Abstract
We studied the seroprevalence of HBsAg, anti-HBs and anti-HBc and the vaccination histories among health care workers (HCWs) at a large suburban referral hospital in Korea. The purpose of this study was to determine the immune status of HCWs against hepatitis B virus and we also wanted to prepare a practical guideline to protect HCWs from occupational exposure. During December, 2003, 571 HCWs (56 physicians, 289 nurses, 113 technicians and 113 aid-nurses) aged between 21 and 74 yr were included in the surveillance. The positive rates of HBsAg and anti-HBs were 2.4% (14/571) and 76.9% (439/571), respectively. The positive rate of anti-HBs was lower in the physician group, and this was associated with the male gender and older age. Of the 439 anti-HBs positive cases, 320 cases (73.1%) were anti-HBc negative and this was significantly associated with a past history of HBV vaccination. The distribution of the anti-HBs levels was not associated with age (except for HCWs in their sixties), gender or occupation. Our study revealed that the seroprevalence rates of HBsAg and anti-HBs in HCWs in Korea were not different from those of the general population. Based on this surveillance, we can make reasonable decisions in case of occupational exposure to hepatitis B virus.
Hepatitis B virus (HBV) infection is highly prevalent in Africa and Asia, and in the different countries, the infection rate ranges from 5% to 20%. In Korea, its prevalence has been decreasing since the HBV vaccination was introduced about 20 yr ago. Nevertheless, HBV infection still ranges from 2 to 8.9% (2-12), which is higher than in the United States and Western Europe (1). Health care workers (HCWs) in Korea are at risk for getting an infection with HBV; therefore, HBV vaccination has been strongly recommended for them. However, studies on the HBV markers for HCWs in Korea are rare. This study was initiated to determine the seroprevalence of HBsAg, anti-HBs and anti-HBc in HCWs in Korea. This study was approved by the institutional review board at our hospital.
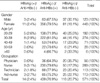
The study was performed at Sanggye Paik Hospital, which is a 700-bed university-affiliated tertiary hospital located in the northeast section of Seoul. Of the 725 HCWs working at the hospital in December, 2003, 571 of them participated in a cross-sectional HBV viral marker study and they replied to the surveillance questionnaires we gave them about their previous HBV vaccinations. The participant distributions according to age, sex and occupations are listed in Table 1. Of the 571 HCWs (123 males and 448 females), 289 (50.6%) were nurses and 466 (81.6%) were under 40 yr of age. The compliance rates according to the occupation were 33.7% (56/166) for physicians, 99.7% (289/290) for nurses, 79.6% (113/142) for aid-nurses and 89.0% (113/127) for technicians; the total compliance rate was 78.8%. Anyone inoculated at least once was classified as the vaccinated group: according to the number of doses, they were divided into the complete (3 or more) and incomplete (1 or 2) vaccinated groups.
A total of 571 samples were tested for HBsAg and anti-HBs with using electrochemiluminescence immunoassay (Elecsys 2010, Roche, Mannheim, German). Samples with a cutoff index greater than or equal to 1.0 were considered positive for HBsAg, and 10 mIU/mL was set as the minimal protective level (positive) of anti-HBs. For the tests for anti-HBc with using a chemiluminescence enzyme immunoassay (ADVIA, Centaur, Bayer, Tarry town, NY, U.S.A.), the specimens with index values greater than 1.0 were considered positive.
All statistical analysis was done using SPSS for Window software, version 11.5.
The overall positive rates of HBsAg and anti-HBs were 2.4% (14/571) and 76.9% (439/571), respectively (Table 2, 3). A number of HBsAg and anti-HBs co-negative cases were 118 (20.7%). The positive rates of HBsAg among the male and female groups were the same (2.4%); however, the positive rate of anti-HBs was higher in the females (79.5%) than in the males (67.5%) (odds ratio: 0.43, p value: 0.003 by chi-square test). According to occupations, the positive rate of HBsAg was the highest in the nurse group (3.1%). The positive rate of anti-HBs was the highest in the nurse group (79.6 %) and the lowest in the physician group (64.3%). The odds ratios for the nurses, technicians and aid-nurses were slightly elevated, but this was statistically insignificant. According to age, the positive rates of both HBsAg and anti-HBs were the highest for the HCW in their thirties, and the positive rate of anti-HBs was the lowest for the HCW in their sixties (odds ratio: 1.04, p value: 0.01).
Among the 439 anti-HBs positive cases, 321 cases (73.1%) had greater than a 100 mIU/mL level of anti-HBs (Table 4). The anti-HBs titers from 100 mIU/mL to <1,000 mIU/mL had the same prevalence among all the age groups (except those workers older than 60) and all the occupational groups. The anti-HBs titers from 10 mIU/mL to <100 mIU/mL were prevalent in HCW in their sixties. The anti-HBs titers greater than 1,000 mIU/mL were prevalent in the physician and nurse groups, compared with the aid-nurse and technician groups (25% and 23.2% vs. 17.7% and 12.4%, respectively).
Of the 571 cases, only 151 cases (26.4%) showed anti-HBc positivity and 78.1% (118/151) of them were positive for anti-HBs (Table 5). Among the 420 anti-HBc negative cases, 321 cases (76.4%) were positive for anti-HBs. Therefore, in the 439 anti-HBs positive cases, the rate of infection-induced (anti-HBc positive) anti-HBs was 26.9% and the rate of vaccine-induced (anti-HBc negative) anti-HBs was 73.1%. The number of vaccine doses and the anti-HBs positive rates were significantly associated in the anti-HBc negative group (p=0.01, chi-square test). Any HBsAg positive case was not observed in the anti-HBc negative group, in contrast to the 9.3% HBsAg positive rate (14/151) in the anti-HBc positive group. In the HBsAg (-)/anti-HBs (+)/anti-HBc (-) group, there were 50 cases noted that had no vaccination history. In the anti-HBs (+)/anti-HBc (+) group, 41 cases had a history of more than 3 vaccine doses, and 4 of them even showed to be positive for HBsAg.
The prevalence rate of HBsAg in Korea is known to be about 2-8.9%, and this rate has decreased in the past 20 yr since HBV vaccination was introduced (2-12). The positive rate for HBsAg in our study is 2.4%. A study carried out in 2003 revealed that the prevalence rates of HBsAg in Korea showed a decreasing tendency from 1.9% in adults to 0.2-0.3% in elementary school children (5). Therefore, the positive rate in our study showed results similar to the study done in 2003. Several studies have been performed in the moderate HBV-endemic areas, and they reported the HBV prevalence in HCWs as ranging from 2.8% to 9.7% (13-15). The overall anti-HBs positive rate in the present study was 76.9%, and it was similar to the anti-HBs positive rate in the general Korean population (2-4, 7).
The compliance rate of our surveillance was 78.8%. However, it varied according to the occupation (33.7-99.7%) and it was lowest in the physicians group (33.7%). The main reason for this might be that the physicians were 'too busy to participate in a study' as was observed in another study (16). The physician group showed the lowest anti-HBs positive rate among the occupational groups. Possibly the higher HBsAg (-)/anti-HBs (-) rate was due to the relatively older age distribution than was seen for the other groups. In the physician group, 48.2% were older than 40 yr of age and only 63% of them was anti-HBs positive, which was below the overall anti-HBs rate. The positive rates of HBsAg and anti-HBs in the nurse group were the highest among the occupational groups. This suggested that the nurse group has more chances to be exposed to the needle stick injury or other infectious body fluid from patients than did the other occupational groups (17, 18), because most of these exposures occur during the disposal of used syringes and recapping (19). Subjects with anti-HBs levels above 100 mIU/mL were regarded as good responders and this titer was usually followed by long-term immunity (20-23). Persistence of anti-HBs is known to be related to the maximum antibody level (20, 21). Although our study was a cross-sectional study and the anti-HBs titers were not at the peak level after a basic course of vaccination, the subjects with a titer higher than 100 mIU/mL anti-HBs seem to be meaningful. This is because the subjects that develop higher anti-HBs titers will retain antibody for a longer period than those subjects with lower levels of antibody. It has been reported that once a level above 10 mIU/mL anti-HBs is acquired, it is unnecessary to give a booster dose even when the anti-HBs level falls below 10 mIU/mL (24).
We must consider the distribution of anti-HBs in relation to the anti-HBc and the vaccination history. Anti-HBc is a remarkable marker to differentiate vaccine-induced anti-HBs from infection-induced anti-HBs. Although no difference was found between the anti-HBc positive and negative groups for the anti-HBs positive rates, the anti-HBs in our HCWs were mainly acquired from vaccination (73.1%). In our study, the positive rate of anti-HBc was 26.4% (151/571) and the rate of the anti-HBc-alone positive cases was 3.3%. The positive rates of anti-HBc in the all the study cases/anti-HBc-alone in Korea have been variably reported; 55.8/19% in 1985 (2), 24.9/1.9% in 1997 (3) and 57.2/5.1% in 2000 (4). The subjects of the studies done in 1985 and 2000 were mainly adults who were aged more than 40 yr old. However, those subjects in the 1997 study and in our study included more of the younger generation Koreans who were in their twenties and thirties. A study done in 1994 (25) showed similar anti-HBs positive rates between the vaccinated and non-vaccinated groups, but another study done in 2000 revealed a higher anti-HBs positive rate in the vaccinated group in Korea (4). A study done in the South Africa revealed that the anti-HBs positive rate in HCWs was 36.6% and only 21.2% of them had a history of past immunization against HBV (26). The anti-HBs seropositivity in Turkish HCWs was reported as 68.4% (13). The seroprevalence of anti-HBc was reported as 32% in Yemen HCWs (27). Therefore, the seroprevalence rates of HBsAg and anti-HBs in Korean HCWs were similar with the prevalence rates in the general Korean population, but the Korean HCWs had lower HBsAg rates and higher anti-HB rates than did the HCWs in the HBV endemic Korea.
Out of 571 cases, 532 cases replied to the questionnaires about HBV vaccination and 74.1% (394/532) of them had previous vaccination histories (206 complete and 188 incomplete). However, 19.8% (78/394) of the vaccinated cases were anti-HBc positive and incomplete vaccination might be one of the reasons for this. Some Korean adults might have taken a HBV vaccination dose during a latent period or a window period after their HBV infections. They even had a vaccination dose after the acquisition of infection-induced anti-HBs with or without a HBV viral maker study for the booster doses. The 50 cases showing HBsAg (-)/anti-HBs (+)/anti-HBc (-)/vaccination (-) results could not be explained well. Incorrect memories or unreliable answers to the surveillance questionnaires about their vaccinations could be the reason. The vaccination done in childhood could be a reason for their incorrect memories. Such results were also observed in other study, in which 10.2% of HBsAg (-)/anti-HBs (+)/anti-HBc (-) cases had no previous vaccination histories (4).
In conclusion, 76.9% of HCWs in a Korean hospital were positive for anti-HBs and 73.1% of them had an anti-HBs level of more than 100 mIU/mL, which suggests long lasting immunity. About 25% of HCWs may need vaccination against HBV infection in case of HBV exposure, such as could happen with a needle stick injury (28).
Figures and Tables
References
1. Zou S, Dodd RY, Stramer SL, Strong DM. Tissue Safety Study Group. Probability of viremia with HBV, HCV, HIV and HTLV among tissue donors in the United States. N Engl J Med. 2004. 351:751–759.

2. Kim YS, Kim JS, Huh BY. A study on hepatitis B virus markers and formation of anti-HBs after hepatitis B vaccination in healthy Korean population. Korean J Epidemiol. 1985. 7:8–15.
3. Oh DJ, Hwang YS, Choi JM, Min TH. A study on ALT levels in hepatitis marker positive donors-Anti-HBc positive rate in blood donors. Korean J Blood Transfus. 1997. 8:9–17.
4. Shin BM, Jeong KW. Distribution of anti-HBs levels in Korean adults. Yonsei Med J. 2000. 41:40–48.

5. Kang YJ, Chi SH. An analysis of major health factors of elementary, middle and high school students in Seoul. 2003 Yearb of School Health. 2003. 33:114–133.
6. Kang HS, Song BC, Ji CX, Kim SY, Kim SK. Serologic markers of hepatitis B virus in pregnant women in Jeju Island. Korean J Hepatol. 2004. 10:191–196.
7. Ju YH, Shin HR, Oh JK, Kim DI, Lee DH, Kim BK, Kim JI, Jung KY. A seroepidemiological study of hepatitis B and C virus (HBV and HCV) infections in the young population in parts of Busan, Korea. Korean J Prev Med Public Health. 2004. 37:253–259.
8. Kim DS, Kim YS, Kim JY, Ahn YO. A study on the seropositivity of HBsAg among biennial health examinees: a nation-wide multicenter survey. Korean J Prev Med. 2002. 35:129–135.
9. Lee DH, Kim JH, Nam JJ, Kim HR, Shin HR. Epidemiological findings of hepatitis B infection based on 1998 National Health and Nutrition Survey in Korea. J Korean Med Sci. 2002. 17:457–462.

10. Park KS, Lee YS, Lee SG, Hwang JY, Chung WJ, Cho KB, Hwang JS, Ahn SH, Park SK. A study on markers of viral hepatitis in adults living in Daegu and Gyungbuk area. Korean J Gastroenterol. 2003. 41:473–479.
11. Jang MK, Lee JY, Lee JH, Kim YB, Kim HY, Lee MS, Park CK, Yoo JY. Seroepidemiology of HBV infection in South Korea, 1995 through 1999. Korean J Intern Med. 2001. 16:153–159.
12. Joo KR, Bang SJ, Song BC, Youn KH, Joo YH, Yang S, Kim KR, Chung YH, Lee YS, Suh DJ. Hepatitis B viral markers of Korean adults in the late 1990s: survey data of 70,347 health screenees. Korean J Gastroenterol. 1999. 33:642–652.
13. Ozsoy MF, Oncul O, Cavuslu S, Erdemoglu A, Emekdas G, Pahsa A. Seroprevalences of hepatitis B and C among health care workers in Turkey. J Viral Hepatitis. 2003. 10:150–156.

14. Hizel K, Sengul A, Emekdas G, Senol E, Inal A. Hastane personelinde Hepatit B seroprevalansi ve rekombinant hepatit B asisina immune cevap. Viral Hepatit Derg. 1998. 4:25–27.
15. Pamukcu M, Mutlu G, Yegin O. Hastane personelinde hepatit B virus markerlerinin prevalansi. Turkish J Infect. 1990. 4:149–157.
16. Cheong HJ, Sohn JW, Choi SJ, Eom JS, Woo HJ, Chun BC, Kim WJ, Park SC. Factors influencing decision regarding influenza vaccination: a survey of healthcare workers in one hospital. Infect Chemother. 2004. 36:213–218.
17. West DJ. The risk of hepatitis B infection among health professionals in the United States; a review. Am J Med Sci. 1984. 287:26–33.

18. Gerberding JL. Incidence and prevalence of human immunodeficiency virus, hepatitis B virus, hepatitis C virus and cytomegalovirus among health care personnel at risk for blood exposure. Final report from a longitudinal study. J Infect Dis. 1994. 170:1410–1417.

19. Hofmann F, Kralj N, Beie M. Needle stick injuries in health care-frequency, causes and preventive strategies. Gesundheitswesen. 2002. 64:259–266.
20. Ambrosch F, Frisch-Niggemeyer W, Kremsner P, Kunz C, Andre F, Safary A, Wiedermann G. Persistence of vaccine induced antibodies to hepatitis B surface antigen and the need for booster vaccination in adult subjects. Postgrad Med J. 1987. 63:Suppl 2. 129–135.
21. Zuckerman JN. Nonresponse to hepatitis B vaccines and the kinetics of anti-HBs production. J Med Virol. 1996. 50:283–288.

22. Ambrosch F, Courouce AM, Coursaget P, Deinhardt F, Desmyter J, Frei PC. Immunization against hepatitis B. Lancet. 1988. 1:875–876.
23. Jilg W, Schmidt M, Deinhardt F. Immune response to hepatitis B revaccination. J Med Virol. 1988. 24:377–384.

24. West DJ, Galandra GB. Vaccine induced immunologic memory for hepatitis B surface antigen: implications for policy on booster vaccination. Vaccine. 1996. 14:1019–1027.

25. Park NH, Lee JB, Kim YS. The vaccination rate of hepatitis B vaccine among Korean adults. J Korean Acad Fam Med. 1994. 15:191–198.
26. Vardas E, Ross MH, Sharp G, McAnerney J, Sim J. Viral hepatitis in South African healthcare workers at increased risk of occupational exposure to blood-borne viruses. J Hosp Infect. 2002. 50:6–12.

27. Shidrawi R, Ali-Huraibi MA, Ali-Haimi MA, Dayton R, Murray-Lyon IM. Seroprevalence of markers of viral hepatitis in Yemeni Healthcare workers. J Med Virol. 2004. 73:562–565.

28. Rodriguez C, Castilla J, del Romero J, Lillo A, Puig ME, Garcia S. Prevalence of hepatitis B virus infection and needs of vaccination in high risk populations. Med Clin (Barc). 2003. 121:697–699.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download