Abstract
We studied the prevalence, type and severity of vigabatrin (VGB)-attributed visual field defects (VFDs), and used these data to assess the associated risk factors in pediatric patients. Medical records were retrospectively reviewed for 67 pediatric patients who received VGB alone or in combination with other antiepileptic drugs, and who had undergone visual field examinations using a Humphrey visual field analyzer. Of the 67 patients, 15 had VGB-attributed VFDs: 13 had nasal arcuate type, 1 had nasal and temporal constricted type and 1 had nasal constricted type. In terms of severity, 7 patients had Grade I VGB-attributed VFDs, 5 had Grade II, 2 had Grade III, and 1 had Grade IV. Although there were no significant differences between the VFD and non-VFD groups with regards to all tested parameters, there were no cases of VGB-attributed VFDs in patients with total treatment durations <2 yr and cumulative doses <10 g/kg. In conclusion, the prevalence of VGB-attributed VFDs in VGB-treated pediatric epilepsy patients was 22%. The high frequency of VGB-attributed VFDs indicates that physicians should inform all patients of this risk prior to VGB treatment and perform periodic visual field examinations.
Vigabatrin (VGB) is an antiepileptic drug that irreversibly inhibits brain γ-aminobutyric acid (GABA) transaminase (1). VGB is used as first-line treatment for infantile spasms, especially those secondary to tuberous sclerosis, and as an adjunct therapy for medically resistant localization-related childhood epilepsies (2).
Following an initial report of 3 patients who experienced concentric visual field losses following VGB treatment (3), several additional studies showed visual field constriction during VGB therapy. Cross-sectional studies have estimated the prevalence of VGB-associated visual field defects (VFDs) as 20-50% in patients receiving VGB mono- or adjunct therapies. Various groups have found that longer treatment (4,5) and higher total doses (6-8) are associated with greater visual field losses in adults, while other studies dispute these correlations (9,10). A characteristic pattern of ocular dysfunction has been observed in VGB-treated patients, including peripheral visual field constriction primarily in the nasal area, which is rarely seen in other conditions (11-13).
Although these studies have shown evidence of VGB-associated VFD, VGB is highly effective and has a low occurrence of side effects or metabolic interactions. Thus, it is still commonly used in the clinic, especially for treatment of infantile spasms and tuberous sclerosis with intractable epilepsy. Most studies on VGB-associated VFD to date have been performed in adult patients, in part because it is difficult to estimate the frequency of this condition in pediatric patients, who are generally unable to cooperate in visual field testing. Only a few studies have been attempted in pediatric patients. We therefore sought to estimate the prevalence, type, severity, and risk factors of VGB-attributed VFDs in pediatric patients.
We retrospectively investigated the medical records of 67 pediatric epileptic patients who were treated with VGB at the Department of Pediatrics of the Asan Medical Center and had undergone ophthalmological examinations. For inclusion, each patient was required to have a diagnosis of epilepsy, no evidence of ophthalmologic disease upon initial examination, and a history of treatment with antiepileptic drugs, including VGB, during the observation period. Patients were excluded if they had poor compliance or non-concentric VFDs, which corresponded to brain organic lesions (e.g. intracranial hemorrhage).
The enrolled patients had been given full ophthalmologic examinations, including visual acuity, ophthalmoscopy, measurement of intraocular pressure, and visual field examination using program 30-2 of the Humphrey Field Analyzer. The severities of the VGB-attributed VFDs were scored as Grade I (minimal, 25-30°), Grade II (moderate, 20-30°), Grade III (moderate to severe, <20°), or Grade IV (severe, ring scotoma)(Fig. 1). Data were analyzed by Fisher's exact test and Student's t-test using SPSS, version 10.01.
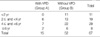
The patient population consisted of 67 VGB-treated patients, 41 males (61.2%) and 26 females (38.8%), with a mean age of 13 yr (range; 6 6/12 yr to 21 yr old). Of the 67 patients, 15 (22%) had VFDs, which we attributed to VGB, and 52 (78%) did not. Of the patients with VGB-attributed VFDs, 13 had nasal arcuate type, 1 had nasal and temporal constricted type, and 1 had nasal constricted type (Table 1). Seven patients had Grade I VGB-attributed VFDs, 5 had Grade II, 2 had Grade III, and 1 had Grade IV (Table 2). To identify potential risk factors for VGB-attributed VFDs, we compared the VFD and non-VFD patient groups with respect to medications and other clinical parameters. There were no significant differences between the VFD and non-VFD patients in terms of mean age at the beginning of treatment, total treatment duration, cumulative VGB dose, maximum VGB dose, sex distribution, structural abnormalities in the brain, or whether VGB was given alone or in conjunction with another drug (p>0.05 each) (Table 3). However, there were no cases of VGB-attributed VFDs in patients with total treatment durations <2 yr (Table 4 and cumulative doses <10 g/kg (Table 5).
Our results indicate that the prevalence of VFDs in VGB-treated children is 22%. This is consistent with recent reports of VFD prevalences ranging from 15 to 20% in western children (7,13-17), but is lower than the about 30% previously observed in VGB-treated children. This may be due to our patient population, which was limited to older patients capable of cooperating with ophthalmologic and visual field examinations. The exclusion of younger patients may have decreased the estimated prevalence of VGB-associated VFDs, because these younger patients, especially those with infantile spasms, require high dose, sustained treatment with VGB and might be more prone to VFDs. In addition, we used automated static perimetry to detect VGB-attributed VFDs, which may have influenced our results. The utilized 30-2 Humphrey Field Analyzer has the advantages of being generally available, investigator independent, easy to use, simple to standardize, and highly effective at detecting nasal field defects. However, because of its limited spatial context, the Humphrey Field Analyzermay miss mild to moderate visual field defects in the temporal fields. These are more reliably demonstrated by other techniques, such as kinetic (Goldmann) perimetry (10,18). However, VGB-associated VFDs typically present as concentric peripheral losses that are most severe nasally, with relatively milder temporal losses; these characteristics indicate that although some mild-to-moderate defects may be underestimated using this technique, the static Humphrey Field Analyzer should reliably detect VGB-attributed VFDs.
A final limitation in the present work is our inability to conclusively identify a causal link between VGB therapy and the observed VFDs; for this to be possible, we would have to enroll only patients who had completed VFD testing prior VGB therapy, which is rare. However, this is a limitation in most, if not all, retrospective studies on pediatric VBG-attributed VFDs. Here, we believe that the noted VFDs are VGB-attributed VFDs because they have the nasal-dominated pattern that is characteristic of VGB-attributed VFDs but is not seen in VFDs due to other causes.
Interestingly, our analysis did not reveal any correlations between the incidence of VGB-associated VFDs and the mean age at the beginning of treatment, total treatment duration, cumulative dose or maximum dose. However, we did note that no VGB-attributed VFDs were seen in patients with total treatment durations <2 yr and cumulative doses <10 g/kg. The latter trends are consistent with previous findings in adults, wherein longer treatment durations (5) and higher total doses of VGB (7) were associated with greater losses in visual fields. These possible associations are particularly important in pediatric patients, because high dose, sustained VGB treatment is commonly used to treat infantile spasms, especially those from tuberous sclerosis (19). If the treatment duration and cumulative dose of VGB are related to VFD, shorter treatments or lower doses should be investigated by linear regression analysis and prospective trials for their abilities to be therapeutically effective while minimizing the occurrence of VFDs. Another important finding was that the most common type of VGB-attributed VFD in our study population was the nasal arcuate type, and that severity Grades I and II were most frequent. These findings are consistent with previous reports that VGB-associated VFDs involve the nasal field (10), and indicate that automated perimetry is likely to be more reliable for identifying VGB-associated VFDs. However, automated perimetry tends not to lend itself to assessment of pediatric patients, suggesting the need for more reliable and cooperation-independent testing methods.
While VGB-attributed VFD was originally considered irreversible (20), more recent studies have shown that this condition can be reversed in adult (21-23) and pediatric (13,24,25) patients after discontinuation of VGB therapy. These reports suggested that patients can recover their retinal function despite apparently permanent damage to retinal cells. Although the mechanism by which VGB causes VFD is still not known, studies have suggested that VGB causes a general defect in the retinal network rather than damaging the outer retinal layer (26). Theoretically, such a defect could functionally recover, at least to some extent, in younger people whose neuronal systems still possess significant plasticity. In the future, it may be possible to perform follow-up visual field examinations on our study population, in an effort to examine reversibility in pediatric patients.
In sum, the results of the present study suggest that VFD occurs in VGB-treated children, but at a lower prevalence than that seen in adults (5,9-11,14,26-29). Our results also suggest that there is a relationship between VGB-attributed VFDs and the duration and total dose of VGB. Therefore, we recommend that the total dose and duration of VGB treatment should be reduced as much as possible, and that patients receiving VGB should be given visual field examinations prior to VGB treatment, and at regular intervals thereafter. Overall, the clinical decision to use VGB should be based on a risk-benefit analysis of each individual case.
Figures and Tables
Fig. 1
Four separate and increasingly severe cases of VBG-attributed field defects, as determined by automated static threshold perimetry using Humphrey Field Analyzer Program 30-2. (A) Grade I (minimal, 25-30°), (B) Grade II (moderate, 20-30°), (C) Grade III (moderate to severe, <20°), (D) Grade IV (severe, ring scotoma).

References
2. Hancock E, Osborne JP. Vigabatrin in the treatment of infantile spasms in tuberous sclerosis: literature review. J Child Neurol. 1999. 14:71–74.
3. Eke T, Talbot JF, Lawden MC. Severe persistent visual field constriction associated with vigabatrin. BMJ. 1997. 314:180–181.

4. Hardus P, Verduin WM, Postma G, Stilma JS, Berendschot TT, van Veelen CW. Concentric contraction of the visual field in patients with temporal lobe epilepsy and its association with the use of vigabatrin medication. Epilepsia. 2000. 41:581–587.

5. Hardus P, Verduin WM, Postma G, Stilma JS, Berendschot TT, van Veelen CW. Long term changes in the visual fields of patients with temporal lobe epilepsy using vigabatrin. Br J Ophthalmol. 2000. 84:788–790.
6. Manuchehri K, Goodman S, Siviter L, Nightingale S. A controlled study of vigabatrin and visual abnormalities. Br J Ophthalmol. 2000. 84:499–505.

7. Vanhatalo S, Nousiainen I, Eriksson K, Rantala H, Vainionpää L, Mustonen K, Äärimaa T, Alen R, Aine MR, Byring R, Hirvasniemi A, Nuutila A, Walden T, Ritanen-Mohammed UM, Karttunen-Lewandowski P, Pohjola LM, Kaksonen S, Jurvelin P, Granstromet LM. Visual field constriction in 91 Finnish children treated with vigabatrin. Epilepsia. 2000. 43:748–756.
8. Malmgren K, Ben-Menachen E, Frisén L. Vigabatrin visual toxicity: Evolution and dose dependence. Epilepsia. 2001. 42:609–615.

9. Kälviäinen R, Nousiainen I, Mäntyjärvi M, Nikoskelainen E, Partanen J, Partanen K, Riekkinen P. Vigabatrin, a GABAergic antiepileptic drug, causes concentric visual field defects. Neurology. 1999. 53:922–926.

10. Wild JM, Martinez C, Reinshagen G, Harding GF. Characteristics of a unique visual field defect attributed to vigabatrin. Epilepsia. 1999. 40:1784–1794.

11. Krauss GL, Johnson MA, Miller NR. Vigabatrin-associated retinal cone system dysfunction: electroretinogram and ophthalmologic findings. Neurology. 1998. 50:614–618.

12. Arndt CF, Derambure P, Defoort-Dhellemmes S, Hache JC. Outer retinal dysfunction in patients treated with vigabatrin. Neurology. 1999. 52:1201–1205.

13. Iannetti P, Spalice A, Perla FM, Conicella E, Raucci U, Bizzarri B. Visual field constriction in children with epilepsy on vigabatrin treatment. Pediatrics. 2000. 106:838–842.

14. Vanhatalo S, Pääkkönen L, Nousiainen I. Visual field constriction in children treated with vigabatrin. Neurology. 1999. 52:1713–1714.

15. Gross-Tsur V, Banin E, Shahar E, Shalev RS, Lahat E. Visual impairment in children with epilepsy treated with vigabatrin. Ann Neurol. 2000. 48:60–64.

16. Wohlrab G, Boltshauser E, Schmitt B, Schriever S, Landau K. Visual field constriction is not limited to children treated with vigabatrin. Neuropediatrics. 1999. 30:130–132.

17. Miller NR, Johnson MA, Paul SR, Girkin CA, Perry JD, Endres M, Krauss GL. Visual dysfunction receiving vigabatrin: Clinical and electrophysiologic findings. Neurology. 1999. 53:2082–2087.
18. Toggweiler S, Wieser HG. Concenteric visual filed restriction under vigabatrin therapy: extent depends on the duration of drug intake. Seizure. 2001. 10:420–423.
19. Appleton RE, Peters AC, Mumford JP, Shaw DE. Randomized, placebo-controlled study of vigabatrin as first-line treatment of infantile spasms. Epilepsia. 1999. 40:1627–1633.
20. Schmit T, Ruther K, Jokiel B, Pfeiffer S, Tiel-Wilck K, Schmitz B. Is visual field constriction in epilepsy patients treated with vigabatrin reversible? J Neurol. 2002. 249:1066–1071.
21. Johnson MA, Krauss GL, Miller NR, Medura M, Paul SR. Visual function loss from vigabatrin: effect of stopping the drug. Neurology. 2000. 55:40–45.

22. Krakow K, Polizzi G, Riordan-Eva P, Holder G, MacLeod WN, Fish DR. Recovery of visual constriction following discontinuation of vigabatrin. Seizure. 2000. 9:287–290.
23. Fledelius HC. Vigabatrin associated visual field constriction in a longitudinal series. Reversibility suggested after drug withdrawal. Acta Ophthalmol Scand. 2003. 81:41–46.
24. Versino M, Veggiotti P. Reversibility of vigabatrin-induced visualfield defect. Lancet. 1999. 354:486.

25. Giordano L, Valseriati D, Vignoli A, Morescalchi F, Gandolfo E. Another case of reversibility of visual-defect induced by vigabatrin monotherapy: is young age a favorable factor? Neurol Sci. 2000. 21:185–186.
26. Nousiainen I, Kalviainen R, Mantyjarvi M. Contrast and glare sensitivity in epilepsy patients treated with vigabatrin or carbamazepine monotherapy compared with healthy volunteers. Br J Ophthalmol. 2000. 84:622–625.

27. Lawden MC, Eke T, Degg C, Harding GF, Wild JM. Visual field defects associated with vigabatrin therapy. J Neurol Neurosurg Psychiatry. 1999. 67:716–722.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download