Abstract
Local epidemiologic data on the etiologies of patients hospitalized with community-acquired pneumonia (CAP) is needed to develop guidelines for clinical practice. This study was conducted prospectively to determine the proportion of atypical bacterial pathogens in adults patients hospitalized with CAP in Korea between October 2001 and December 2002. Microbiological diagnosis was determined by serology for antibodies to Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila. Nucleic acid of M. pneumoniae and C. pneumoniae in respiratory samples and Legionella antigen in urine samples were detected. The study population consisted of 126 patients (71 males, 55 females), averaging 54.6 yr (SD±17.8), whose paired sera were available. An etiologic diagnosis for atypical pathogens was made in 18 patients (14.3%): C. pneumoniae 9 (7.1%), M. pneumoniae 8 (6.3%), and L. pneumophila 3 patients (2.4%). Streptococcus preumoniae and other typical pathogens were isolated from 36 patients (28.6%). Of 126 patients, 16 (12.7%) were admitted to intensive care unit and atypical pathogens were identified in 5 patients (31.3%). Initial clinical features of patients with pneumonia due to atypical, typical or undetermined pathogens were indistinguishable. We conclude that atypical pathogens should be seriously considered in hospitalized patients with CAP, when initiating empiric treatment in Korea.
Despite recent advances in diagnosis and treatment, community-acquired pneumonia (CAP) has been recognized as a common and potentially lethal condition, especially in older adults and those with co-morbid diseases (1). Current guidelines for the management of adult CAP recommend initial empirical antimicrobial treatment (2-4). This approach is based on microbial patterns derived from several large prospective epidemiological series in different geographic areas.
The etiology of CAP depends on the geographic area, the study population, and the utilized microbiological laboratory tests (2). In most studies, Streptococcus pneumoniae is the most common etiology in adult patients with CAP (1-6). However, the etiology remains undetermined in 40-60% of cases (2, 3). A major factor contributing to the unknown etiology of CAP is the difficulty in identifying atypical pathogens: Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella species. Diagnostic testing for these pathogens is not routinely performed since culture is difficult, time-consuming, and requires significant expertise. Serological diagnosis based on high acute antibody titers is quick but inaccurate, whereas diagnosis using the paired serology approach is more accurate but requires >2 week to perform. However, the importance of the atypical pathogens is highlighted by the increasing frequency of atypical organisms recognized in recent years with the development of more sensitive diagnostic techniques (5,7) and consideration of a macrolide in proper empirical antimicrobial therapy (3,8).
In Korea, very limited number of studies have been undertaken to identify atypical pathogens as a cause of CAP (9-11). In this study, we performed a prospective study to characterize atypical pathogens as a cause of CAP among adults patients admitted to 5 teaching hospitals over a period of one year by using diagnostic tests for nucleic acid, antigen and antibody detection of M. pneumoniae, C. pneumoniae, and L. pneumophila.
This prospective study is the result of Korean subgroup analysis of ASIA-CAP study which was performed in 8 countries from October 2001 to December 2002. This study was conducted in 5 teaching hospitals located in Seoul and Kyungi province, Korea between October 2001 and December 2002, after prior approval from each Institutional Review Board. Written informed consent was obtained from all patients or their legal representatives before study enrolment. The study was carried out in compliance with Good Clinical Practice, including International Conference on Harmonization Guidelines and the Declaration of Helsinki.
The study population consisted of adult patients (≥16 yr) hospitalized with CAP. All patients had clinical features and radiological findings compatible to CAP. Inclusion criteria were new infiltrates on chest radiography or consolidation that could not be attributed to some other etiology and 3 or more of the following signs and symptoms: cough, acute changes in the quality of sputum (<10 epithelial cells and >25 polymorphonuclear leukocytes per low-power field in microscopy), documented fever (>38℃) or hypothermia (<36.1℃) within the preceding 24 hr, rales, leukocytosis (>10×109/L or >15% bands), malaise, myalgia or gastrointestinal symptoms. All eligible patients were required to undergo serological tests on paired acute- and convalescent-phase sera, as well as tests for Legionella antigen in urine and polymerase chain reaction (PCR) on respiratory samples collected at baseline.
Patients with evidence of tuberculosis, nosocomial pneumonia, lung cancer, aspiration pneumonia, or bronchiectasis were excluded from the study. Subjects who were HIV positive or who had been hospitalized within 2 weeks prior to study enrolment were also excluded.
Conventional cultures of clinical samples obtained from patients with CAP were performed at each hospital and additional samples were sent to the central laboratory of Korea University Hospital for microbiological tests for atypical pathogens. For the purpose of serological testing, blood samples (5-8 mL) were collected aseptically and stored at -20℃ until convalescent sera were obtained after 2-8 weeks to be tested simultaneously. Sputum, nasopharyngeal aspirates, bronchoalveolar lavage, and samples of pleural fluid suitable for PCR analysis were stored in PCR buffer in 2 mL vials at -20℃ before testing. Urine samples were collected in sterile containers and stored at -20℃ until testing.
Specific antibodies (IgG and IgM) to M. pneumoniae were antibodies (IgG and IgM) to M. pneumoniae were measured using a particle agglutination test (SERODIA MYCO II, Fujirebrio Inc, Tokyo, Japan). A modified microimmunofluorescence (MIF) test (Focus Diagnostics Inc, Cypress, CA, U.S.A.) using purified elementary bodies diluted in egg yolk sac was used to measure specific IgG antibodies to C. pneumoniae, and C. psittaci. Legionella antibodies were detected by an indirect immunofluorescence antibody test (MarDx Diagnostics Inc, Carlsbad, CA, U.S.A.) for IgG antibodies to L. pneumophila serogroup 1 through 7.
PCR assays for the detection of M. pneumoniae and C. pneumoniae were performed as previously described with primers targeting the p1 adhesin gene of M. pneumoniae (12) and the 16S rRNA gene of C. pneumoniae (13). The presence of a PCR product of 463 bp or 209 bp on gel electrophoresis was considered indicative of infection with C. pneumoniae or M. pneumoniae, respectively.
For the qualitative detection of L. pneumophila serogroup 1 soluble antigen in urine, specimens were tested by a microtiter enzyme-linked immunosorbent assay (Biotest Legionella Urine Antigen EIA; Biotest AG, Dreieich, Germany) according to the manufacturer's recommendation.
The following criteria were used to classify a diagnosis as definitive: 1) a four-fold or greater rise in antibody titers for M. pneumoniae, C. pneumoniae, or L. pneumophila between acute- and convalescence-phase sera; and 2) detection of L. pneumophila antigen in urine. A probable etiologic diagnosis was based on the detection of mycoplasmal or chlamydial DNA in respiratory secretions.
A total of 202 patients hospitalized with a diagnosis of CAP were enrolled in this study. Paired sera were obtained from 126 patients and provided the basis for estimating the rates of infection caused by the three atypical respiratory pathogens. Failure to obtain paired serum samples on 76 patients was mainly due to follow-up loss (59 patients). Other reasons were failure to meet eligibility criteria (7 patients), tuberculosis (4 patients), and death (6 patients).
Table 1 summarizes the demographic data and clinical features at baseline of the 126 patients analyzed. Seventy-one patients were male and 55 were female. Forty-six patients (36.5%) were 65 yr or older. The mean age of the patients was 54.6 yr (range, 16 to 86 yr) (SD, ±17.8); males were slightly older than females. Forty-five patients (35.7%) had at least one underlying disease with diabetes mellitus being the most common (13.5%).
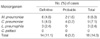
Etiologic diagnosis was achieved in 50 (39.7%) cases, and remained unknown in 76 cases. Atypical pathogens were identified in 18 patients (14.3%); 14 (11.1% of the total) diagnoses were definitive. The most common pathogen was C. pneumoniae (7.1%), followed by M. pneumoniae (6.3%), and L. pneumophila (2.4%) (Table 2). C. psittaci pneumonia was not found. In 9 cases with C. pneumoniae, 5 cases were diagnosed using serologic criteria with a four-fold or greater rise in antibody titer and 4 cases by positive PCR in sputum samples. In 8 cases with M. pneumoniae, 5 cases were diagnosed by the serologic criteria, one case by both serology and PCR assay in sputum samples, and 2 cases by PCR assay alone. Three patients with L. pneumophila pneumonia were diagnosed by the serologic criteria. No cases were positive for urinary antigen to L. pneumophila serogroup 1.
Routine bacterial cultures of sputum and blood were obtained in 126 patients; 39 pathogens were isolated from 36 patients (28.6%). S. pneumoniae was isolated from 17 (13.5%) cases. Other microorganisms isolated were Klebsiella pneumoniae (4), Pseudomonas spp. (4), Acinetobacter spp. (4), Streptococcus spp. (4), Escherichia coli (2), Enterobacter spp. (2), Haemophilus influenzae (1), and Staphylococcus aureus (1). Two or more pathogens were identified in 7 patients: a combination of a typical pathogen plus an atypical pathogen (4 cases) and a combination of two typical pathogens (3 cases).
Underlying diseases, symptoms, signs, and laboratory/radiology parameters of were compared among patients' groups with atypical, typical, or unknown pathogens are shown in Table 3. Cases with dual typical-atypical infections were excluded from the analysis. Clinical features and laboratory parameters did not differ significantly among the three groups. In addition, no differences were observed with respect to atypical etiology between two age groups: ≥65 yr and <65 yr. In 46 cases of ≥65 yr, atypical pathogens were identified in 7 (15.2%) cases: C. pneumoniae 4 (8.7%), M. pneumoniae 2 (4.3%) and L. pneumophila 2 (4.3%) cases. In 80 cases of <65 yr, atypical pathogens were identified in 11 (13.8%) cases: M. pneumoniae 6 (7.5%), C. pneumoniae 5 (6.3%), and L. pneumophila 1 (1.3%) case. C. pneumoniae was not detected in patients <40 yr. All L. pneumophila cases were detected in patients >60 yr. C. pneumoniae and L. pneumophila were more frequently found in patients with underlying diseases than those without underlying diseases: 8.9% vs. 6.2% and 4.4% vs. 1.2%, respectively. However, it was not statistically significant (p>0.05). M. pneumoniae was more frequently identified in patients without underlying diseases (8.6% vs. 2.2%, p>0.05).
Five cases (31.3%) out of 16 patients requiring admission to the ICU had pneumonia caused by atypical pathogens: C. pneumoniae (3 cases) L. pneumophila (1 case) and M. pneumoniae (1 case). All cases were diagnosed by the definitive criteria. There were no statistical differences with respect to atypical etiology between patients admitted the ICU and general ward (p>0.05).
In this study, we analyzed the atypical etiology of CAP in adult patients treated in hospital, based on the precise criteria of etiologic classification and the use of several diagnostic procedures that included serologic tests on paired sera, detection of bacterial antigen in urine, and detection of nucleic acids in sputum. Cases of atypical pneumonia have increasingly been reported, particularly in studies that have applied sensitive diagnostic methods (5,7,14-17). The proportion of cases of atypical pneumonia in other pneumonia studies has varied from 8% to 63% (18-21). The proportion of atypical pathogens (14.3%) found in our study was comparable to that reported previously in other studies on CAP in Korea (18.5%)(10).
C. pneumoniae is a frequent cause of CAP in patients treated in hospital, with rates ranging from 3.4 to 43% (20,21), and is also associated with severe CAP (2,14,22). In our study, C. pneumoniae was the etiology for 6.3% of CAP, and was responsible for 18.8% of severe pneumonia requiring admission to the ICU, that was slightly higher than that from other studies (22,23). All three cases of severe CAP with C. pneumonia met the criteria of definitive diagnosis; one patient had chronic lung disease and 2 patients were previously healthy. Of the 2 previously healthy patients, one patient had dual infection with C. pneumoniae and a typical pathogen. Among patients with C. pneumoniae pneumonia, underlying illness was not present in 56.6%, and dual infection did not occur in 66.7%. Therefore, we suggest that C. pneumoniae could be the sole cause of CAP requiring hospitalization.
The incidence of M. pneumoniae in hospitalized CAP patients varies from 0.8 to 29.2% according to the study population (21). In this study, M. pneumoniae was identified in 7.1% of patients with CAP, which was similar to the results from previous Korean studies (10). Although M. pneumoniae pneumonia is more frequent among children and young adults (3), our results shows no age predilection, suggesting that it can occur in all age groups.
The incidence of Legionella as a cause of sporadic CAP varies from 0.6 to 12.2% among cases requiring hospitalization, depending on the geographic area and the diagnostic technique used (21). In this study, L. pneumophila was identified in 2.4% of patients with CAP, which was similar to the result from a previous Korean study (9). In other Korean studies, no cases of Legionella pneumonia were found (10). In our study, in addition to the 3 definitive cases with Legionella pneumonia, 15 (11.9%) cases showed persistently high antibody titers (≥1:256) in both acute and convalescent serum samples. These data suggest that L. pneumophila might be the potential etiology of CAP in Korea similar to western countries. There were no cases with positive urinary antigen test, even when serology for L. pneumophila was positive. Although previous studies reported high sensitivity of the urinary antigen assay for L. pneumophila serogroup 1, it has some limitations. The differences in sensitivities were attributed initially to differences in the proportion of clinical material from pneumonia patients with infection caused by L. pneumophila serogroup 1 versus infection caused by other serogroups (24). Moreover, variation was attributed to the differences in clinical severity of the diseases. While 40-53% of the urinary antigen tests were positive in patients with mild Legionnaires' disease, 88-100% of the tests were positive in patients with severe Legionnaires' disease. Different urinary antigen assays have been reported with different sensitivities for detecting other serogroups which ranged from 14 to 69% (25-27). Although culture for Legionella was not performed in this study and thus identification of L. pneumophila serogroups was not possible, three definitive cases with Legionella pneumonia could be postulated to have been due to non-L. pneumophila serogroup 1.
C. psittaci was not identified as a cause of CAP in this study. Up until now, there have been no reports on C. psittaci pneumonia in Korea (10). We suggest that C. psittaci might be a rare cause of CAP in adult population in Korea.
As reported in recent study (28), PCR assay seems to be less sensitive than serological testing for diagnosing C. pneumoniae and M. pneumoniae. In addition, current problems with PCR techniques include great variability due to differences in sample collection and preparation methods, and amplification procedures; there are no U.S. Food and Drug Administration (FDA)-cleared reagents for PCR for detecting M. pneumoniae and C. pneumoniae (3,16). Thus rapid diagnosis for these pathogens still remains to be solved in the clinical field.
In present study, 126 out of 202 patients enrolled were analyzed for atypical pathogen identification. Fifty-nine patients were follow-up loss and not included for analysis because second serum samples were missing. Thus, it is possible that atypical pathogens were underestimated. In other studies, however, the rates of paired serum sampling was much lower rates of 31-44% than 62% in this study (7,10) and it helped increase the reliability of the data analyzed. It was not possible to determine the impact of atypical pathogens on mortality because a second serum was not available for those six deceased. Some of patients who died during the course of pneumonia may also have aggravation of comorbid illness. As our study included only hospitalized patients, further study is needed to determine role of atypical pathogens in patients who do not require hospital admission and could have been safely managed in their home.
Our study verified again that clinical presentation was not useful in differentiating typical and atypical pathogens (29,30). This study concluded that frequency of the atypical pathogens among patients hospitalized with CAP does not differ remarkably between Korea and western countries. Atypical pathogens should be taken into account when making guidelines of empirical antibiotic therapy for CAP in Korea.
Figures and Tables
Table 1
Demographic and clinical characteristics for the 126 hospitalized adult patients with community-acquired pneumonia

References
2. Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, Dean N, File T, Fine MJ, Gross PA, Martinez F, Marrie TJ, Plouffe JF, Ramirez J, Sarosi GA, Torres A, Wilson R, Yu VL. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001. 163:1730–1754.
3. Bartlett JG, Dowell SF, Mandell LA, File TM Jr, Musher DM, Fine MJ. Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis. 2000. 31:347–382.

4. Mandell LA, Bartlett JG, Dowell SF, File TM Jr, Musher DM, Whitney C. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis. 2003. 37:1405–1433.

5. Ruiz-Gonzalez A, Falguera M, Nogues A, Rubio-Caballero M. Is Streptococcus pneumoniae the leading cause of pneumonia of unknown etiology? A microbiologic study of lung aspirates in consecutive patients with community-acquired pneumonia. Am J Med. 1999. 106:385–390.
6. Mandell LA. Epidemiology and etiology of community-acquired pneumonia. Infect Dis Clin North Am. 2004. 18:761–776.

7. Marston BJ, Plouffe JF, File TM Jr, Hackman BA, Salstrom SJ, Lipman HB, Kolczak MS, Breiman RF. The Community-Based Pneumonia Incidence Study Group. Incidence of community-acquired pneumonia requiring hospitalization. Results of a population-based active surveillance Study in Ohio. Arch Intern Med. 1997. 157:1709–1718.
8. Plouffe JF. Importance of atypical pathogens of community-acquired pneumonia. Clin Infect Dis. 2000. 31:Suppl 2. 35–39.

9. Kim MJ, Cheong HJ, Sohn JW, Shim HS, Park DW, Park SC, Woo JH, Kang JM, Kim YK, Shin WS, Kim YR, Lee HJ, Kim JH. A prospective multicenter study of the etiological analysis in adults with community-acquired pneumonia: Legionella, Leptospira, Hantaan virus and Orientia tsutsugamushi. Korean J Infect Dis. 2001. 33:24–31.
10. Lee SJ, Lee MG, Jeon MJ, Jung KS, Lee HK, Kishimoto T. Atypical pathogens in adult patients admitted with community-acquired pneumonia in Korea. Jpn J Infect Dis. 2002. 55:157–159.
11. Joo CH, Yoon HJ, Nam JH, Cho YG, Woo JH, Kang JM, Shin WS, Kim YR, Kim MJ, Chung HJ, Lee HJ, Kim YK. A prospective multicenter study on the etiological analysis of community-acquired pneumonia in adult patients in Korea: detection of Mycoplasma pneumoniae and Chlamydia pneumoniae. Korean J Infect Dis. 2001. 33:15–24.
12. Ieven M, Ursi D, Van Bever H, Quint W, Niesters HG, Goossens H. Detection of Mycoplasma pneumoniae by two polymerase chain reactions and role of M. pneumoniae in acute respiratory tract infections in pediatric patients. J Infect Dis. 1996. 173:1445–1452.

13. Gaydos CA, Quinn TC, Eiden JJ. Identification of Chlamydia pneumoniae by DNA amplification of the 16S rRNA gene. J Clin Microbiol. 1992. 30:796–800.

14. File TM Jr, Plouffe JF Jr, Breiman RF, Skelton SK. Clinical characteristics of Chlamydia pneumoniae infection as the sole cause of community-acquired pneumonia. Clin Infect Dis. 1999. 29:426–428.

15. Sopena N, Sabria M, Pedro-Botet ML, Manterola JM, Matas L, Dominguez J, Modol JM, Tudela P, Ausina V, Foz M. Prospective study of community-acquired pneumonia of bacterial etiology in adults. Eur J Clin Microbiol Infect Dis. 1999. 18:852–858.

17. Gutierrez F, Masia M, Rodriguez JC, Mirete C, Soldan B, Padilla S, Hernandez I, Royo G, Martin-Hidalgo A. Community-acquired pneumonia of mixed etiology: prevalence, clinical characteristics, and outcome. Eur J Clin Microbiol Infect Dis. 2005. 24:377–383.

18. Mundy LM, Auwaerter PG, Oldach D, Warner ML, Burton A, Vance E, Gaydos CA, Joseph JM, Gopalan R, Moore RD. Community-acquired pneumonia: impact of immune status. Am J Respir Crit Care Med. 1995. 152(4 Pt 1):1309–1315.

19. Lieberman D, Schlaeffer F, Boldur I, Lieberman D, Horowitz S, Friedman MG, Leiononen M, Horovitz O, Manor E, Porath A. Multiple pathogens in adult patients admitted with community-acquired pneumonia: a one year prospective study of 346 consecutive patients. Thorax. 1996. 51:179–184.

20. Marrie TJ. Community-acquired pneumonia: epidemiology, etiology, treatment. Infect Dis Clin North Am. 1998. 12:723–740.

21. Gupta SK, Sarosi GA. The role of atypical pathogens in community-acquired pneumonia. Med Clin North Am. 2001. 85:1349–1365.

22. Cosentini R, Blasi F, Raccanelli R, Rossi S, Arosio C, Tarsia P, Randazzo A, Allegra L. Severe community-acquired pneumonia: a possible role for Chlamydia pneumoniae. Respiration. 1996. 63:61–65.
23. Ruiz M, Ewig S, Torres A, Arancibia F, Marco F, Mensa J, Sanchez M, Martinez JA. Severe community-acquired pneumonia Risk factors and follow-up epidemiology. Am J Respir Crit Care Med. 1999. 160:923–929.
24. Plouffe JF, File TM Jr, Breiman RF, Hackman BA, Salstrom SJ, Marston BJ, Fields BS. Community Based Pneumonia Incidence Study Group. Reevaluation of the definition of Legionnaires' disease: use of the urinary antigen assay. Clin Infect Dis. 1995. 20:1286–1291.

25. Benson RF, Tang PW, Fields BS. Evaluation of the Binax and Biotest urinary antigen kits for detection of Legionnaires' disease due to multiple serogroups and species of Legionella. J Clin Microbiol. 2000. 38:2763–2765.
26. Helbig JH, Uldum SA, Luck PC, Harrison TG. Detection of Legionella pneumophila antigen in urine samples by the BinaxNOW immunochromatographic assay and comparison with both Binax Legionella Urinary Enzyme Immunoassay (EIA) and Biotest Legionella Urin Antigen EIA. J Med Microbiol. 2001. 50:509–516.

27. Dominguez JA, Gali N, Pedroso P, Fargas A, Padilla E, Manterola JM, Matas L. Comparison of the Binax Legionella urinary antigen enzyme immunoassay (EIA) with the Biotest Legionella Urin antigen EIA for detection of Legionella antigen in both concentrated and nonconcentrated urine samples. J Clin Microbiol. 1998. 36:2718–2722.
28. Menendez R, Cordoba J, de La Cuadra P, Cremades MJ, Lopez-Hontagas JL, Salavert M, Gobernado M. Value of the polymerase chain reaction assay in noninvasive respiratory samples for diagnosis of community-acquired pneumonia. Am J Respir Crit Care Med. 1999. 159:1868–1873.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download