Abstract
We report our experience in 13 patients who underwent transcatheter closure of Fontan fenestration with the Cook® detachable coils. These patients underwent the extracardiac type Fontan operation with a short conduit fenestration (n=7) or lateral tunnel type with a punch-hole fenestration (n=6). Fenestration closure was done at the mean age of 5.1±2.4 yr, average of 32 months after the Fontan operation. We used one to three coils depending on the fenestration type, size, and residual shunt. Aortic oxygen saturations increased by an average of 5.4 (2-9)% and mean pressures in the Fontan circuit increased by an average of 2.1 (0-6) mmHg. During fol-low-up (median of 23 months), five patients (4 in extracardiac, 1 in lateral tunnel) had complete occlusion of the fenestration on echocardiography. There was no immediate or late complication. Transcatheter closure of fenestration in Fontan operation using the Cook® detachable coil is a safe and feasible technique. However, the coil was ineffective for closure of a punch-hole fenestration in the lateral tunnel type operation. In the conduit type fenestration, some modification of fenestration method instead of a short conduit for coil closure or use of new device is necessary to increase complete closure rate.
Since the first description in 1971, there have been many modifications of the Fontan operation to reduce mortality and morbidity (1-4). Fenestration in the Fontan type operation allows right to left shunting that reduces Fontan pathway pressure and improves cardiac output and short-term clinical outcome in the standard-risk population (5, 6). However, persistent right-to-left shunting results in cyanosis and increases the risk of paradoxical embolism (7). For these reasons, fenestration closure is recommended after recovery from the Fontan surgery (8, 9) and several devices have been used to close the fenestration. We tried transcatheter closure of the fenestration with the Cook® detachable coils because public medical insurance does not allow other expensive devices but coils. This report describes our experience of transcatheter closure of Fontan fenestration with the Cook® detachable coils.
A total of 22 patients have undergone examination for transcatheter closure of the Fontan fenestration in our hospital since 1998. These patients had persistent systemic desaturation and no signs of increased systemic venous pressure and/or low cardiac output such as hepatomegaly, ascites or edema. In 9 patients, closure was not tried because of high Fontan pathway pressure in 6 patients, inability to pass a catheter through the fenestration in 2 patients, and too large fenestration for coil occlusion in 1 patient.
Transcatheter closure of the Fontan fenestration was performed in 13 patients. Their average age at the time of the procedure was 5.1±2.4 (2.7-11.7, median of 4.3) yr. Their previous diagnoses are listed in Table 1. The patients underwent two types of Fontan operation. One was an extracardiac type Fontan operation with a short conduit as a fenestration in 7 patients (5 or 6 mm of fenestration) and the other was a lateral tunnel type Fontan with a punch-hole adjustable fenestration in 6 patients (3.5-5.0 mm of fenestration, unknown in 1 patient). The fenestration closure was done at an average of 32 (9-123, median of 17) months after the Fontan operation.
We reviewed the medical records of the patients to ascertain demographic, echocardiographic, hemodynamic and angiographic data. Presence of residual shunt after closure was evaluated by angiography at the cardiac catheterization lab and thereafter by echocardiography. After discharge, resting oxygen saturation was measured transcutaneously in room air.
Transthoracic echocardiography was performed before cardiac catheterization to detect a possible thrombus and to evaluate patency of the fenestration.
We evaluated arterial and venous collaterals by angiograms at the aorta, subclavian arteries, superior vena cava or innominate vein, and pulmonary artery. After closure of collaterals, we measured the pressures and oxygen saturations at several sites of the Fontan circuit, left ventricle and aorta. We then performed a test occlusion of the fenestration with the Swan-Ganz catheter and confirmed complete occlusion by angiogram at the inferior vena cava (IVC)-to the pulmonary artery baffle. About 15 to 20 min after the test occlusion we measured the changes of pressure and oxygen saturation within the Fontan circuit, left atrium and aorta.
The criteria for fenestration closure was: right atrial pressure ≤18 mmHg, increase in the difference of arteriovenous oxygen saturation ≤33%, right atrial saturation ≥40%, and increase in the mean RA pressure <4 mmHg (10, 11). If the changes of pressure and cardiac output were acceptable, one or more detachable coils (Cook® Flipper™ PDA closure detachable coil) were implanted.
We used heparin during the procedure and warfarin and/or aspirin thereafter.
The results of the fenestration closure depending on the type of Fontan operation were compared with the Fisher's exact test. The differences of oxygen saturation and baffle pressure between pre- and post-fenestration closure were compared with Wilcoxon two-sample test in SAS version 9.1.
We used one coil in eight patients (8 mm×3 loops in 3 patients; 5 mm×3 loops in 3 patients; 6.5 mm×4 loops in 2 patients), 2 coils in four patients (8 mm×4 loops+5 mm×3 loops; 8 mm×4 loops+6.5 mm×4 loops; 8 mm ×3 loops+6.5 mm×4 loops; 6.5 mm×4 loops+5 mm×4 loops) and three coils in one patient (6.5 mm×4 loops+5 mm×4 loops+5 mm×3 loops). Out of the 6 patients who underwent the lateral tunnel type Fontan operation, a single coil was used in four patients and two coils in two patients. Out of the 7 patients who underwent the extracardiac type Fontan operation, a single coil was used in four patients, two coils in two patients and three coils in one.
We did not measure the fenestration size on angiogram in all patients, but there was any case with significant narrowing of fenestration. At first we used single coil larger than the fenestration size at the operation, but later we preferred multiples coils because of low probability of delayed complete closure. It was decided depending on the residual shunt amount on angiogram after initial coil deployment whether to put an additional coil or not. We tried to put one or less loop of the coil in the left atrial side and one to two loops in the baffle side (Fig. 3, 4).
Before and after fenestration closure, oxygen saturation data at the femoral artery are presented in Table 2. Aortic oxygen saturations increased by an average of 5.4 (2-9)%. After closure of the fenestration, oxygen saturation increased in all cases. There was no significant difference in oxygen saturation change between the two types of Fontan operation (p=1.0).
The pressure change data in the Fontan circuit is presented in Table 3. Mean pressures in the Fontan circuit increased by an average of 2.1 mmHg (range, 0 to 6 mmHg). In patients who underwent the lateral tunnel type Fontan operation, the increase of the Fontan circuit pressure was less than in the extracardiac type (average 1.5 vs. 2.6 mmHg). However, there was no statistical difference (p=0.2258). The pressure in the Fontan pathway increased in all patients but one.
There was no immediate complication in catheterization laboratory. In one of six patients with the lateral tunnel type Fontan operation and in four of seven patients with the extracardiac Fontan operation, the fenestrations closed immediately as observed by angiography and echocardiography. The median follow up duration after the fenestration closure was 23 (11-86) months.
The most recent transcutaneous oxygen saturation data is shown in Table 2 and Fig. 1, 2. The latest saturation was an average of 91.5 (88.0-96.0)% for the lateral tunnel type and 93.3 (86.0-93.3)% for the extracardiac type. Between the two groups, there was no statistical difference in the change of pre- and post-procedure oxygen saturation (mean difference of 5.6% in the lateral tunnel type versus 5.2% in the extracardiac type; p=0.7802).
The most recent echocardiograms showed complete occlusion of the fenestration in five of 13 patients (4 in extracardiac type and 1 in lateral tunnel type). One patient with the extracardiac type Fontan operation had immediate complete occlusion. Six months later, however, an echocardiogram revealed recanalization of the fenestration. Only one patient with the extracardiac type showed delayed complete closure at 14 months after the fenestration closure.
Finally, eight patients (3 in extracardiac type and 5 in lateral tunnel type) had small residual shunt. The complete closure rate was higher in the extracardiac type, but in this small sample, the difference was not statistically significant (p=0.2657).
There have been no immediate or late complications such as coil embolization, thromboembolic events, or documented hemolysis during follow-up.
Results depending on the fenestration size are shown in Table 4. Out of the 13 patients, 1 of 1 patient with 3.5 mm fenestration, 2 of 5 patients with 5 mm fenestration and 2 of 4 patients with 6 mm fenestration had complete occlusion. In one patient, fenestration size was not known.
Before the procedure, 12 of a total of 13 patients had taken warfarin and/or aspirin (warfarin in 5 patients, aspirin in 3 patients, warfarin and aspirin in 4 patients). After the procedure, all patients took warfarin and/or aspirin (warfarin in 3 patients, aspirin in 2 patients, warfarin and aspirin in 8 patients).
One patient with the lateral tunnel type Fontan operation, who had trivial residual leakage on immediate echocardiography, underwent follow-up catheterization 2 yr after the procedure due to progressive cyanosis. His initial pressure in the Fontan pathway before the fenestration closure was 6 mmHg and the pressure after fenestration closure was 9 mmHg. On the follow-up angiograms, there were only several minor collateral arteries but no significant collateral veins. An angiogram at the baffle revealed a small patent fenestration (size=3.3 mm). After a test occlusion, the pressure in the Fontan circuit increased to 18 mmHg from 11 mmHg. We decided not to close the residual fenestration according to our procedure protocol.
Although the fenestration in the Fontan procedure can improve immediate postoperative course, it may result in persistent cyanosis and paradoxical embolism. There is still debate about whether to close the fenestration or not. Recent reports support the need for fenestration closure. Goff et al. (9) reported that fenestration closure is followed by improved oxygenation, reduced need for anticongestive medication and improved somatic growth. They recommended that patients with fenestrated Fontan procedure should undergo late (>6 months after surgery) transcatheter closure if O2 saturations are <90% and test occlusion is tolerated.
Several devices have been used to close the fenestration. In the extracardiac type Fontan operation with a conduit fenestration, coils (12-14) and the Amplatzer duct occluder (15) were used with successful results. In several studies, the attempts at fenestration closure in the lateral tunnel type Fontan operation were carried out using atrial septal occluders such as the Amplatzer septal occluder (8, 16, 17), Clamshell (18) or CardioSEAL (9) with excellent results. Unfortunately, in our country, the use of septal occluders or the Amplatzer duct occluder for fenestration closure is not allowed by public medical insurance system.
Data from our study showed that fenestration closure with coils was more efficient in the extracardiac type Fontan operation than in the lateral tunnel type (57% vs. 16%) even though there was no statistical difference. In the lateral tunnel type Fontan operation, only one case with a 3.5 mm fenestration had complete occlusion of the fenestration. We thought a punch-hole fenestration in the lateral tunnel type was not suitable for closure with coils.
However, even in patients with the extracardic type Fontan operation, the complete closure rate was only 57%. It seems that the low rate of complete closure is related to the shape of the fenestration graft. In our cases, the fenestration graft used in the extracardiac type Fontan was a short (about 7 mm) straight tube. There was no case of spontaneous fenestration closure in our patients with this kind of fenestration graft. In addition, the shape might contribute to the low complete closure rate because a coil cannot be easily tangled in this type of graft. In other studies using coils (12, 13) more than half of the complete closure cases were delayed complete occlusion. There have been some modifications to fenestration graft to increase closure rate. Bradley et al. (12) made the fenestration graft narrow with surgical clip across the midportion to facilitate later fluoroscopic localization and subsequent transcatheter coil occlusion of persistent fenestrations. In that report there was spontaneous closure in 56% of patients who underwent the fenestrated Fontan operation. Kim et al. (14) also used a long angled tube graft to facilitate coil embolization. Comparing the closure rates and pattern in these reports, we thought a short straight conduit in extracardiac type Fontan was not good for later coil occlusion. It would be better to make some modifications to fenestration graft to increase complete closure rate with coils or to use other devices such as the Amplatzer vascular plug which becomes available recently.
Anticoagulation therapy, taken by most of our cases, also contributed to the low rate of complete closure. The Cook® Flipper™ PDA closure detachable coil is designed as a platinum or stainless steel coil with spaced synthetic fibers to promote maximum thrombogenicity. Therefore, anticoagulation therapy in our cases might prevent complete closure of the fenestration.
The difference of oxygen saturation between immediately after the fenestration closure and at the most recent follow-up evaluation was noted in our data. The findings may be partially due to the method of data collection. Data on immediate oxygen saturation after the fenestration closure was obtained during sedation, but follow-up data was obtained at an out-patient clinic. In addition, development of new small venous collaterals after fenestration closure was a possible explanation.
One patient who had trivial leakage immediately after fenestration closure developed a substantial flow through the fenestration with decrease of oxygen saturation (94% to 91%). During the cardiac catheterization, he showed a significant increase of pressure in the Fontan circuit after the test occlusion (initial Fontan pathway pressure before closure, 6 mmHg; post-closure, 9 mmHg; follow-up Fontan pathway pressure before test occlusion, 11 mmHg; after test occlusion, 18 mmHg). Because there was no significant veno-venous collaterals, desaturation was thought to be by reopening of the fenestration. Increased flow through the fenestration on echocardiogram and increased Fontan pathway pressure can explain increased right to left shunting through the fenestration as well as reopening of the fenestration by increased pressure. If there was complete closure of the fenestration using the atrial septal occluder, the patient would suffer from complications due to high systemic venous pressure.
In conclusion, transcatheter closure of the fenestration in the Fontan operation with detachable coil is a safe and feasible technique. However, the coil was ineffective for closure of a punch-hole fenestration in the lateral tunnel type operation. In the extracardiac type Fontan operation, the detachable coil is also not ideal for closure of a short straight conduit fenestration. Modifications to fenestration conduit such as a long redundant fenestration graft or clipped tube fenestration graft would be helpful for the fenestration closure with coil. Other closure device such as the Amplatzer vascular plug can be considered for complete closure of a short conduit.
Figures and Tables
Fig. 1
Before and immediately after the fenestration closure and the latest systemic oxygen saturation in the patients with complete closure of fenestration.
Fig. 2
Before and immediately after the fenestration closure and the latest systemic oxygen saturation in the patients with incomplete closure of fenestration.

Fig. 3
Angiogram after fenestration closure in a patient who underwent lateral tunnel type Fontan operation. One loop of the coil is in the pulmonary atrial side, and the remained two loops are in the IVC-to-PA baffle. There is small residual shunt through the coil. IVC, inferior vena cava; PA, pulmonary artery.
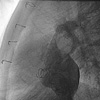
Fig. 4
Fenestration closure in a patient who underwent extracardiac type Fontan operation with a short conduit (A) as a fenestration. An angiogram shows the flow through this short conduit (B, arrow). There is small shunt on an angiogram (D) after the first coil detachment (C). Therefore we put the second (E) and the third coil (F) one by one. There is no significant residual fenestration flow after insertion of three coils (G).

Table 2
Before and immediately after the fenestration closure and the latest systemic oxygen saturation (average; [range])
References
1. de Leval MR, Kilner P, Gewillig M, Bull C. Total cavopulmonary connection: a logical alternative to atriopulmonary connection for complex Fontan operations. Experimental studies and early clinical experience. J Thorac Cardiovasc Surg. 1988. 96:682–695.
3. Gundry SR, Razzouk AJ, del Rio MJ, Shirali G, Bailey LL. The optimal Fontan connection: a growing extracardiac lateral tunnel with pedicled pericardium. J Thorac Cardiovasc Surg. 1997. 114:552–558.

4. Marcelletti C, Corno A, Giannico S, Marino B. Inferior vena cavapulmonary artery extracardiac conduit. A new form of right heart bypass. J Thorac Cardiovasc Surg. 1990. 100:228–232.
5. Bridges ND, Lock JE, Castaneda AR. Baffle fenestration with subsequent transcatheter closure. Modification of the Fontan operation for patients at increased risk. Circulation. 1990. 82:1681–1689.

6. Laks H, Pearl JM, Haas GS, Drinkwater DC, Milgalter E, Jarmakani JM, Isabel-Jones J, George BL, Williams RG. Partial Fontan: advantages of an adjustable interatrial communication. Ann Thorac Surg. 1991. 52:1084–1094.

7. Rosenthal DN, Friedman AH, Kleinman CS, Kopf GS, Rosenfeld LE, Hellenbrand WE. Thromboembolic complications after Fontan operations. Circulation. 1995. 92:II287–II293.

8. Cowley CG, Badran S, Gaffney D, Rocchini AP, Lloyd TR. Transcatheter closure of Fontan fenestrations using the Amplatzer septal occluder: initial experience and Follow-up. Catheter Cardiovasc Interv. 2000. 51:301–304.

9. Goff DA, Blume ED, Gauvreau K, Mayer JE, Lock JE, Jenkins KJ. Clinical outcome of fenestrated Fontan patients after closure: the first 10 years. Circulation. 2000. 102:2094–2099.
10. Bridges ND, Lock JE, Mayer JE Jr, Burnett J, Castaneda AR. Cardiac catheterization and test occlusion of the interatrial communication after the fenestrated Fontan operation. J Am Coll Cardiol. 1995. 25:1712–1717.

11. Hijazi ZM. Extracardiac fenestrated Fontan operation: to close or not to close the fenestration? Catheter Cardiovasc Interv. 2001. 54:93–94.

12. Bradley TJ, Human DG, Culham JA, Duncan WJ, Patterson MW, LeBlanc JG, Sett SS. Clipped tube fenestration after extracardiac Fontan allows for simple transcatheter coil occlusion. Ann Thorac Surg. 2003. 76:1923–1928.

13. Sommer RJ, Recto M, Golinko RJ, Griepp RB. Transcatheter coil occlusion of surgical fenestration after Fontan operation. Circulation. 1996. 94:249–252.

14. Kim SJ, Lee JY, Song JY, Kim YH. Catheter closure of tube graft fenestration in extracardiac Fontan operation. Int J Cardiol. 2005. 104:224–226.

15. Rueda F, Squitieri C, Ballerini L. Closure of the fenestration in the extracardiac Fontan with the Amplatzer duct occluder device. Catheter Cardiovasc Interv. 2001. 54:88–92.

16. Moore JW, Murdison KA, Baffa GM, Kashow K, Murphy JD. Transcatheter closure of fenestrations and excluded hepatic veins after Fontan: versatility of the Amplatzer device. Am Heart J. 2000. 140:534–540.

17. Tofeig M, Walsh KP, Chan C, Ladusans E, Gladman G, Arnold R. Occlusion of Fontan fenestrations using the Amplatzer septal occluder. Heart. 1998. 79:368–370.

18. Mavroudis C, Zales VR, Backer CL, Muster AJ, Latson LA. Fenestrated Fontan with delayed catheter closure. Effects of volume loading and baffle fenestration on cardiac index and oxygen delivery. Circulation. 1992. 86:II85–II92.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download