Abstract
Prednisone or prednisolone are the mainstay drug treatments for autoimmune hepatitis in children. However, long-term use of corticosteroid is associated with the risk of steroid-induced toxicities, and this situation requires newer immuno-suppressive agents for the treatment of autoimmune hepatitis, especially in growing children. An 11-yr-old Korean girl with type-1 autoimmune hepatitis discontinued prednisolone due to toxicities, i.e., hirsutism, buffalo hump, and skin striae, and remained clinical and biochemical remission under replacement of deflazacort and ursodeoxycholic acid combination therapy. A follow-up liver biopsy after 19 months of deflazacort and ursodeoxycholic acid treatment showed histologic remission.
Autoimmune hepatitis is a chronic necro-inflammatory hepatitis of unknown etiology. It is characterized by autoantibodies that target against liver-specific and non-organ-specific antigens (1). Corticosteroids, especially prednisone or prednisolone (PD), have been the key drugs of initial antiinflammatory and immuno-suppressive therapy of autoimmune hepatitis in children (2). However, it is well known that long-term use of corticosteroid is associated with the risk of steroid-induced toxicities, and this requires newer immunosuppressive agents for the treatment of autoimmune hepatitis, especially in growing children.
We report on the case of a 11-yr-old Korean girl with type-1 autoimmune hepatitis who discontinued PD due to steroid-induced toxicities, but who remained in biochemical and clinical remission while undergoing deflazacort and ursodeoxycholic acid (UDCA) combination therapy.
A 9-yr-old girl was admitted to Eul-Ji Hospital because of jaundice and right upper quadrant pain. Her height was 135 cm (75-90 percentile), and weight was 43 kg (over 97 percentile). The sclera was icteric, and the liver edge descended 4 cm below the right costal margin. The results of laboratory studies were as follows: aspartate aminotransferanse (AST) 1,106 IU/L, alanine aminotransferase (ALT) 1,888 IU/L, total bilirubin 25.7 mg/dL, direct bilirubin 18.2 mg/dL, total protein 6.9 g/dL, albumin 4.2 g/dL, serum alkaline phosphatase 1,160 IU/L, GGTP 71 IU/L, INR 2.4, aPTT >120 sec, antinuclear antibody (ANA) (+) speckled pattern, with 1:320 titer, anti-smooth muscle antibody (Ab) (-), anti-mitochondrial (AMA Ab) (-), IgG 1,397 mg/dL, anti-HAV IgM (-), anti-HBc IgM (-), HbsAg (-), EBV-VCA IgG/M (-/-), and ceruloplasmin 28 mg/dL. Liver biopsy results showed piecemeal necrosis at the portal-lobular interface accompaning mild to moderate infiltration of lymphocytes, moderate centrilobular cholestasis, moderate lobular inflammation, and moderate fibrosis (Fig. 1). According to the scoring system of International Autoimmune Hepatitis Group (3), she had definite autoimmune hepatitis (score=16). Initially, on 40 mg of PD and 300 mg of UDCA daily, she gradually recovered both clinically and biochemically. PD was tapered gradually, and three months later, she was taking 15 mg of PD and 300 mg of UDCA daily. At eight months, her aminotransferase level had elevated to 400 IU/L, but reduced rapidly when PD was increased to 40 mg/day. At nine months, she was taking 15 mg/day of PD and 300 mg/day of UDCA, but she complained of hirsutism, striae, moon face, and buffalo hump, at ten months. The results of a second round of laboratory studies conducted at this time were; AST 21 IU/L, ALT 52 IU/L, total bilirubin 0.7 mg/dL, total protein 7.2 g/dL, albumin 4.7 g/dL, glucose 86 mg/dL, ANA (+) speckled pattern, with 1:160 titer. Accordingly, deflazacort (Calcort®, HanDok Pharm Co., Ltd, Eumseonggoon, Chungcheongbuk-do, Korea) was administered at dose of 18 mg a day, instead of PD at dose of 18 mg a day, and UDCA was continued. Her biochemical test remained within normal ranges on this regimen, and the PD-associated complications improved rapidly. Fourteen months later, deflazacort was reduced at dose of 15 mg a day, and after 19 months of deflazacort treatment, a follow-up liver biopsy was performed. This showed no lobular activity, no portal activity, near-normal periportal inflammation, and fibrosis (Fig. 2). ANA testing at this time also yielded a negative result (Fig. 3). Deflazacort was discontinued after 25 months and UDCA was discontinued a few months after this. The girl has been in clinical and biochemical remission for two years now, without therapy.
There are few diseases to be differentiated from autoimmune hepatitis, overlap syndrome, in which the features of autoimmune hepatitis is combined with those of primary biliary cirrhosis, or primary sclerosing cholangitis, and autoimmune cholangitis. In overlap with primary biliary cirrhosis, serologic test of AMA is usually positive and histologic study shows findings of cholangitis. In overlap with primary sclerosing cholangitis, serologic test of AMA is negative, and histologic evidence suggests various forms of cholangitis. In autoimmune cholangitis, serologic test of AMA is negative, and histologic examination shows bile duct injury, suggestive of primary biliary cirrhosis. Autoimmune cholangitis, also, is generally not steroid-responsive. In the present case, despite the cholestatic presentation, serum level of GGTP was not so high, histologic study showed no evidence of definite cholangitis, and response to steroid was excellent. According to the scoring system of International Autoimmune Hepatitis Group, this case has definite autoimmune hepatitis (pre-treatment score 16, post-treatment score 18).
The long-term use of corticosteroid is known to be associated with the risk of steroid-induced toxicities. Generally, there are several ways of reducing steroid-associated toxicities, i.e., administering steroid on an alternate-day schedule, administering adjunctive agent to reduce the need for steroid, and finding a substitute agent. However, of these three options in case of autoimmune hepatitis, the risk of relapse is higher if steroids are administered on an alternate-day schedule (4), and thus this method is not recommended. Some authors add azathioprine to steroids if normalization of the liver function is not obtained by steroids alone or if too high a dose of steroids is required to maintain normal transaminase levels (4). Initial combination therapy with steroid and azathioprine, is considered by some authors as standard therapy of autoimmune hepatitis in children, as in adults (1). However, there is concern about the oncogenecity associated with long-term azathioprine therapy (5), and because of its hepatotoxicity, some authors do not recommend azathioprine as first line treatment, particularly in severely jaundiced patients (4). Thus, UDCA was prescribed as an adjuvant medication with PD or deflazacort. In a clinical study on Japanese adults, UDCA improved aminotransferase levels and reduced inflammation in liver biopsy (6); however, a clinical study on Caucasian adults showed no significant difference in the results of biochemical tests or in histologic indices between a UDCA group and a placebo group (7). Thus, the role of UDCA in autoimmune hepatitis warrants further study.
Deflazacort is a synthetic steroid, an oxazoline derivative of PD, with potentially lower toxicities than prednisone or PD (8), and has been widely used as an immunosuppressant in the field of pediatric nephrology; nephrotic syndrome and renal transplantation (9), and in Duchenne dystrophy (10). Only one case of adult study has indicated that deflazacort might be a suitable substitute for PD in the treatment of autoimmune hepatitis (11). In clinical trials in Spain, deflazacort was administered to patients with type-1 autoimmnune hepatitis who were in remission on a stable dose of PD. Only clinical and biochemical remission were maintained during the follow-up period without histologic examination. In the present case, deflazacort was substituted for PD as a therapeutic drug in a child who was in remission on PD and UDCA, but significant PD-associated toxicities occurred. After switching to deflazacort, these toxicities improved rapidly, and the patient remained in clinical and biochemical remission. After 19 months on deflazacort, a follow-up liver biopsy showed near-normalization of auto-immune hepatitis. This is the first known clinical report to show that deflazacort is a suitable substitute for PD in the treatment of autoimmune hepatitis. Clinical and biochemical remission in this case were supported by documented histologic resolution.
A recent study showed the measurement of organ- and non-organ-specific auto-antibodies and IgG levels correlated with disease activity in autoimmune hepatitis (12). The patient in the present case remained ANA-positive with 1:160 titer, when on PD and UDCA, but became ANA negative at about the time of the follow-up liver biopsy performed after 19 months on deflazacort and UDCA. This may provide additional evidence that deflazacort is a possible substitute for PD in the treatment of autoimmune hepatitis. This case poses the possibility that deflazacort can be a possible substitute for prednisone in type-1 autoimmune hepatitis in children, and demonstrates the need for further study.
Figures and Tables
Fig. 1
The pre-treatment liver biopsy shows moderate-lobular inflammation and mild portal inflammation (H&E, ×100). The inset shows piecemeal necrosis and moderate fibrosis (H&E, ×400).
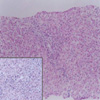
Fig. 2
Post-treatment liver biopsy shows no lobular activity, and no portal activity (H&E, ×100). The inset shows near-normal periportal inflammation and fibrosis in the portal area (H&E, ×200).

Fig. 3
Clinical course of the patient. The patient manifested fulminent hepatitis with ANA positivity and a normal IgG level. Initially, a conventional steroid (prednisolone) and ursodeoxycholic acid was tried. After the development of steroid toxicities, deflazacort (Calcort®) was substituted for prednisolone. The patient remained on clinical and biochemical remission, and ANA became negative. A follow-up liver biopsy was performed.
T.B, total bilirubin; UDCA, ursodeoxycholic acid; ANA, antinuclear antibody.

References
1. Alvarez F. Suchy FJ, Sokol RJ, Balistreri WF, editors. Autoimmune hepatitis. Liver disease in children. 2001. 2nd ed. Philadelphia Lippincott: Williams & Wilkins;429–441.
2. Gregorio GV, Portmann B, Reid F, Donaldson PT, Doherty DG, McCartney M, Mowat AP, Vergani D, Mieli-Vergani G. Autoimmune hepatitis in childhood: A 20-year experience. Hepatology. 1997. 25:541–547.

3. Alvarez F, Berg PA, Bianchi FB, Bianchi L, Burroughs AK, Cancado EL, Chapman RW, Cooksley WG, Czaja AJ, Desmet VJ, Donaldson PT, Eddleston AL, Fainboim L, Heathcote J, Homberg JC, Hoofnagle JH, Kakumu S, Krawitt EL, Mackay IR, MacSween RN, Maddrey WC, Manns MP, McFarlane IG, Meyer zum Buschenfelde KH, Mieli-Vergani G, Nakanuma Y, Nishioka M, Penner E, Porta G, Portmann BC, Reed WD, Rodes J, Schalm SW, Scheuer PJ, Schrumpf E, Seki T, Toda G, Tsuji T, Tygstrup N, Vergani D, Zeniya M. International autoimmune hepatitis group report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999. 31:929–938.

4. Vergani D, Mieli-Vergani G. Walker WA, Goulet O, Kleinman RE, Sherman PM, Shneider BL, Sanderson IR, editors. Autoimmune disease. Pediatric gastrointestinal disease. 2004. 4th ed. Hamilton: BC Decker;1208–1218.
5. Tage-Jensen U, Schlichting P, Thomsen HF, Hoybye G, Thomsen AC. Malignancies following long-term azathioprine treatment in chronic liver disease. A report from the Copenhagen study group for liver diseases. Liver. 1987. 7:81–83.
6. Nakamura K, Yoneda M, Yokohama S, Tamori K, Sato Y, Aso K, Aoshima M, Hasegawa T, Makino I. Efficacy of ursodeoxycholic acid in Japanese patients with type 1 autoimmune hepatitis. J Gastroenterol Hepatol. 1998. 13:490–495.

7. Czaja AJ, Carpenter HA, Lindor KD. Ursodeoxycholic acid as adjunctive therapy for problematic type 1 autoimmune hepatitis: a randomized placebo-controlled treatment trial. Hepatology. 1999. 30:1381–1386.

8. Markham A, Bryson HM. Deflazacort. A review of its pharmacological properties and therapeutic efficacy. Drugs. 1995. 50:317–333.
9. Ferraris JR, Pasqualini T, Legal S, Sorroche P, Galich AM, Pennisi P, Domene H, Jasper H. Effect of deflazacort versus methylprednisone on growth, body composition, lipid profile, and bone mass after renal transplantation. The deflazacort study group. Pediatr Nephrol. 2000. 14:682–688.
10. Campbell C, Jacob P. Deflazacort for the treatment of Duchenne dystrophy: a systemic review. BMC Neurol. 2003. 3:7.

11. Rebollo Bernardez J, Cifuentes Mimoso C, Pinar Moreno A, Caunedo Alvarez A, Salas Herrero E, Jimenez-Saenz M, Herrerias Gutierrez J. Deflazacort for long-term maintenance of remission in type 1 autoimmune hepatitis. Rev Esp Enferm Dig. 1999. 91:630–638.
12. Gregorio GV, McFarlane B, Bracken P, Vergani D, Mieli-Vergani G. Organ and non-organ specific autoantibody titers and IgG levels as markers of disease activity: a longitudinal study in childhood autoimmune liver disease. Autoimmunity. 2002. 35:515–519.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download