Abstract
Polyarteritis nodosa (PAN) is a systemic vasculitis characterized by multi-organ involvement with protean manifestations. We evaluated the clinical features of PAN in Korea. Twenty-seven patients were diagnosed as PAN at Seoul National University Hospital between January 1990 and July 2003. The male-to-female ratio was 1.7:1 and mean age at onset (±SD) was 47.4±20 yr. Their presenting features at diagnosis were similar to those reported previously, i.e., myalgia, muscle weakness or leg tenderness (70%), fever (52%), weight loss >4 kg (44%), skin rash (44%), peripheral edema (33%), abdominal pain (33%), and arthralgia/arthritis (30%). However, the prevalence of testicular pain or tenderness was higher (24%) than reported previously and only three (11.5%) had HBsAg positivity without liver enzyme elevation. Nine patients (33%) had a five-factor score (FFS) of 2. Fourteen patients (52%) responded to treatment, 2 patients relapsed and 4 died within 1 yr of diagnosis. During a median follow-up of 55.5 months, three of the four PAN-related deaths had an initial FFS of 2. The clinical features of PAN were not significantly different from those reported previously. However, testicular pain or tenderness was more frequent and patients with a high FFS tended to have a poorer prognosis.
Polyarteritis nodosa (PAN) is an uncommon systemic necrotizing vasculitis and is characterized by the presence of inflammatory reactions of medium or small-sized blood vessels with multiorgan involvements including skin, kidney, peripheral nerve, muscle, gastrointestinal tract and others (1,2). PAN was first described by Kussmaul and Maier in 1866 and many reports have been issued on its clinical features. In Korea, dozens of case reports and two papers on cutaneous PAN have been published (3,4). Although the prevalence of hepatitis B is high in Korea and the association between PAN and hepatitis B is well known, no study about clinical features of systemic PAN has been conducted. Thus we analyzed the clinical features of classic PAN in Korea.
We searched the database of Seoul National University Hospital for adult PAN patients (age ≥16 yr old) between January 1990 and July 2003. Thirty six patients were first suspected of having PAN and 27 of these satisfied the American College of Rheumatology (ACR) 1990 criteria for the classification of PAN. Thus, 9 patients were excluded; 4 had a limited form of PAN and five had a cutaneous form. All limited and cutaneous PAN patients showed no evidence of other organ involvement or of a saccular aneurysm by angiography. The male-to-female ratio was 1.7:1, mean age of onset was 47.4±20 yr and the median follow up period was 55.5 months (range 0.6-162 month).
We retrospectively reviewed the medical records of 27 patients with PAN satisfying the ACR 1990 criteria. The parameters studied were gender, age, follow-up time, symptoms and signs at onset, ACR criteria for PAN, organ involvement, and laboratory findings. Symptoms and signs at onset included; fever, arthralgia and arthritis, peripheral edema, abdominal pain, hepatomegaly, subcutaneous nodule, lymphadenitis, peripheral ischemia, and sinusitis.
The other clinical features according to the ACR criteria were weight loss >4 kg, skin rash, testicular pain or tenderness, myalgia, weakness or leg tenderness, neuropathy, hypertension, elevated blood urea nitrogen (BUN) or creatinine, the presence of hepatitis B surface antigen (HBsAg) or hepatitis B surface antibody (HbsAb), an arteriographic and histopathologic abnormality. Organ involvement was divided into joint or muscle, peripheral nerve, skin, kidney, gastrointestinal tract, central nervous system, heart, and lung.
In addition, laboratory tests at the time of diagnosis of PAN included; hemoglobin, white blood cell and platelet counts, Westergren erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), anti-streptolysin O (ASO), complement 3 (C3), antinuclear antibody, rheumatoid factor, and antineutrophil cytoplasmic antibody (ANCA). Angiographic and histopathologic findings were also obtained. A positive angiographic finding of PAN was defined as the presence of microaneurysm or stenosis (narrowing or tapering) of medium-sized vessels, and a positive pathologic finding was considered as focal segmental necrotizing vasculitis of medium- and small-sized arteries.
For the treatment and prognosis of PAN, we analyzed medications, response to medications, post-treatment recurrence or death, and causes of death. A five-factor score (FFS) at the time of diagnosis was calculated to evaluate the association with mortality. These 5 factors were; proteinuria >1 g/day, renal insufficiency (serum creatinine >1.58 mg/dL), gastrointestinal symptoms, cardiomyopathy, and centel nervous system involvement(5-7). If patients were lost to follow at our hospital, we interviewed them or their first-degree relatives to check upon recurrence or cause of death. Kaplan-Meier survival curves were plotted.
The ages of patients were evenly distributed from 17 to 72 yr old. Clinical features at the time of diagnosis are summarized in Table 1. Over half of the patients had fever at the time of onset. The average number of 1990 ACR criteria per patient was 4.67 (range 3-7), and the most prevalent items were histopathologic abnormality (96%), and myalgia, weakness and leg tenderness (70%), followed by neuropathy (63%), positive HBsAg or HBsAb (56%), weight loss >4 kg (44%), skin rash (44%), arteriographic abnormality (40%), elevated BUN or creatinine (30%), hypertension (30%) and testicular pain or tenderness (24%) (Table 2).
The distribution of organ involvement was as follows; joint or muscle (65%), peripheral nerve (63%), skin (44%), kidney (48%), gastrointestinal tract (48%), central nervous system (7%), heart (7%), and lung (4%). Skin rash included livedo reticularis (3 of 12), erythema nodosum (3/12), and maculopapular rash (6/12).
When FFS was analyzed to evaluate its association with PAN related mortality, 10 (37%) patients had an FFS of 0, 8 (29.6%) an FFS of 1, and 9 an FFS of 2 (33.3%). Of the 9 patients with an FFS of 2, four died. The hazard ratio (HR) of mortality associated with an FFS=2 was 2.22 (Table 5).
Laboratory findings are summarized in Table 3. Fourteen (52%) patients had an elevated acute phase reactant (ESR >40 mm/hr or CRP >0.5 mg/dL). Fourteen (56%) patients were HBsAg or HBsAb positive; however, only three among them showed HBsAg positivity and they did not have elevated liver enzymes. One of three HBsAg positive patients became negative for HBsAg but positive for anti-HBc antibody. Five (19%) patients were ANCA positive; three c-ANCA and two p-ANCA. Twenty-six patients underwent tissue biopsy of muscle, nerve, skin, or GI tract. istopathological findings were necrotizing inflammation of medium-sized or small arteries in 25 patients (Table 2). Twenty patients underwent diagnostic angiography and 8 (40%) had positive angiographic findings for renal artery (5 cases), superior mesenteric artery (2 cases), hepatic artery (1 case), brachial artery (1 case), or tibial artery (1 case).
Treatment regimens included prednisolone alone (14 cases), prednisolone plus cyclophosphamide (11 cases), prednisolone plus other immunosuppressant (azathioprine, cyclosporine) (2 cases). In our study, no one was treated with an HBV antiviral agent.
One year after treatment, 14 patients (52%) responded to their medication, 2 patients (7%) relapsed and 4 patients (15%) died. Seven patients (26%) were lost to follow up and their data were collected by telephone interviewing afterwards. Of the patients who were lost to follow up, one relapsed and was followed by another hospital, three were living asymptomatically without treatment, two died from an accident, and one could not be reached.
Although one relapsed and four died among the 14 patients in the prednisolone alone group, only one relapsed out of 11 patients in the prednisolone plus cyclophosphamide group at one year after treatment.
During a median follow-up of 55.5 months, 4 cases relapsed (median: 44.5 months). However, the relapsed patients responded to increments in prednisolone dosage or the addition of another immunosuppressant, and no further mortality occurred among the relapsed cases.
Eight deaths occurred during follow-up; four were vasculitis-related deaths, i.e., multiorgan failure (1), subarachnoid hemorrhage (1), and renal failure (2). Three of the patients that succumbed had an initial FFS of 2 and one patient had an FFS of one (Table 5). The mean age of these 4 patients at diagnosis was 62 yr. All disease-related deaths occurred within 6 months of diagnosis. Excluding a gastric cancer patient, mortality among patients with an FFS of 2 was 33.3% (Table 5). No death was associated with a treatment related side effect. Four deaths were unrelated to disease, i.e., lymphoma with pneumonia (49 months after diagnosis), gastric cancer (1 month after diagnosis), and two accidental deaths (Fig. 1).
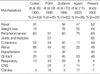
This study was conducted to investigate the clinical manifestation and the course of PAN in Korean patients. All patients were collected according to ACR criteria. Chapel Hill Consensus Conference defined PAN as necrotizing inflammation of medium-sized or small arteries without glomerulonephritis or vasculitis in arterioles, capillaries, or venules (2). Thus patients with glomerulonephritis were not present in our patients population. Overall clinical manifestations and disease courses were similar to those reported by other studies (Table 4) (8-11), which reported high incidence of involvement of; peripheral nerve (51-75%), muscle and joint (51%), skin (11-58%), kidney (22-66%), hypertension (14-32%), gastrointestinal tract (25-53%), central nervous system (2-24%), heart (4-18%), and lung (6-40%)(Table 4) (8-11).
The reported incidence of orchitis/epididymitis by autopsy studies vary from 60 to 80% (11,20,32), but symptomatic testicular pain is an infrequent presenting manifestation of PAN, and a few reports quote a rate of at presentation orchitis/epididymitis of 2-18% (11,20-23). Our study showed a high rate (24%) of testicular pain or tenderness. These results suggest that orchitis/epididymitis requires cautious checking in Koreans in the presence of musculoskeletal symptoms, livedo reticularis, or mono- or polyneuropathic symptoms and signs.
Some reports have categorized small vessel vasculitis largely into ANCA-associated vasculitis and immune-complex vasculitis (13,14). Several groups concluded after a careful histological examination that ANCA is strongly correlated with small-sized vessel involvement (7,9,12). ANCA-associated vasculitis is the most common primary systemic small vessel vasculitis in adults and includes three major categories: microscopic polyangiitis, Wegener's granulomatosis and Churg-Strauss syndrome (7,15-18). On the contrary, PAN is not known to have a high positive rate of ANCA (13,19). Our study shows a 14% ANCA positivity rate which is comparable to other foreign reports which showed up to 20%.
Sergent et al. presented substantial evidence which indicated that at least one subset of PAN patients experienced systemic vasculitis as a result of chronic hepatitis B virus associated immune complex disease(24). Guillevin et al. in France in a 1981-1992 study also reported that 25-30% of PAN patients are associated with hepatitis B, based on HBsAg positivity (10); however, the rate in the general French population was only 0.3% (25-27). In 1990, ACR proposed PAN classification criteria, which included the presence of HBsAg or HBsAb in serum as criteria (1). Recent epidemiologic data from northeast Asian countries including Korea, China, Taiwan, and Japan, show that the HBsAg positive rate, even after the 1983 global hepatitis B vaccination program was introduced in Korea, is at 4-6%. Also, taking into consideration HBsAb positive rate of 70-80%, the ACR PAN criteria may produce a bias in the northeast Asian population that causes over-diagnosis of PAN (28-31). A large scale epidemiologic study may be necessary to investigate whether the high positive rates of HBsAg and HBsAb influence the diagnosis and prevalence of PAN in Korea.
Old age could be an important prognostic factor. The average age of the four fatal vasculitis patients that died was 62 yr, which exceeded the total patient average age of 47.4 yr. According to Guillevin et al., the critical period in terms of mortality is the first year of the disease (5-7). Our study also showed no disease related death occurred after 7 months from the diagnosis.
Guillevin et al. established FFS after subjecting every clinical item to univariate and multivariate analyses (11), and FFS items found to be significantly associated with an increased mortality, namely, renal insufficiency, proteinuria and/or gastrointestinal tract involvement, were found to be the major factors associated with a poor prognosis. They also suggested that renal insufficiency (Cr >1.58 mg/dL) and severe gastrointestinal involvement necessitating surgery are significant predictors of death (6). In our study no disease related mortality occurred in those with an FFS of 0, in contrast three of the four disease-related mortality cases had an FFS of 2. Disease-related mortality cases showed the following items of five factors; renal insufficiency (3 cases), cardiac involvement (2 cases), central nervous system involvement (1 case) and gastrointestinal tract involvement (1 case). Patients with a higher FFS tended to have a high HR compared with those with a lower FFS in the present study, even though statistical significance was not achieved due to the small number of cases (Table 5). FFS may help clinicians develop a prognostic approach to PAN and guide treatment choice (5-7).
Prednisolone based treatment is a well known treatment modality in PAN. Sometimes a cytotoxic agent and plasmapheresis are added. A cytotoxic agent is indicated for patients with disease refractory to corticosteroids or with serious major organ involvement (7). Plasmapheresis can be performed in fulminant disease or after the failure of another treatment but it may facilitate infection (6,7). Most reports on plasmapheresis are based on anecdotal trials or small scale studies. Our study shows no significant difference between the survival rates of those on prednisolone alone and prednisolone plus cytotoxic therapy. Moreover, long term treatment with a cytotoxic agent (e.g. cyclophosphamide) may result in a higher incidence on lymphoma or some other malignancy. We experienced a mortality in a case with non Hodgkin's lymphoma and pneumonia on cyclosporine treatment.
In conclusion, our study demonstrates that the clinical features of polyarteritis nodosa in Korea are similar to those described in other countries. However, the prevalence of testis involvement appears to be high, and patients with high FFS tended to have a poor prognosis.
Figures and Tables
Fig. 1
Kaplan-Meier survival curve of polyarteritis nodosa patients. This curve plots time to disease related death. Eight patients died during the follow up period. Among these, 4 patients died due to vasculitis related causes (multiorgan failure, subarachnoid hemorrhage, renal failure in 2 cases) within one year. Other causes of death were lymphoma (1 case), metastatic gastric cancer (1 case), and accidents (2 cases).

Table 2
Clinical features of polyarteritis nodosa patients according to the American College of Rheumatology (ACR) 1990 criteria

References
1. Lightfoot RW, Michel BA, Bloch DA, Hunder GG, Zvaifler NJ, McShane DJ, Arend WP, Calabrese LH, Leavitt RY, Lie JT, Masi AT, Mills JA, Stevens MB, Wallace SL. The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum. 1990. 33:1088–1093.

2. Jennette JC, Falk RJ, Andrassy K, Bacon PA, Churg J, Gross WL, Hagen EC, Hoffman GS, Hunder GG, Kallenberg CG, Mccluskey RT, Sinico RA, Rees AJ, Es La, Waldherr R, Wiik A. Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum. 1994. 37:187–192.
3. Lee CW, Kim YJ, Park MH. Clinical features of cutaneous polyarteritis nodosa. Korean J Dermatol. 1995. 33:225–231.
4. Yoon CH, Lee CW. Clinical patterns of cutaneous lesions on the legs in patients with cutaneous polyarteritis nodosa. Korean J Dermatol. 2003. 41:869–872.
5. Guillevin L, Le Thi Huong D, Godeau P, Jais P, Wechsler B. Clinical findings and prognosis of polyarteritis nodosa and Churg-Strauss angiitis: a study in 165 patients. Br J Rheumatol. 1988. 27:258–264.

6. Guillevin L, Lhote F, Gayraud M, Cohen P, Jarrousse B, Lortholary O, Lortholary O, Thibult N, Casassus P. Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome. A prospective study in 342 patients. Medicine (Baltimore). 1996. 75:17–28.

7. Guillevin L, Lhote F. Classification and management of necrotizing vasculitides. Drugs. 1997. 53:805–816.
8. Cohen RD, Conn DL, Ilstrup DM. Clinical features, prognosis, and response to treatment in polyarteritis. Mayo Clin Proc. 1980. 55:146–155.
9. Fortin PR, Larson MG, Watters AK, Yeadon CA, Choquette D, Esdaile JM. Prognostic factors in systemic necrotizing vasculitis of the polyarteritis nodosa group: a review of 45 cases. J Rheumatol. 1995. 22:78–84.
10. Guillevin L, Lhote F, Cohen P, Sauvaget F, Jarrousse B, Lortholary O, Noel LH, Trepo C. Polyarteritis nodosa related to hepatitis B virus. A prospective study with long-term observation of 41 patients. Medicine. 1995. 74:238–253.

11. Agard C, Mouthon L, Mahr A, Guillevin L. Microscopic polyangiitis and polyarteritis nodosa: how and when do they start? Arthritis Rheum. 2003. 49:709–715.

12. Lhote F, Guillevin L. Polyarteritis nodosa, microscopic polyangiitis, and Churg-Strauss syndrome. Clinical aspects and treatment. Rheum Dis Clin North Am. 1995. 21:911–947.
14. Cupps TR, Fauci AS. The Vasculitides. Major Probl Intern Med. 1981. 21:1–211.
16. Fauci AS. Braunwald E, Isselbacher KI, Petersdorf RG, Wilson JD, Martin JB, Fauci AS, editors. The vasculitis syndromes. Harrison's Principles of Internal Medicine. 1998. 14th ed. New York: McGraw-Hill;1912–1914.
19. Hoffman G, Specks U. Antineutrophil cytoplasmic antibodies. Arthritis Rheum. 1998. 41:1521–1537.

20. Wright LF, Bicknell SL. Systemic necrotizing vasculitis presenting as epididymitis. J Urol. 1986. 136:1094.

21. Tanuma Y, Oda T, Yokoo A, Ito S, Takeuchi K. Recurrent polyarteritis nodosa limited to the testis. J Urol. 2003. 170:1953.

22. Karyn SE, Stephen JF, Jacob R. Polyarteritis nodosa presenting as hematuria and a testicular mass. J Urol. 2001. 166:624.
23. Mukamel E, Abarbanel J, Savion M, Konichezky M, Yachia D, Auslaender L. Testicular mass as a presenting symptom of isolated polyarteritis nodosa. Am J Clin Pathol. 1995. 103:215–217.

24. Sergent JS, Lockshin MD, Christian CL, Gocke DJ. Vasculitis with hepatitis B antigenemia: long-term observation in nine patients. Medicine (Baltimore). 1976. 55:1–18.
25. Michault A, Faulques B, Sevadjan B, Troalen D, Marais A, Barau G. Prevalence of hepatitis A, B, C virus markers in Reunion (south hospital and Saint Pierre prison). Bull Soc Pathol Exot. 2000. 93:34–40.
26. Aker MI, Mast EE. The epidemiology of the viral hepatitis in the United States. Gastroenterol Clin North Am. 1994. 23:437–455.
27. Lepage L, Schiele F, Janot C, Siest G. Prevalence of viral hepatitis B markers in a sample population seen at a center of preventive medicine. Pathol Biol (Paris). 1986. 34:851–854.
28. Hsu HM, Lu CF, Lee SC, Lin SR, Chen DS. Seroepidemiologic survey for hepatitis B virus infection in Taiwan: the effect of hepatitis B mass immunization. J Infect Dis. 1999. 179:367–370.

29. Furusyo N, Hayashi J, Sawayama Y, Kawakami Y, Kishihara Y, Kashiwagi S. The elimination of hepatitis B virus infection: changing seroepidemiology of hepatitis A and B virus infection in Okinawa, Japan over a 26-year period. Am J Trop Med Hyg. 1998. 59:693–698.

30. Andre F. Hepatitis B epidemiology in Asia, the Middle East and Africa. Vaccine. 2000. 18:Suppl 1. 20–22.

31. Joo KR, Bang S, Song B, Youn KH, Joo YH, Yang S, Kim KR, Chung Y, Lee YS, Suh DJ. Hepatitis B viral markers of Korean adults in the late 1990s: Survey data of 70,347 health screenees. Korean J Gastroenterol. 1999. 33:642–652.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download