Abstract
Studies investigating the effect of prophylactic drugs on hepatic veno-occlusive disease (VOD) development are rare in children that have undergone allogeneic hematopoietic stem cell transplantation (HSCT). This study examined risk factors for VOD, the effect of prophylactic low-dose heparin or lipo-prostaglandin E1 (lipo-PGE1) and the survival rate at day +100 in children undergoing allogeneic HSCT. Eighty five children underwent HSCT between June 1997 and September 2004. Patients were diagnosed and classified as having mild, moderate or severe VOD according to Seattle clinical criteria. Among 85 patients, 25 (29%) developed VOD. VOD occurred more frequently in patients receiving busulfan-based conditioning (24/65, 37%) than in those receiving TBI-based (1/10, 10%) or other (0/10, 0%) regimens (p<0.05). The incidence of VOD was lower in patients with non-malignant disease compared to those with malignant disease (p<0.05). Survival at day +100 for non-VOD patients was better than that for VOD patients (92% vs. 76%, p<0.05). No patients receiving prophylactic heparin or lipo-PGE1 were found to develop severe VOD, whereas 5 of 35 patients not receiving such prophylaxis developed severe VOD. Given severe VOD is associated with a high mortality rate, this study indicates that prophylactic heparin or lipo-PGE1 may decrease mortality in children undergoing HSCT.
Veno-occlusive disease (VOD) of the liver is a severe complication of intensive chemotherapy and hematopoietic stem cell transplantation (HSCT). The incidence rate of VOD ranges from 5% to 60%, and the mortality rate is as high as 50% in some studies (1-4). In children who have undergone HSCT, the incidence of VOD ranges from 22% to 28%, and the mortality rate is reported to be up to 47% (5-8). VOD is characterized by right upper quadrant pain, hepatomegaly, fluid retention, ascites, weight gain and hyperbilirubinemia occurring by day 20 after HSCT (1).
Reported risk factors for developing VOD include pre-HSCT liver dysfunction, poor performance status, female gender, advanced disease status at the time of transplantation, prior hepatic irradiation, vancomycin or amphotericin B use in the early post transplantation period, HLA mismatch-related or -unrelated donor transplantation, and use of busulfan (Bu) or total body irradiation (TBI) as a conditioning regimen (2, 5-11). An important new risk factor for VOD is administration of gemtuzumab ozogamicin (Mylotarg), an anti-CD33 monoclonal antibody (12-17).
The prevention of fatal VOD is an obvious priority. The prophylactic use of drugs such as heparin or prostaglandin E1 (PGE1) has a beneficial effect in preventing VOD development. Some reports show that continuous infusion of low dose heparin is highly effective in preventing VOD after HSCT without an added risk of bleeding (18, 19). PGE1 is a vasodilator with inhibitory effects on platelet aggregation and prothrombolytic activity (20). Gluckman et al. reported that the use of prophylactic PGE1 via continuous intravenous infusion decreased the overall incidence of VOD, although they did not use lipo-PGE1 (21). Cho et al. reported the possible beneficial effect of lipo-PGE1 to prevent development of VOD, whereas they did not compare the efficacy with control group (22).
The purpose of the present single center study was to identify VOD risk factors and the effect of prophylactic low-dose heparin or PGE1 on pediatric patients undergoing allogeneic HSCT.
Eighty-nine pediatric patients undergoing allogeneic HSCT at the Asan Medical Center between June 1997 and September 2004 were enrolled. Four patients who died of causes other than VOD before day +21 were subsequently excluded. The medical records of the remaining 85 patients were retrospectively reviewed.
The following parameters were evaluated to determine their status as risk factors for the development of VOD: 1) patient-related factors: age at time of HSCT, disease status at the time of transplantation, viral serology results in both donor and recipient, and liver function before HSCT; 2) transplantation-related factors: stem cell source, HLA matching, conditioning regimen and prophylactic treatment for VOD.
The following factors were evaluated to determine their effect on the severity of VOD: maximum level of total serum bilirubin, maximum level of serum aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase (ALP), maximum level of serum blood urea nitrogen (BUN), serum creatinine (Cr) and post-transplantation weight gain.
Diseases were divided into three groups according to type and status at the time of transplantation: 1) non-malignant diseases, including severe aplastic anemia (SAA), pure red cell anemia (PRCA), chronic granulomatous disease (CGD) and hemophagocytic lymphoproliferate histiocytosis (HLH) in second remission, 2) early stage hematologic malignancies, including acute lymphoblastic leukemia (ALL) in the first or second complete remission, acute myeloid leukemia (AML) in the first complete remission, myelodysplastic syndrome (MDS), chronic myeloid leukemia (CML) in the chronic phase, acute mixed lineage leukemia (AMLL) in the first complete remission and juvenile myelomonocytic leukemia (JMML), 3) advanced stage hematologic malignancies, including ALL in greater than the second complete remission, CML in the accelerated phase, AMLL beyond the first complete remission and acute leukemia in partial remission.
Definition: Seattle clinical criteria were used for VOD diagnosis. A diagnosis of VOD required two of the following within 20 days of transplantation; serum bilirubin >2 mg/dL (34 µM/L), hepatomegaly and weight gain >2% over baseline.
Severity: The severity of VOD was classified as mild, moderate or severe. Mild VOD was defined as the absence of adverse effects of liver dysfunction with complete resolution of symptoms and signs. Moderate VOD was characterized as the adverse effects of liver dysfunction requiring therapy such as diuretics for fluid retention and analgesics for pain. Severe VOD was defined as the persistence of symptoms after day 100 or death before day 100 with ongoing VOD.
Prophylactic heparin (Heparin sodium, Hanlim, Seoul, Korea) was administered using the dose 100 U/kg/day in continuous intravenous infusion, starting on day -7 until day +30. Heparin was discontinued if testing found the activated partial thromboplastin time (aPTT) had increased by 1.2-fold over normal, or if there were any major bleeding episodes. Lipo-PGE1 (Eglandin; alprostadil, Welfide, Osaka, Japan) was continuously intravenously infused at a dose of 1 µg/kg/day from day +1 until day +30. Patients were assigned to receive or not receive prophylaxis according to the decision of each physician.
Associations between VOD, potential risk factors and prophylaxis were tested by univariate analyses using the chi-square test or Fisher's exact test for comparing categorical variables, and t tests for comparing continuous variables. Variables associated with a p<0.1 in univariate analysis were fitted to a logistic regression model for multivariate analysis. Analysis of survival was calculated using the Kaplan-Meier method and log-rank test. All data were analyzed using SPSS version 11.5.
Patient characteristics at the time of transplantation are shown in Table 1. The median age at HSCT was 7.3 yr (range: 0.6 to 15.6 yr). Of a total of 85 patients, 11 received transplantation for non-malignant disease and 74 for malignant disease. Of the 74 patients with malignant disease, 11 were transplanted in the advanced stage of the disease. Conditioning regimens were Bu-based for 65 patients (oral Bu for 33, intravenous Bu for 32), TBI-based for 10, and other regimens in 10 patients that included a case of non-myeloablative conditioning.
VOD developed in 25 of 85 patients (29%) with the median diagnosis day being 11.4 (range: day -4 to day +21). Of 25 patients, 12 had mild VOD (48%), 8 had moderate VOD (32%) and 5 had severe VOD (20%).
Univariate analysis was performed to identify risk factors for VOD (Table 2). Age at transplantation, stem cell source and HLA matching were found not to be risk factors. Similarly, viral status including CMV, HSV, HBV and HCV for either donor or recipient at transplantation had no significant influence on development of VOD. In contrast, disease status was identified as a risk factor, with none of 13 non-malignant disease patients developing VOD, while 20 of 61 patients with early stage hematologic malignancy (36%) and 5 of 11 patients with advanced stage hematologic malignancy (45%) developing VOD (p<0.03). The type of conditioning regimen was also found to affect VOD development (p=0.02), with Bu-based regimens associated with an incidence of 37%, TBI-based regimens associated with an incidence of 10%, and other conditioning regimens associated with an incidence of 0%. There was no difference in VOD incidence according to the formulation of Bu (41% for oral Bu vs. 34% for intravenous Bu, p=0.80). Prophylactic treatment with either low-dose heparin (2/10, 20%) or lipo-PGE1 (14/40, 35%) showed no difference on development of VOD (p=0.53).
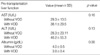
Pre-transplantation liver function and albumin levels were similar for both VOD and non-VOD patients (Table 3). The incidence of VOD in patients with normal liver function (AST <40 IU/L, ALT <40 IU/L, total bilirubin <1.2 mg/dL and albumin >3 g/dL) was 27% (18/68) and that in patients with abnormal liver function was 42% (7/17). However there was no significant difference in the incidence of VOD between two groups (p=0.37).
The median for development of mild/moderate VOD was day +12 (range: -4 to +21), while the median for severe VOD was day +7 (range: +2 to +15) (p>0.05). There were no significant differences in maximum levels of AST, ALT, total bilirubin and ALP after transplantation between patients with mild/moderate VOD and those with severe VOD. While the raw data suggested higher total bilirubin levels in severe VOD compared to mild/moderate VOD patients, statistical analysis did not find this difference significant. Ascites developed in 8 of 20 (40%) mild/moderate VOD patients and 4 of 5 (80%) severe VOD patients (p>0.05). There was no significant difference between the two groups in terms of maximum serum BUN or Cr after transplantation. While renal dysfunction that elevated serum Cr more than twice the baseline level or required dialysis was more frequent in patients with severe VOD, the difference from mild/moderate VOD patients was not statistically significant. However, renal dysfunction was less frequent in patients with mild VOD compared to patients with moderate or severe VOD (p=0.03). The occurrence of pulmonary dysfunction was more common in severe VOD compared to mild/moderate VOD patients (Table 4).
Of the 85 patients, 50 received prophylactic low-dose heparin or lipo-PGE1 treatment for VOD and 35 did not. Although the overall incidence of VOD did not differ between treated and non-treated patients (16/50 vs. 9/35, respectively), fewer patients receiving prophylaxis developed severe VOD compared to patients who did not receive prophylaxis (0/50 vs. 5/35, respectively, p=0.02) (Table 5). None of patients who received either lipo-PGE1 or heparin developed severe VOD.
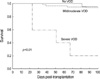
All 5 patients with severe VOD died of causes directly attributable to VOD, leading to an estimated survival rate of 0% at 100 days posttransplant. In contrast, the survival rate for patients with mild/moderate VOD was 95%, and for patients without VOD the rate was 92% (p<0.01) (Fig. 1).
Hepatic VOD is one of the most common life-threatening complications that can occur during HSCT. The incidence of VOD is reported to range from 5% to 60% in adults (1-4, 21, 23), and the incidence of post-transplantation VOD in children is reported to range from 18% to 28%, with the ranges probably reflecting the differences in conditioning regimens, type of graft and patient characteristics (5-8, 24, 25). Comparable to those results, the present retrospective study found that the incidence of hepatic VOD in pediatric patients undergoing allogeneic HSCT was 29%.
Pre-HSCT risk factors for VOD development include old age, elevated transaminases prior to conditioning therapy, previous abdominal radiation and advanced disease (2, 9). Our study found that age at HSCT and pre-transplantation liver function were not risk factors, whereas presence of hematologic malignancy was a risk factor. Reported HSCT-related risk factors for VOD development include conditioning regimen, degree of HLA matching, donor type and positive CMV serology in the recipient (2, 9, 24, 25). In particular, others report a higher incidence of VOD in patients receiving Bu and cyclophosphamide (Cy) compared with those receiving TBI and Cy (26). Similarly, in this study the incidence of VOD in patients using Bu and Cy was 30%, and the incidence of VOD in patients using TBI and Cy was 10%. These data indicate that Bu and Cy conditioning was a risk factor for VOD development, although there was no difference in VOD incidence according to the formulation of Bu. Therefore, the higher incidence of VOD in malignancy compared to non-malignant disease might be associated with conditioning regimens including Bu or TBI that were not used in non-malignant disease. Unlike Carreras et al. (2), the present study found that the degree of HLA matching was not a risk factor. We also found that the incidence of VOD was not affected by stem cell source or viral serology status (CMV, HSV, HBV, HCV) of either the donor or recipient at transplantation. Previous studies have reported that maximum total bilirubin, maximum BUN, maximum Cr and maximum AST levels were higher in severe VOD compared to mild/moderate VOD patients (23, 25).
A previous retrospective study of pediatric patients found that severe VOD was diagnosed earlier than mild/moderate VOD, and that the former was associated with a high incidence of ascites, pulmonary dysfunction and renal dysfunction (25). A study of adults reported that ascites, pleural effusion and renal dysfunction were common in severe VOD (23). In our study, maximum levels of total bilirubin and AST did not differ between mild/moderate and severe VOD patients. However, it may be difficult to draw firm conclusions from these observations as this study included only a relatively small number of severe VOD patients. Possibly reflecting this, although the raw data showed ascites (80%) and renal dysfunction (80%) were observed more frequently in severe VOD patients compared to mild/moderate VOD patients, this difference did not reach statistical significance. We found that pulmonary dysfunction requiring O2 supply or intubation occurred more frequently in severe VOD than in mild/moderate VOD patients, as reported elsewhere (23).
Recently, several centers conducted studies examining the use of defibrotide (DF) to treat VOD. A multicenter study found the complete response rate in severe VOD patients was 50% for pediatric patients (27) and 36% in children and adults (28).
While DF is a partially successful therapeutic treatment for severe VOD, administration of prophylactic treatments is generally considered a superior strategy. However, currently there are no effective prophylactic treatments for VOD. Prophylactic strategies have included administration of low-dose heparin or PGE1. One randomized study has demonstrated that low-dose heparin reduced the overall incidence of VOD (18). There has been a few trials reporting that PGE1 or lipo-PGE1 is an effective prophylacxis for VOD (21, 22). The limited number of studies in this area indicates there is a critical lack of data regarding these putative prophylactic approaches for VOD.
We found that neither prophylactic low-dose heparin nor lipo-PGE1 reduced the incidence of VOD. However, these prophylactic strategies reduced the severity of VOD, with no patients treated with low-dose heparin or lipo-PGE1 found to develop severe VOD. However development of severe VOD was not different between patients receiving low-dose heparin and those receiving lipo-PGE1. This observation may have particular clinical significance given that no severe VOD patients survived more than 100 days in the present study, whereas the non-severe VOD survival rate was greater than 90%. In regard to mortality rates reported by others, Barker et al. (24) found that the post-transplantation mortality rate at day 100 was 38.5%, and that severe VOD was associated with a mortality rate of 98% by day 100 after HSCT.
The present study made a number of significant findings. First, pediatric patients with non-malignant disease developed VOD less frequently than those with malignant disease, and the stage of hematologic malignancy did not affect the incidence of VOD. Second, pediatric patients who received Bubased conditioning regimens developed VOD more frequently than those receiving TBI-based or other regimens. Finally, VOD was less severe in pediatric patients administered prophylactic lipo-PGE1 or low-dose heparin. These data indicate that administration of prophylactic low-dose heparin or lipo-PGE1 may improve outcomes after HSCT in children. The present findings highlight the need for a randomized prospective study using a larger cohort.
Figures and Tables
Table 1
Patient characteristics at the time of transplantation

SAA, severe aplastic anemia; PRCA, pure red cell anemia; CGD, chronic granulomatous disease; ALL, acute lymphoblastic leukemia; AML, acute myeloid leukemia; MDS, myeloysplastic syndrome; CML, chronic myeloid leukemia; AMLL, acute mixed lineage leukemia; JMML, juvenile myelomonocytic leukemia; HLH, hemophagocytic lymphoproliferate syndrome; HM, hematologic malignancy; CR, complete remission; PR, partial remission; Bu, busulfan; Cy, cyclophosphamide; VP16, Etoposide; Mel, melphalan; Flu, fludarabin; ATG, anti-thymocyte globulin; VOD, veno-occlusive disease.
References
1. McDonald GB, Hinds MS, Fisher LD, Schoch HG, Wolford JL, Banaji M, Hardin BJ, Shulman HM, Clift RA. Veno-occlusive disease of the liver and multiorgan failure after bone marrow transplantation: a cohort study of 355 patients. Ann Intern Med. 1993. 118:255–267.

2. Carreras E, Bertz H, Arcese W, Vernant JP, Tomas JF, Hagglund H, Bandini G, Esperou GB, Russell J, Rubia J, Girolamo GD, Demuynck H, Hartmann O, Clausen J, Ruutu T, Leblond V, Iriondo A, Bosi A, Ben-Bassat I, Koza V, Gratwohl A, Apperley JF. Incidence and outcome of hepatic veno-occlusive disease after blood or marrow transplantation: a prospective cohort study of the European Group for Blood and Marrow Transplantation. Blood. 1998. 92:3599–3604.
3. Jones RJ, Lee KS, Beschorner WE, Vogel VG, Grochow LB, Braine HG, Vogelsang GB, Sensenbrenner LL, Santos GW, Saral R. Venoocclusive disease of the liver following bone marrow transplantation. Transplantation. 1987. 44:778–783.

4. Ayash LJ, Hunt M, Antman K, Nadler L, Wheeler C, Takvorian T, Elias A, Antin JH, Greenough T, Eder JP. Hepatic venoocclusive disease in autologous bone marrow transplantation of solid tumors and lymphomas. J Clin Oncol. 1990. 8:1699–1706.

5. Hasegawa S, Horibe K, Kawabe T, Kato K, Kojima S, Matsuyama T, Hirabayashi N. Veno-occlusive disease of the liver after allogeneic bone marrow transplantation in children with hematologic malignancies: incidence, onset time and risk factors. Bone Marrow Transplant. 1998. 22:1191–1197.

6. Ozkaynak MF, Weinberg K, Kohn D, Sender L, Parkman R, Lenarsky C. Hepatic veno-occlusive disease post-bone marrow transplantation in children conditioned with busulfan and cyclophosphamide: incidence, risk factors, and clinical outcome. Bone Marrow Transplant. 1991. 7:467–474.
7. Meresse V, Hartmann O, Vassal G, Benhamou E, Valteau-Couanet D, Brugieres L, Lemerle J. Risk factors for hepatic veno-occlusive disease after high-dose busulfan-containing regimens followed by autologous bone marrow transplantation: a study in 136 children. Bone Marrow Transplant. 1992. 10:135–141.
8. Rosenthal J, Sender L, Secola R, Killen R, Millerick M, Murphy L, Cairo MS. Phase II trial of heparin prophylaxis for veno-occlusive disease of the liver in children undergoing bone marrow transplantation. Bone Marrow Transplant. 1996. 18:185–191.
9. Bearman SI. The syndrome of hepatic veno-occlusive disease after marrow transplantation. Blood. 1995. 85:3005–3020.

10. Rozman C, Carreras E, Qian C, Galo RP, Bortin MM, Rowlings PA, Ash RC, Champlin RF, Henslee-Downey PJ, Herzig RH, Hinterberger W, Klein JP, Prentice HG, Reiffers J, Zwaan FE, Horowitz MM. Risk factors for hepatic veno-occlusive disease following HLA-identical sibling bone marrow transplants for leukemia. Bone Marrow Transplant. 1996. 17:75–80.
11. Kami M, Mori S, Tanikawa S, Akiyama H, Onozawa Y, Tanaka T, Okamoto R, Maeda Y, Sasaki T, Kaku H, Matsuura Y, Hiruma K, Sakamaki H. Risk factors for hepatic veno-occlusive disease after bone marrow transplantation: retrospective analysis of 137 cases at a single institution. Bone Marrow Transplant. 1997. 20:397–402.

12. Wadleigh M, Richardson PG, Zahrieh D, Lee SJ, Cutler C, Ho V, Alyea EP, Antin JH, Stone RM, Soiffer RJ, DeAngelo DJ. Prior gemtuzumab ozogamicin exposure significantly increases the risk of venoocclusive disease in patients who undergo myeloablative allogeneic stem cell transplantation. Blood. 2003. 102:1578–1582.

13. Rajvanshi P, Shulman HM, Sievers EL, McDonald GB. Hepatic sinusoidal obstruction after gemtuzumab ozogamicin (Mylotarg) therapy. Blood. 2002. 99:2310–2314.

14. Giles FJ, Kantarjian HM, Kornblau SM, Thomas DA, Garcia-Manero G, Waddelow TA, David CL, Phan AT, Colburn DE, Rashid A, Estey EH. Mylotarg (gemtuzumab ozogamicin) therapy is associated with hepatic venoocclusive disease in patients who have not received stem cell transplantation. Cancer. 2001. 92:406–413.

15. Nabhan C, Rundhaugen L, Jatoi M, Riley MB, Boehlke L, Peterson LC, Tallman MS. Gemtuzumab ozogamicin (Mylotarg™) is infrequently associated with sinusoidal obstructive syndrome/veno-occlusive disease. Ann Oncol. 2004. 15:1231–1236.
16. Tack DK, Letendre L, Kamath PS, Tefferi A. Development of hepatic veno-occlusive disease after Mylotarg infusion for relapsed acute myeloid leukemia. Bone Marrow Transplant. 2001. 28:895–897.

17. Cohen AD, Luger SM, Sickles C, Mangan PA, Porter DL, Schuster SJ, Tsai DE, Nasta S, Gewirtz AM, Stadtmauer EA. Gemtuzumab ozogamicin (Mylotarg) monotherapy for relapsed AML after hematopoietic stem cell transplant: efficacy and incidence of hepatic venoocclusive disease. Bone Marrow Transplant. 2002. 30:23–28.

18. Attal M, Huguet F, Rubie H, Huynh A, Charlet JP, Payen JL, Voigt J, Brousset P, Selves J, Muller C, Pris J, Laurent G. Prevention of hepatic venoocclusive disease after bone marrow transplantation by continuous infusion of low-dose heparin: a prospective, randomized trial. Blood. 1992. 79:2834–2840.
19. Park SH, Lee MH, Lee H, Kim K, Kim WS, Jung CW, Im YH, Yoon SS, Kang WK, Park K, Park CH, Kim SW. A randomized trial of heparin plus ursodiol vs heparin alone to prevent hepatic veno-occlusive disease after hematopoietic stem cell transplantation. Bone Marrow Transplant. 2002. 29:137–143.

20. Vaughan DE, Plavin SR, Schafer AI, Loscalzo J. PGE1 accelerates thrombolysis by tissue plasminogen activator. Blood. 1989. 73:1213–1217.
21. Gluckman E, Jolivet I, Scrobohaci ML, Devergie A, Traineau R, Bourdeau-Esperou H, Lehn P, Faure P, Drouet L. Use of prostaglandin E1 for prevention of liver veno-occlusive disease in leukaemic patients treated by allogeneic bone marrow transplantation. Br J Haematol. 1990. 74:277–281.

22. Cho B, Sung IK, Kim DW, Lee HJ, Kim SY, Chung NG, Kim CC, Kim HK. A trial use of prophylactic low-dose lipo PGE1 (Eglandin) for the prevention of hepatic veno-occlusive disease after hematopoietic stem cell transplantation in children with hematologic malignancies. Korean J Pediatr Hematol Oncol. 2000. 7:242–248.
23. Litzow MR, Repoussis PD, Schroeder G, Wismayer DS, Batts KP, Anderson PM, Arndt CA, Chen MG, Gastineau DA, Gertz MA, Inwards DJ, Lacy MQ, Tefferi A, Noel P, Solberg LA Jr, Letendre L, Hoagland HC. Veno-occlusive disease of the liver after blood and marrow transplantation: analysis of pre- and post-transplant risk factors associated with severity and results of therapy with tissue plasminogen activation. Leuk Lymphoma. 2002. 43:2099–2107.
24. Barker CC, Butner JD, Anderson RA, Brant R, Sauve RS. Incidence, survival and risk factors for the development of veno-occlusive disease in pediatric hematopoietic stem cell transplant recipients. Bone Marrow Tranaplant. 2003. 32:79–87.

25. Reiss U, Cowan M, McMillian A, Horn B. Hepatic venoocclusive disease in blood and bone marrow transplantation in children and young adults: incidence, risk factors, and outcome in a cohort of 241 patients. J Pediatr Hematol Oncol. 2002. 24:746–750.

26. Ringden O, Ruutu T, Remberger M, Nikoskelainen J, Volin L, Vindelev L, Parkkali T, Lenhoff S, Sallerfors B, Ljungman P, Mellander L, Jacobsen N. A randomized trial comparing busulfan with total body irradiation as conditioning in allogeneic marrow transplant recipients with leukemia: a report from the Nordic Bone Marrow Transplantation Group. Blood. 1994. 83:2723–2730.

27. Corbacioglu S, Greil J, Peters C, Wulffraat N, Laws HJ, Dilloo D, Strahm B, Gross Wieltsch U, Sykora KU, Ridolfi-Lüthy A, Basu O, Gruhn B, Güngör T, Mihatsch W, Schulz AS. Defibrotide in the treatment of children with veno-occlusive disease: a retrospective multicentre study demonstrates therapeutic efficacy upon early intervention. Bone Marrow Tranaplant. 2004. 33:189–195.
28. Richardson PG, Murakami C, Jin Z, Warren D, Momtaz P, Hoppensteadt D, Strahm B, Gross-Wieltsch U, Sykora KW, Ridolfi-Lüthy A, Basu O, Gruhn B, Güngör T, Mihatsch W, Schulz AS. Multi-institutional use of defibrotide in 88 patients after stem cell transplantation with severe veno-occlusive disease and multisystem organ failure: response without significant toxicity in a high-risk population and factors predictive of outcome. Blood. 2002. 100:4337–4343.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download