Abstract
We reviewed clinical manifestation of 12 patients from three Korean families. They showed mild to moderate bone fragility, and suggested an autosomal dominant inheritance pattern. Significant intrafamilial phenotype variability was obvious. Clinical, radiological, and histopathologic characteristics that distinguished this subtype from others include ossification of interosseous membrane of the forearm with radial head dislocation, hyperplastic callus formation, no evidence of type I collagenopathy and an abnormal histopathologic pattern. Severity of the interosseous membrane ossification was correlated with increasing age (p<0.01) and the radial head dislocation was thought to be a developmental problem rather than a congenital problem. Four children who had bisphosphonate treatment showed improved bone mineral density, radiological changes, and biochemical responses. Osteogenesis imperfecta type V was a distinctive subtype of osteogenesis imperfecta, which caused mild to moderate disability clinically.
Osteogenesis imperfecta (OI) is a genetic disorder characterized by bone fragility, deformity of the spine and long bones, and other clinical symptoms such as short stature, blue sclera, and dentinogenesis imperfecta. The Sillence classification into 4 types (1) has been widely used, but severity of phenotypes varies extensively in each types, especially in type IV (2). Subgroups of type IV patients with characteristic phenotypes were proposed and subsequently classified as types V, VI, and VII (3-5). OI type V was reported to have hyperplastic callus, ossification of interosseous membrane of the forearm, radial head dislocation, abnormal histopathologic pattern, and absence of mutation in COL1A1 or COL1A2 genes (3). It has been reported to constitute 4 to 5% of OI patients seen in hospitals (6). However, to the best of our knowledge, no report has described clinical and radiological manifestation of OI type V patients in the Asian population.
We reviewed twelve Korean patients with OI type V to describe their clinical and radiological manifestations.
Among 122 osteogenesis imperfecta patients who visited our hospital over a 6 yr period, we identified five patients showing typical features of OI type V (Cases 1, 2, 3, 11, 12). One patient was a sporadic case, and two other patients were father and daughter. The remaining two patients were from a big family with OI type V inherited through four generations (Fig. 1). Seven more patients from this family were diagnosed as OI type V. Thus, twelve patients from three Korean families were included in this study. They were seven men and five women. Age at the time of diagnosis ranged from 8 months to 75 yr. Four patients were skeletally immature and eight were mature.
Medical histories including previous fractures were taken from all patients. Thorough physical examination was done, including deformity of the spine and extremities, range of motion of the joints, dental status, and color of the sclera. Standing height was measured and transformed into Z-score according to age and sex using standard growth chart for children (7) and data from National Anthropometric Survey of Korea for adults (8).
Skeletal series of the plain radiographs was reviewed in the five index cases. For the remaining seven cases, plain radiographs of the forearm were evaluated. Ossification of the interosseous membrane of the forearm on anteroposterior radiograph was classified into three grades-Grade I: incomplete ossification of the interosseous membrane with clear space more than 2 mm; Grade II: incomplete ossification of the interossous membrane with clear space less than 2 mm; and Grade III: definite bony connection between both forearm bones via interosseous membrane (Fig. 2).
Four skeletally immature patients were treated with bisphosphonates, either cyclic intravenous pamidronate or oral alendronate according to the protocols previously reported (9,10). Biochemical response was monitored by measuring urinary excretion of creatinine, calcium, and cross-linked N-telopeptides of type I collagen (NTx). Bone mineral density was measured at the lumbar spine (L2-4) and the femur neck using a dual energy radiography absorptiometry (Expert-x1, Lunar, Madison, WI, U.S.A.). It was transformed to age-matched Z score using the children's references provided by the manufacturer.
Surgical specimen of the osseous tissue underwent histopathologic study in two cases. The undecalcified bone section was stained with toluidine blue, and evaluated under polarized light microscope.
Statistical analysis was performed with use of Spearman's nonparametric correlation test. p-value <0.05 was considered statistically significant.
Pertinent data of the patients are summarized in Table 1. Pedigrees of two families concurred with autosomal dominant inheritance pattern. All the patients were community ambulators. Only one patient with scoliosis and both hip ankylosis needed a cane for commuting (Case 2).
Number of fractures in lifetime ranged from 1 to 15. Fracture frequency ranged from 0.02 to 4.5 fractures/year (average, 0.98 fracture/year). The age and sex-matched Z-score for standing height averaged-0.35 (range, -2.53 to 1.71). All the patients had normal sclerae and teeth in color and shape. The range of forearm rotation was limited in all patients and averaged 85 degrees. Flexion of the elbow joint was limited to 110 degrees or less in seven elbows of four patients.
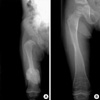
The radial head dislocations were present bilaterally in all patients except three children under 5 yr of age. However, in one of them, both radial heads dislocated during follow-up before 2 yr of age (Fig. 3). Among 10 fractures treated by these authors, only one case of the femur shaft fracture showed hyperplastic callus formation, which eventually remodeled (Fig. 4).
All the patients showed ossification of the interosseous membrane of the forearm. They were grade I in twelve forearms, grade II in 10, and grade III in 2. Severity of ossification was significantly correlated with increasing age (p<0.01), but not with range of the forearm rotation (p=0.566).
One of the index patients (Case 2) showed ossification of the interosseous membrane of the lower leg as well. He had also suffered from extraarticular bony ankylosis of both hip joints which developed gradually since 15 yr-old (Fig. 5A, B). The remaining eleven patients did not show any limitation of joint motion other than the elbow and forearm.
Four patients had scoliosis larger than 20 degrees. One underwent surgical stabilization (Case 9), but another patient with scoliosis of 59 degrees with marked trunk shift (Case 2, Fig. 5C) refused surgical stabilization. The remaining two patients had scoliosis of less than 40 degrees.
Four skeletally immature patients who had received bisphosphonate treatment showed biochemical responses such as decrease of the urinary excretion of calcium and NTx. Additional radio-opacity accumulated at the juxtaphyseal metaphysis of the long bones on top of the pre-existing metaphyseal white bands (Fig. 4), as previously described (9,10). Bone densitometry follow-up was available in two patients. Case 3 had oral alendronate from age 10 yr for 2.5 yr, whose bone mineral density of the lumbar spine (L2-4) improved from 0.505 g/cm2 (Z= -2.82) to 1.018 g/cm2 (Z=0.9). In another patient (Case 11), who received intravenous pamidronate of 10 mg/kg through seven cycles for one year, the bone mineral density of the lumbar spine improved from 0.289 g/cm2 to 0.435 g/cm2, but Z-score could not be calculated as the reference values of this age group was not available.
Three out of twelve patients underwent orthopedic surgical procedures. One young adult (case 9) underwent spinal fusion for scoliosis. Case 3 complained of bilateral radial head dislocations and cubitus varus deformities at the proximal forearm. Right radial head excision was performed along with ulnar corrective osteotomy at age 10+9 yr, and left radial head excision at age 12+11 yr, mainly for cosmetic purpose. There was neither improvement of range of the elbow and forearm motion nor any detrimental effect at the wrist after these surgical procedures. The four-year-old boy (Case 11) underwent an osteotomy at the radius diaphysis to correct the volar apex angulation of 41°. The osteotomy healed uneventfully, however he lost range of the forearm pronation from 30° to 10° although the interosseous membrane ossification did not aggravate and the radial head was still in situ.
Histopathologic examination of the surgical specimen from these two patients revealed irregularly arranged lamellae with mesh-like appearance (Fig. 6).
Osteogenesis imperfecta is one of the most common inherited disorders of connective tissue (2). Many classification systems have been proposed for this disease, which reflects difficulties in categorizing this disease entity due to its diverse phenotypes, varying severity, and poor correlation between genotype and phenotype (1,2). A series of distinct subtypes of OI has been proposed (3-5), which would have been classified as type IV according to the Sillence classification. Of these, OI type V is characterized by bone fragility, ossification of the interosseous membrane of the forearm, radial head dislocation, hyperplastic callus formation, heredity suggesting an autosomal dominant pattern and no evidence of mutation in type I collagen genes (3).
From the experience of these cases we agree that OI type V is a distinct disease entity, which could be differentiated from the other types of OI by clinical and radiological examinations. Histologic findings, if available, may be confirmatory, and a negative result of type I collagen mutation analysis might be helpful for confirming the diagnosis, although neither specific nor sensitive.
Previous report on OI type V did not describe clinical manifestation of the affected family members other than the index cases (3). Index cases of the current study were the most severely affected cases. One patient (Case 2) required walking aid due to both hip joint ankylosis, but he seemed to be the most seriously affected, showing multiple ectopic ossifications besides the forearm interosseous membrane (Fig. 5). All the other patients did not have any serious functional disability interfering with daily life. Therefore, OI type V may be considered a relatively mild type of OI with varying severity.
Ossification of interosseous membrane of the forearm seems to be a pathognomonic feature of OI type V. All patients included in this study showed interosseous membrane ossifications, which were symmetrical and advancing with age. But interestingly there was no significant correlation between severity of ossification and range of the forearm rotation except for Grade III which resulted in complete ankylosis. Moreover, either radial head excision or deformity correction of the forearm bones could not improve the forearm rotation. These findings suggest that an unknown pathology within the interosseous membrane or its surrounding soft tissue, rather than ossification itself, attribute to limitation of the forearm rotation, which needs to be further investigated.
Radial head dislocation is one of the most characteristic phenotypes of this disease. OI type V should be included in the differential diagnosis of radial head dislocation in children in this context. Fassier et al. (11) reported that the incidence and direction of radial head dislocation in OI type V differ significantly from that of other types. In our series, all the patients over 10 yr-old were found to have dislocated radial heads, whereas the three affected children had radial head in situ when firstly presented under age 5 yr, suggesting that radial head dislocation in OI type V was developmental rather than congenital. Pathomechanism of the radial head dislocation has not been fully elucidated. Ossification of the interosseous membrane and angular deformity of the forearm bones seem to contribute to its development.
Radial head excision can be considered if symptomatic or for cosmetic purpose, although the timing of operation is controversial. The authors believe that a dislocated radial head in OI type V may be safely excised before skeletal maturity if clinically indicated as in the case of congenital radial head dislocation (12).
Bisphosphonate treatment for osteogenesis imperfecta patients has been well established as a standard treatment (9,10,13). Recently, researchers have reported that intravenous pamidronate therapy has similar effect in OI type V as in the other OI types (14,15). We treated 4 children in this series with either oral alendronate or cyclic intravenous pamidronate, and all showed biochemical and radiological responses as expected. However, in patients with relatively mild symptoms, its clinical benefit should be weighed against its potential complications, as in other types of OI.
The present study is the first report of OI type V in Asian population. Affected family members shared some phenotypes with other types of OI, although clinical, radiological, and histological characteristics distinguished this disease from other OI types.
Figures and Tables
 | Fig. 1Pedigrees of osteogenesis imperfecta type V families. (A) The family of cases 2 and 3. (B) The family of cases 4-12. |
 | Fig. 2Ossification of interosseous membrane of the forearm. (A) Grade I; (B) Grade II; and (C) Grade III. |
 | Fig. 3Development of the radial head dislocation. (A) The radial head is in situ at age 9 months. (B) Radiograph at age 28 months shows dislocated radial head (Case 1). |
 | Fig. 4Hypertrophic callus formation six weeks after femoral shaft fracture at age 9 month (A). A radiograph taken 1.5 yr later shows remodeling of the callus (B). Note the multiple white bands parallel to the physis formed by cyclic intravenous pamidronate and the juxtaphyseal metaphyseal white area which is one of the radiologic manifestations of OI type V (Case 1). |
 | Fig. 5Radiographic abnormalities other than the elbow and forearm. Heterotopic ossification around the hip joints and femur (A); ossification of the interosseous membrane of the lower leg (B); and right thoracic scoliosis with decompensated trunk-shift (C) (Case 2). |
 | Fig. 6Polarized light microscope histopathologic finding of a bone specimen from Case 3. Note the irregular, mesh-like lamellation pattern (Toluidine blue, ×200). |
References
1. Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet. 1979. 16:101–116.

2. Shapiro F. Osteogenesis imperfecta in pediatric orthopedic deformities. 2001. Boston: Academic Press;847–860.
3. Glorieux FH, Rauch F, Plotokin H, Ward L, Travers R, Roughley P, Lalic L, Glorieux DF, Fassier F, Bishop NJ. Type V osteogenesis imperfecta: a new form of brittle bone disease. J Bone Miner Res. 2000. 15:1650–1658.

4. Glorieux FH, Ward LM, Rauch F, Lalic L, Roughley P, Travers R. Osteogenesis imperfecta type VI: a form of brittle bone disease with a mineralization defect. J Bone Miner Res. 2002. 17:30–38.

5. Ward LM, Rauch F, Travers R, Chabot G, Azouz EM, Lalic L, Roughley PJ, Glorieux FH. Osteogenesis imperfecta type VII: an autosomal recessive form of brittle bone disease. Bone. 2002. 31:12–18.

7. References for Korean children's physical development. 1998. Updated Oct. 9, 1998. Retrieved 24 January 2006. Seoul, Korea: Korean Pediatric Society;http://www.pediatrics.or.kr/default.asp
.
8. National Anthropometric Survey of Korea. 1997. Retrieved January 24, 2006. Seoul, Korea: Korean Agency for Technology and Standards;http://www.standard.go.kr
.
9. Cho TJ, Choi IH, Chung CY, Yoo WJ, Park MS, Park YK. Efficacy of oral alendronate in children with osteogenesis imperfecta. J Pediatr Orthop. 2005. 25:607–612.

10. Cho TJ, Park MS, Choi IH, Chung CY, Yoo WJ. Efficacy of cyclic intravenous pamidronate therapy for children with osteogenesis imperfecta. J Korean Orhtop Assoc. 2003. 38:741–747.

11. Fassier AM, Rauch F, Aarabi M, Janelle C, Fassier F. Radial head dislocation in osteogenesis imperfecta. Proceedings of the 9th International Conference on Osteogenesis Imperfecta. 2005. 95.
12. Campbell CC, Waters PM, Emans JB. Excision of the radial head for congenital dislocation. J Bone Joint Surg Am. 1992. 74:726–733.

13. Glorieux FH, Bishop NJ, Plotkin H, Chabot G, Lanoue G, Travers R. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med. 1998. 339:947–952.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download