Abstract
Intradural lumbar disc herniation is a rare pathological entity. The pathogenesis of intradural lumbar disc herniation is not known clearly. Intradural disc herniations usually occurred at the L4-L5 levels but have also been reported at other levels. However, intradural disc herniation at L5-S1 is quite rare. There are approximately nine reports in the English literature of intraradicular disc herniation at L5-S1. We described a 61-yr-old man with suspected intradural mass at the level of L5-S1 space. The patient presented with pain in the lower back and both lower legs for 4 months and a sudden exacerbation of the symptoms for 3 days. Gadolinium-enhanced magnetic resonance imaging (MRI) demonstrated a large disc herniation at the L5-S1 level with an intradural component. L5 and S1 laminectomy was performed, and dura was swollen and immobile. Subsequent durotomy was performed and an intradural disc fragment was removed. The patient had full recovery in 3 months. Intradural lumbar disc herniation must be considered in the differential diagnosis of mass lesions in the spinal canal. Contrast-enhanced MRI scans are useful to differentiate a herniated disc from a disc space infection or tumor.
Rupture of intervertebral disc material into the intradural space is a rare event in lumbar disc disease but must be considered in the differential diagnosis of mass lesion causing nerve root or cauda equina syndromes. The pathogenesis of lumbar intradural disc herniation is most likely related to dense adhesion between the ventral dura mater and the posterior longitudinal ligament. These adhesions can apparently result either from repeated minor trauma or from prior surgery. Intradural disc herniations are usually seen at L4-L5 and L3-L4, but have also been reported at other levels. There are approximately nine reports in the English literature of intraradicular disc herniation at L5-S1. However, intradural disc herniation at L5-S1 is quite rare. This report presents a case of intradural disc herniation at L5-S1 mimicking an intradural extramedullary spinal tumor.
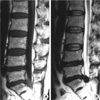
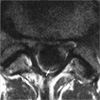
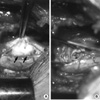
A 61-yr-old man was admitted to hospital having experienced pain in the lower back and both lower legs for 4 months and a sudden exacerbation of the symptoms for 3 days before admission. He had no history of trauma or previous lower back surgery. Neurological examination revealed weakness of the extensor hallucis longus and decreased ankle reflex in both lower extremities. Straight leg raise was positive at 30° bilaterally. A sensory deficit over the saddle area was observed, but bladder and bowel function were normal. Magnetic resonance imaging (MRI) showed a mass-like lesion at the level of L5-S1 space (Fig. 1). Gadolinium-enhanced MRI demonstrated a large disc herniation at the L5-S1 level with an intradural component (Fig. 2). He underwent L5 and S1 laminectomy. The dura was swollen and immobile. Subsequent durotomy demonstrated a 1×2 cm mass occupying the spinal canal with peripheral displacement of the nerve roots (Fig. 3). Careful excision of the disc fragment revealed a 0.4×0.4 cm defect in the anterior thecal sac, which was firmly adherent. An anterior dural defect was found communicating with the L5-S1 interspace. A frozen section confirmed the presence of a disc fragment without neoplastic activity. Discectomy was completed and the thecal defect closed. The patient's postoperative period was uneventful and he gained full recovery in 3 months.
Intradural disc herniations comprise 0.27% of all herniated Intradural Disc Herniation at L5-S1 discs (1). Lumbar intradural disc rupture must be considered in the differential diagnosis of mass lesions causing nerve root or cauda equina syndromes. Approximately 123 cases of intradural disc herniations have been reported since 1942 (2). The majority of them occurred at the L4-L5 levels and only 12 cases occurred at L5-S1. Mut et al. (3) suggested the following classification for intradural disc herniations. Type A: Herniation of a disc into the dural sac. Type B: Herniation of a disc into the dural sheath in the preganglionic region of the nerve root. Type B intradural disc herniation has been named intraradicular disc herniation. This terminology is confusing and actually indicates a special type of disc herniation through the dural sheath of the nerve root but not within the epineurium. Therefore, describing Type B as an intraradicular disc herniation is more specific and certain. Type B intradural disc herniations are much less frequent. Of the 12 cases of intradural disc herniation were reported at L5-S1, 9 belonged to Type B intradural disc herniation and the other 3 could not be classified due to the absence of any comment of their type. Ten cases of Type B intradural disc herniation have been reported, and all were in the lumbar region: 9 in the S1 nerve root and one in the L5 nerve root (3-6). There are approximately nine reports in the English literature of intraradicular disc herniation at L5-S1. However, Type A intradural disc herniation at L5-S1 is quite rare. This report presents a case of Type A intradural disc herniation at L5-S1 mimicking an intradural extramedullary spinal tumor.
The exact mechanism of the dural tear by a herniated disc is not known clearly. An anatomical investigation revealed dense non-separable adhesions of the ventral dura to the posterior longitudinal ligament at the L4-L5 level in eight of 40 cadavers (7). It was suggested that adhesions formed congenitally or caused by trauma, surgery, inflammation, osteophytes or disc protrusion fixed the dural sac. A study of fresh adult cadavers by Spencer et al. (8) demonstrated the existence of dural ligaments fixing the dura and nerve roots at their exit from the main dural sac to the posterior longitudinal ligament and vertebral body periosteum proximal to the intervertebral disc. Distal fixation generally occurs at the intervertebral foramen where the epineural sheath of the spinal nerve is attached. These ligaments in certain cases also cause increased nerve root fixation, thereby allowing penetration of a ruptured disc to the S1 root. The reason why Type A herniations occur at the L4-L5 intervertebral disc space and Type B at L5-S1 is also yet be elucidated. The postulated mechanism is adhesions in both Type A and Type B. Although intraradicular disc herniation are frequently seen at the L5-S1, Type A intradural disc herniation could occur at the L5-S1, if adhesions between the ventral dura and the posterior longitudinal ligament are formed congenitally or caused by trauma, surgery, inflammation at the L5-S1 level.
It is usually not difficult with current MRI techniques to differentiate lumbar disc herniation from other conditions (2). Contrast-enhanced MRI scans are useful to differentiate a herniated disc from a disc space infection or tumor. Peripheral enhancement around the nonenhancing disc fragment is commonly seen on contrast MRI. A herniated disc fragment will rarely be enhanced centrally, which is attributed to vascular granulation tissue infiltrating the fragment (2).
In our case, the lesion had intermediate signal intensity on T1-weighted and low signal intensity on T2-weighted MRI scans and that led us to suspect an intradural extramedullary tumor lesion. However on contrast MRI scans there was peripheral enhancement of the lesion, which is typical for a disc fragment (9).
While treating lumbar disc disease, the possibility of an intradural disc herniation should be kept in mind for the success of the discectomy and the management of failed back syndrome.
We herein present a case of intradural disc herniation at L5-S1 mimicking an intradural extramedullary spinal tumor that demonstrates the role and the importance of contrast MRI in the diagnosis of intradural disc herniation.
Figures and Tables
References
1. Epstein NE, Syrquin MS, Epstein JA, Decker RE. Intradural disc herniations in the cervical, thoracic, and lumbar spine: report of three cases and review of the literature. J Spinal Disord. 1990. 3:396–403.
2. D'Andrea G, Trillò G, Roperto R, Celli P, Orlando ER, Ferrante L. Intradural lumbar disc herniations: the role of MRI in preoperative diagnosis and review of the literature. Neurosurg Rev. 2004. 27:75–80.
3. Mut M, Berker M, Palaoglu S. Intraradicular disc herniations in the lumbar spine and a new classification of intradural disc herniations. Spinal Cord. 2001. 39:545–548.

4. Aydin MV, Ozel S, Sen O, Erdogan B, Yildirim T. Intradural disc mimicking a spinal tumor lesion. Spinal Cord. 2004. 42:52–54.

5. Suzer T, Tahta K, Coskun E. Intraradicular lumbar disc herniation: Case report and review of the literature. Neurosurgery. 1997. 41:956–959.
6. Tsuji H, Maruta K, Maeda A. Postoperative intraradicular intervertebral disc herniation. Spine. 1991. 61:998–1000.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download