Caputo R. Abnormality of water barrier function in psoriasis. Role of ceramide functions. Arch Dermatol. 1994. 130:452–456.
13. Cho Y, Lew BL, Seong K, Kim NI. An inverse relationship between ceramide synthesis and clinical severity in patients with psoriasis. J Korean Med Sci. 2004. 19:859–863.

15. Jin K, Higaki Y, Takagi Y, Higuchi k, Yada Y, Kawashima M, Imokawa G. Analysis of beta-glucocerebrosidase and ceramidase activity in atopic and aged dry skin. Acta Derm Venereol. 1994. 74:337–340.
16. Aioi A, Tonogaito H, Suto H, Hamada K, Ra CR, Ogawa H, Maibach H, Matsuda H. Impairment of skin barrier function in NC/Nga Tnd mice as a possible model for atopic dermatitis. Br J Dermatol. 2001. 144:12–18.

17. Hara J, Hoguchi K, Okamoto R, Kawashima M, Imokawa G. High expression of sphingomyelin deacylase is an important determinant of ceramide deficiency leading to barrier disruption in atopic dermatitis. J Invest Dermatol. 2000. 115:406–413.
18. Spiegel S, Foster D, Kolesnick R. Signal transduction through lipid second messengers. Curr Opin Cell Biol. 1996. 8:159–167.

19. Fisher GJ, Tavakkol A, Leach K, Burns D, Basta P, Loomis C, Griffiths CE, Cooper KD, Reynolds NJ, Elder JT. Differential expression of protein kinase C isoenzymes in normal and psoriatic adult human skin: reduced expression of protein kinase C-beta II in psoriasis. J Invest Dermatol. 1993. 101:553–559.
20. Visnjic D, Batinic D, Banfic H. Different roles of protein kinase C alpha and delta isoforms in the regulation of neutral sphingomyelinase activity in HL-60 cells. Biochem J. 1999. 344:921–928.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download