Abstract
Although the etiology of Behçet's Disease (BD; MIM 109650) remains to be clearly elucidated, levels of tumor necrosis factor alpha (TNF-α) have been reported to be significantly elevated in BD patients, and TNF-α blockers have been demonstrated to exhibit some degree of therapeutic efficacy for a certain subset of BD sufferers. In this study, we have conducted an analysis of the TNFA haplotypes in the promoter response element that affect the binding affinity of specific transcription factors, in order to characterize their association with the clinical features of BD. Six polymorphisms in the promoter region of TNFA were genotyped in 254 BD patients and 344 control subjects, via the PCR-RFLP technique. TNFA -1031*C, -863*A and -308*G alleles were associated with an increased risk of BD (p=0.030, OR=1.4; p=0.008, OR=1.5; p=0.010, OR=1.8, respectively). The sole TNFA haplotype -1031C-863A-857C-376G-308G-238G, was associated with a 1.6 fold increase in the risk of BD, whereas the TNFA haplotype -1031T-863C-857C-376G-308A-238G was associated with a 0.6 decreased risk of BD. The TNFA -1031*C, -863*A, -857*C and -308*G alleles were significantly associated with BD. The findings of this study, collectively, indicate that TNFA haplotypes in the promoter response elements may exert significant influence on susceptibility to BD.
Behçet's Disease (BD; MIM 109650) is a chronic multisystem inflammatory disorder of unclear etiology, which is characterized by primary features including recurrent oral and genital ulcers as well as skin and ocular lesions. Other minor manifestations of BD include arthritis, large vessel involvement (LVI), and lesions of central nervous system (CNS) and gastrointestinal (GI) tract. The mean age of onset of BD is in the early 30s, and the male-to-female ratio varies with ethnicity (1). Although the precise pathogenesis of BD remains a matter of some controversy, genetic, immunological, and environmental factors have been suggested to contribute to the development of BD (2). Several susceptibility variant genetic alleles, including alleles of Th1 cytokine-associated genes, have been recognized for their effects on the clinical symptoms of BD. A recent study of Turkish multicase families identified several BD susceptibility loci, via whole-genome linkage analysis. The loci with the strongest association with BD were detected at positions 6p22-24 and 12p12-13 (3).
Tumor necrosis factor alpha (TNF-α) is a multifunctional, pro-inflammatory cytokine, which performs a variety of functions in innate immune response, including activation of macrophages and apoptosis, which appears to be responsible for the recurrent inflammatory reactions encountered in BD patients. The promoter polymorphism of theTNFA gene, which is located on chromosome 6p21.3, has been associated with the expression of TNF-α. TNF-α levels tend to be significantly elevated in active BD patients, and increased production of TNF-α have been associated with clinical deterioration (4,5). Several single nucleotide polymorphisms (SNPs) in the TNFA promoter region appear to alter transcription efficiency in response to specific external stimuli (6-8). Excessive or insufficient TNF-α production might be responsible for the variable patterns of the pathogenesis of this disease. These SNPs, as well as TNF-α overproduction, have been associated with susceptibility to or with the severity of, both inflammatory diseases and autoimmune diseases, including rheumatoid arthritis, systemic lupus erythematosus, and Crohn's disease (9). There is, currently, a large body of evidence from in vitro experiments which suggests that TNF-α is produced at higher levels in both the monocytes and γ/δ T cells of BD patients in response to lipopolysaccharide treatment than has been observed in control subjects. However, the mechanism underlying this phenomenon remains to be determined (10, 11). Also, infliximab (monoclonal anti-TNF-α antibody) and etanercept (a dimeric soluble p75 TNF receptor) have demonstrated a high degree of therapeutic efficacy for suffers of BD coupled with uveitis, intestinal ulcers, and orogenital ulcers (12, 13).
Researchers have been attempting for several years to determine whether polymorphisms of the TNFA promoter region influence the expression of TNF-α in BD or its susceptibility or its severity and clinical features. The results of these allelic and genotypic associations, however, are somewhat contradictory, as the implicated polymorphic sites and allele frequencies appear to vary substantially among ethnic groups (14, 15). Most notably, -376G>A and -308G>A are either completely absent or quite rare among Asians, including the Koreans and the Japanese (6,16,17). Therefore, this study was focused specifically on the haplotypic association of TNFA promoter response elements with the risks and clinical features of BD.
Two hundred fifty-four patients (130 males and 124 females) from 16 to 66 yr of age registered at the Behçet's Disease Specialty Clinic of Severance Hospital at the Yonsei University College of Medicine and the Ajou University School of Medicine and 344 healthy Korean controls were included in this case-control study. The youngest onset of BD was 3 yr old and the oldest onset was 58 yr old and the mean age of disease onset was 33.2±10.4 yr old. BD was diagnosed according to the clinical criteria of the International Study Group for Behçet's Disease or the revised criteria of Behçet's Disease(18).
Genomic DNA was extracted from peripheral blood by using a QIAamp Blood Mini kit (Quiagen, Valencia, CA, U.S.A.). Six SNPs in the promoter region of TNFA gene at the position of -1031 T>C, -863 C> A, -857 C>T, -376 G>A, -308 G>A and -238 G>A (according to GenBank accession No. AB088112) were analyzed by using polymerase chain reaction (PCR) and restriction fragment length polymorphism (RFLP) methods. The -1031 T>C was amplified with PCR by using primers 5'-ACAAGGCTGACCAAGAGAGAA-3' and 5'-GTCCCCATACTCGACTTTCAT-3'and was digested with the BbsI restriction enzyme (19). The -863 C>A was amplified by using primers 5'-GGCTCTGAGGAATGGGTTAC-3'and 5'-CTACATGGCCCTGTCTTCGTTACG-3' and was digested with the TaiI restriction enzyme (20). The reverse primer contained one mismatched nucleotide sequence (underlined). Genotyping for -857C>T was conducted by using the forward primer 5'-AAGTCGAGTATGGGGACCCCCCGTTAA-3'and the reverse primer 5'-CCCCAGTGTGTGGCCATATCTTCTT-3'which made it possible to use the restriction enzyme HincII (19). The G>A substitution at position -376 was analyzed by the Tsp509I restriction enzyme by using the primers, 5'-CCCCGTTTTCTCTCCCTCAA-3'and 5'-TGTGGTCTGTTTCCTTCTAA-3'(21). The polymorphic region containing the NcoI restriction site at -308 G>A was amplified by using primers 5'-AGGCAATAGGTTTTGAGGGCCAT-3'and 5'-TCCTCCCTGCTCCGATTCCG-3'. The G>A transition polymorphism at position -238 was examined by PCR using primers 5'-CCCAGAAGACCCCCCTCGGAACC-3'and 5'-ACCTTCTGTCTCGGTTTCTTCTCCATCGC-3'and was digested with the HpaII restriction enzyme (19). The digested PCR products were electrophoresis on an 8% or 5% polyacrylamide gel and were stained with ethidium bromide to visualize the DNA fragments.
The Hardy-Weinberg equilibrium and Linkage disequilibrium coefficient Lewontin's D'(¦D'¦) were performed with the R program v.1.9.1 (http://cran.r-project.org). The statistical significance of the difference in TNFA allele frequencies between BD patients and controls was examined by the χ2 or Fisher's exact test by using SAS version 8.1 (SAS Institute, Cary, NC, U.S.A.). Haplotypes of each individual were inferred by using the PHASE program, v.2.0.1 (22). A p-value of less than 0.05 was considered statistically significant.
A total of 254 Korean BD patients and 344 control subjects were analyzed for six SNPs in the TNFA promoter region. The genotype and allele frequencies of the regulatory response element promoter polymorphisms TNFA gene of the BD patients and controls are shown in Table 1. Distributions of the genotypes of both groups agree with those predicted under the conditions of Hardy-Weinberg equilibrium. The TNFA -376G>A was not polymorphic in the Korean population. The TNFA -1031*C, -863*A and -308*G alleles are shown to be significantly associated with BD (p=0.030, odds ratio [OR]=1.4; p=0.008, OR=1.5; p=0.010, OR=1.8, respectively). They were significantly higher in the BD patients suffering from major symptoms (OR=1.4-1.9) and arthritis(OR=1.4-2.9) than in the controls (Table 2). There was no association between the presence of minor -238*A allele and the symptoms of BD except for BD with GI lesions.
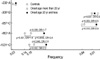
The age at which an individual first manifests major symptoms of the BD appears to be genetically influenced. The TNFA promoter SNPs influenced the age onset (before 20 yr) in BD. The TNFA -1031*C, -863*A and -857*C alleles were shown to have a significantly higher association among the BD patients whose onset age is younger than 20 yr old when compared with those whose onset age is after 20 yr old (p=0.03-0.04, OR=1.6-2.5). Significant differences between BD and controls were observed in the distribution of TNFA -1031*C, -863*A and -857*C did show significantly higher ORs in the early onset age group than the later onset age group (OR=1.6-2.5) (Fig. 1).
TNFA promoter polymorphisms showed linkage disequilibrium in the Korean population (Table 3). The TNFA-1031*T was strong associated with -863*C (p<0.0001) and -857*C (p<0.0001). The -863*C was in linkage disequilibrium with the -857*C (p=0.0003). Among 22 estimated haplotypes, the most common haplotype, TNFA -1031T-863C-857C-376G-308G-238G (55%) and six common TNFA haplotypes were observed in the Korean population. The overall haplotype distributions were found to be significantly different between the BD patients and the controls by the permutation test (p=0.02). The TNFA -1031C-863A-857C-376G-308G-238G haplotype containing the three alleles TNFA -1031*C, -863*A and -308*G was found to be significantly associated with BD. Conversely, the TNFA -1031T-863C-857C-376G-308A-238G which did not have these alleleic polymorphisms was protective against BD (Table 4).
The patients were characterized by clinical features whose major/minor symptoms were oral, genital ulcers, skin, ocular lesions, arthritis, and LVI. The CNS and GI lesions are rare. We investigated the clinical features of the TNFA haplotypepositive individuals in terms of the frequency of the haplotype, TNFA -1031C-863A-857C-376G-308G-238G, which contains the three alleles -1031*C, -863*A and -308*G. Being compared with the controls, it was significantly over-represented among patients (OR=1.6-3.0) who suffered from oral and genital ulcers, skin and ocular lesions, arthritis and CNS but not among those who suffered from LVI or GI lesions. On the other hand, the haplotype TNFA -1031T-863C-857C-376G-308A-238G which does not carry those alleles were shown to significantly reduce the risk of BD than in controls (p=0.029-0.013, OR=0.4-0.6) (Table 4). Frequencies of TNFA -1031T-863C-857T-376G-308G-238G and TNFA -1031C-863C-857C-376G-308G-238A haplotypes in the patients with CNS or GI lesions significantly differed from those in the controls, but the number of patients was too small for a statistical analysis (Table 4).
Both clinical and polymorphism-focused studies have uncovered evidence suggesting that TNF-α functions as a mediator in the initiation and propagation of BD. Polymorphisms of the TNFA promoter region have been associated with BD in several ethnic groups, but it remains somewhat uncertain as to whether this is the results of the existence of susceptibility sites, or to the level of TNF-α expression. In this study, a significant difference was observed between BD patients and controls with regard to the polymorphisms of the regulatory response promoter region of the TNFA gene. The alleles, TNFA -1031*C, -863*A and -308*G were closely associated with BD, but TNFA -376G>A and -238G>A were not significantly associated among Korean sufferers of BD. These results are consistent with findings of studies employing different ethnic groups. The TNFA -1031*C allele was strongly association with BD in Caucasian patients, in a previous study conducted in the United Kingdom (23). The other previous studies involving Turkish and Caucasian patients, the TNFA -376G>A, -308G>A and -238G>A alleles were not significantly associated with BD (15,23-25). In studies of haplotypes of the TNFA promoter, the TNFA -1031C-863A-857C-376G-308G-238G haplotype, which harbors the -1031*C, -863*A and -308*G alleles, was significantly associated with BD. Conversely, the TNFA -1031T-863C-857C-376G-308A-238G haplotype, which does not harbor the aforementioned allelic polymorphisms, was associated with a reduced susceptibility to BD. The same results were reported in Caucasian BD patients in the United Kingdom (23). We compared the risk of BD between the early onset age group and the later onset of group, with regard to the TNFA alleles. The -1031*C, -863*A and -857*C alleles were detected with a significantly greater frequency in the former than in the latter.
Inflammation in cases of BD is believed to be mediated by cytokines derived from T-helper type 1 lymphocytes, including TNF-α(26). It appears that disease activity can be significantly associated with the secretion of pro-inflammatory mediators, as the result of the direct activation of circulating monocytes. The pro-inflammatory cytokine, TNF-α , triggers a signaling cascade, converging on the activation of the NF-κB transcription factor, which is also involved in a variety of features of immune response, which in turn constitutes the basis for a host of physiological and pathological processes. The TNF-α/NF-κB pathway also appears to be relevant to human diseases (27). The enhanced/silenced expression of pro-inflammatory cytokines indicates the presence of a defect in the normal regulatory mechanisms, and this may have a genetic basis. Much of the control of gene expression appears to involve transcription factors (trans-acting) bound to proximal promoter regulatory response sequences (cis-acting). Gene expression is mediated by several sets of cis-acting regulatory regions, including the core or proximal promoter region, and the response elements. The response elements modulate transcription in response to specific external stimuli, including heat shock 70 or interferon-gamma. The response elements are normally located a short distance upstream of the promoter elements. Allele-specific elements may bind the transcriptional factors, OCT-1 and NF-κB, in the -1031T>C, -863C>A and -857C>T of the TNFA regulatory response promoter region, which are thought to be involved in a variety of the immune response functions. Although the roles of the allele-dependent binding elements of TNFA -1031, -863 and -857 SNPs have yet to be precisely delineated, the susceptible sites associated with the development of BD are in the -1031T>C, -863C>A and -857C>T SNPs of the regulatory response promoter region, and not in -376G>A, -308G>A or -238G>A (6,15,28-30). These SNPs also evidenced no relationship with the degree of severity of the clinical features of BD (15).
The pro-inflammatory cytokines, TNF-α and mannosebinding lectin (MBL), are potent inducers of inflammation. Elevated levels of these cytokines are frequently associated with the activation of macrophages, thereby influencing the severity of inflammatory responses. Both of these pro-inflammatory cytokines induce local inflammatory responses, and also exert systemic effects. The over-expression of these cytokines may be responsible for the pathogenesis of recurrent BD. It has been reported previously that the MBL2 HYPA haplotype, which induces an elevate expression of MBL, was related to susceptibility to BD, and also to the early onset of disease (31,32). TNF-α production tended to be elevated in carriers of the TNFA -1031*C, -863*A or -857*T alleles, who also suffered from severe periodontitis (19). The frequency with which individuals were determined to harbor both the TNFA -1031C-863A-857C-376G-308Gand MBL2 HY-- (-550*G, -221*G) haplotypes was significantly higher in the BD patient group than among the controls (p=0.004). The elevated production of TNF-α and MBL2 haplotypes might serve to accelerate recurrent inflammation, or may play a critical pathogenic role in initiating immune responses, which might also result in the development of BD. A host of genes appear to be related to BD susceptibility, and the TNFA promoter haplotypes appear to be fairly important markers with regard to their association with BD.
In conclusion, the findings of this study indicate that the TNFA -1031C-863A-857C-308G haplotype can be confidently associated with the development of BD as well as early age of onset. This haplotype was also determined to be responsible for the enhanced inflammatory reactions seen in cases of BD involving primary symptoms.
Figures and Tables
References
1. Bang DS, Oh SH, Lee KH, Lee ES, Lee SN. Influence of sex on patients with Behcet's disease in Korea. J Korean Med Sci. 2003. 18:231–235.

2. Zierhut M, Mizuki N, Ohno S, Inoko H, Gul A, Onoe K, Isogai E. Immunology and functional genomics of Behcet's disease. Cell Mol Life Sci. 2003. 60:1903–1922.
3. Karasneh J, Gul A, Ollier WE, Silman AJ, Worthington J. Whole-genome screening for susceptibility genes in multicase families with Behcet's disease. Arthritis Rheum. 2005. 52:1836–1842.
4. Oztas MO, Onder M, Gurer MA, Bukan N, Sancak B. Serum interleukin 18 and tumor necrosis factor-alpha levels are increased in Behcet's disease. Clin Exp Dermatol. 2005. 30:61–63.
5. Sayinalp N, Ozcebe OI, Ozdemir O, Haznedaroglu IC, Dundar S, Kirazli S. Cytokines in Behcet's disease. J Rheumatol. 1996. 23:321–322.
6. Higuchi T, Seki N, Kamizono S, Yamada A, Kimura A, Kato H, Itoh K. Polymorphism of the 5'-flanking region of the human tumor necrosis factor (TNF)-alpha gene in Japanese. Tissue Antigens. 1998. 51:605–612.
7. Wilson AG, Symons JA, McDowell TL, McDevitt HO, Duff GW. Effects of a polymorphism in the human tumor necrosis factor alpha promoter on transcriptional activation. Proc Natl Acad Sci USA. 1997. 94:3195–3199.
8. Kroeger KM, Carville KS, Abraham LJ. The -308 tumor necrosis factor-alpha promoter polymorphism effects transcription. Mol Immunol. 1997. 34:391–399.
9. Negoro K, Kinouchi Y, Hiwatashi N, Takahashi S, Takagi S, Satoh J, Shimosegawa T, Toyota T. Crohn's disease is associated with novel polymorphisms in the 5'-flanking region of the tumor necrosis factor gene. Gastroenterology. 1999. 117:1062–1068.

10. Mege JL, Dilsen N, Sanguedolce V, Gul A, Bongrand P, Roux H, Ocal L, Inanc M, Capo C. Overproduction of monocyte derived tumor necrosis factor alpha, interleukin (IL) 6, IL-8 and increased neutrophil superoxide generation in Behcet's disease. A comparative study with familial Mediterranean fever and healthy subjects. J Rheumatol. 1993. 20:1544–1549.
11. Yamashita N, Kaneoka H, Kaneko S, Takeno M, Oneda K, Koizumi H, Kogure M, Inaba G, Sakane T. Role of γ/δ T lymphocytes in the development of Behcet's disease. Clin Exp Immunol. 1997. 107:241–247.

12. Sfikakis PP, Theodossiadis PG, Katsiari CG, Kaklamanis P, Markomichelakis NN. Effect of infliximab on sight-threatening panuveitis in Behcet's disease. Lancet. 2001. 358:295–296.

13. Melikoglu M, Fresko I, Mat C, Ozyazgan Y, Gogus F, Yurdakul S, Hamuryudan V, Yazici H. Short-term trial of etanercept in Behcet's disease: a double blind, placebo controlled study. J Rheumatol. 2005. 32:98–105.
14. Allen RD. Polymorphism of the human TNF-alpha promoter; random variation or functional diversity? Mol Immunol. 1999. 36:1017–1027.
15. Ates AK, Kinikli G, Duzgun N, Duman M. Lack of association of tumor necrosis factor-alpha gene polymorphisms with disease susceptibility and severity in Behcet's disease. Rheumatol Int. 2006. 26:348–353.
16. Wang XT, Ohtsuka Y, Kimura K, Muroi M, Ishida T, Saito J, Munakata M. Antithetical effect of tumor necrosis factor-alpha gene polymorphism on coal workers' pneumoconiosis (CWP). Am J Ind Med. 2005. 48:24–29.
17. Lee EB, Kim JY, Lee YJ, Park MH, Song YW. TNF and TNF receptor polymorphisms in Korean Behcet's disease patients. Hum Immunol. 2003. 64:614–620.
18. International Study Group for Behcet's Disease. Criteria for diagnosis of Behcet's disease. Lancet. 1990. 335:1078–1080.
19. Soga Y, Nishimura F, Ohyama H, Maeda H, Takashiba S, Murayama Y. Tumor necrosis factor-alpha gene (TNF-alpha) -1031/-863, -857 single-nucleotide polymorphisms (SNPs) are associated with severe adult periodontitis in Japanese. J Clin Periodontol. 2002. 30:524–531.
20. Skoog T, van't Hooft FM, Kallin B, Jovinge S, Boquist S, Nilsson J, Eriksson P, Hamsten A. A common functional polymorphism (C->A substitution at position -863) in the promoter region of the tumour necrosis factor-alpha (TNF-alpha) gene associated with reduced circulating levels of TNF-alpha. Hum Mol Genet. 1999. 8:1443–1449.
21. Moukoko CE, El Wali N, Saeed OK, Mohamed-Ali Q, Gaudart J, Dessein AJ, Chevillard C. No evidence for a major effect of tumor necrosis factor alpha gene polymorphisms in periportal fibrosis caused by Schistosoma mansoni infection. Infect Immun. 2003. 71:5456–5460.
22. Stephens M, Smith NJ, Donnelly P. A new statistical method for haplotype reconstruction from population data. Am J Hum Genet. 2001. 68:978–989.

23. Ahmad T, Wallace GR, James T, Neville M, Bunce M, Mulcahy-Hawes K, Armuzzi A, Crawshaw J, Fortune F, Walton R, Stanford MR, Welsh KI, Marshall SE, Jewell DP. Mapping the HLA association in Behcet's disease: a role for tumor necrosis factor polymorphisms? Arthritis Rheum. 2003. 48:807–813.
24. Duymaz-Tozkir J, Gul A, Uyar FA, Ozbek U, Saruhan-Direskeneli G. Tumour necrosis factor-alpha gene promoter region -308 and -376 G-->A polymorphisms in Behcet's disease. Clin Exp Rheumatol. 2003. 21:Suppl 30. 15–18.
25. Oz D, Karsli F, Atalay A, Sahin S. Bang D, Lee ES, Lee S, editors. TNF-alpha gene polymorphisms in Behcet's disease. Proceedings of the 9th international conference on Behcet's disease. 2000. Seoul: Design Mecca Publishing;161–165.
26. Gul A. Behcet's disease: an update on the pathogenesis. Clin Exp Rheumatol. 2001. 19:Suppl 24. 6–12.
27. Bouwmeester T, Bauch A, Ruffner H, Angrand PO, Bergamini G, Croughton K, Cruciat C, Eberhard D, Gagneur J, Ghidelli S, Hopf C, Huhse B, Mangano R, Michon AM, Schirle M, Schlegl J, Schwab M, Stein MA, Bauer A, Casari G, Drewes G, Gavin AC, Jackson DB, Joberty G, Neubauer G, Rick J, Kuster B, Superti-Furga G. A physical and functional map of the human TNF-alpha/NF-kappa B signal transduction pathway. Nat Cell Biol. 2004. 6:97–105.
28. Udalova IA, Richardson A, Denys A, Smith C, Ackerman H, Foxwell B, Kwiatkowski D. Functional consequences of a polymorphism affecting NF-kappaB p50-p50 binding to the TNF promoter region. Mol Cell Biol. 2000. 20:9113–9119.
29. van Heel DA, Udalova IA, De Silva AP, McGovern DP, Kinouchi Y, Hull J, Lench NJ, Cardon LR, Carey AH, Jewell DP, Kwiatkowski D. Inflammatory bowel disease is associated with a TNF polymorphism that affects an interaction between the OCT1 and NF (-kappa) B transcription factors. Hum Mol Genet. 2002. 11:1281–1289.
30. Verity DH, Wallace GR, Vaughan RW, Kondeatis E, Madanat W, Zureikat H, Fayyad F, Marr JE, Kanawati CA, Stanford MR. HLA and tumour necrosis factor (TNF) polymorphisms in ocular Behcet's disease. Tissue Antigens. 1999. 54:264–272.

31. Park KS, Min K, Nam JH, Bang D, Lee ES, Lee S. Association of HYPA haplotype in the mannose-binding lectin gene-2 with Behcet's disease. Tissue Antigens. 2005. 65:260–265.

32. Madsen HO, Garred P, Thiel S, Kurtzhals JA, Lamm LU, Ryder LP, Svejgaard A. Interplay between promoter and structural gene variants control basal serum level of mannan-binding protein. J Immunol. 1995. 155:3013–3020.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download