Abstract
Infertile women with chronic anovulation are prone to be exposed to unopposed estrogen stimulation and have the high risk of being suffering from endometrial hyperplasia or even endometrial carcinoma. A few reports have suggested that nulliparous young women (under 40 yr of age) with endometrial carcinoma could be treated conservatively to preserve fertility and succeed the live birth. We report on a 36-yr-old woman who received conservative treatment of endometrial carcinoma (stage I, grade 1) by curettage and progestin. After megestrol medication of total 71,680 mg during 24 weeks, we found the regression of endometrial lesion by curettage and hysteroscopic examination. Then we decided to perform in vitro fertilization program. Two embryos were transferred and heterotypic pregnancy was diagnosed 27 days after embryo transfer. After right salpingectomy, she received routine obstetrical care and delivered by cesarean section at 38 weeks in gestational periods. Two years after delivery, she is healthy without any evidence of recurrent disease. The fertility preserving treatment is an option in endometrial cancer patients if carefully selected, and assisted reproductive technologies would be helpful.
Endometrial carcinoma is the most common malignant tumor of the female genital tract in western country. Many patients with endometrial carcinoma are in their 50's and only 5% of them are under age 40 (1). Endometrial adenocarcinoma in child bearing age is relatively uncommon, except in those with obesity, chronic anovulation, irregular menstruation, infertility and is associated with so-called polycystic ovary syndrome or estrogen producing tumor. Prolonged unopposed estrogen exposure in infertile women with chronic anovulation may induce endometrial hyperplasia progressing to carcinoma. Failure of ovulation, characteristically expressed with amenorrhea or oligomenorrhea, occurred in 21% of infertile patients, ovulatory dysfunction cause subfertility in 15-20% of couples (2). The risk of endometrial carcinoma was increased 4.8-folds in infertile patients and 10.3-folds in infertile women with chronic anovulation (3). So it is essential to evaluate the endometrial disease thoroughly during infertility work up in these patients (4,5).
Most patients with endometrial carcinoma undergo hysterectomy, however, in a young woman who wishes to bear a child, trial treatment with progestins has been attempted, and successful pregnancies after the conservative treatment have been reported. Endometrial cancer in younger patients (age under the 40 yr) is generally associated with a better prognosis because the tumors are detected at an early stage and likely to be highly differentiated and hormonally dependent. In such a setting, high dose progestins followed by curettage may be the alternative treatment in patients who wish to preserve fertility.
We report a case of successful live birth through the in vitro fertilization (IVF) program after conservative treatment of endometrial cancer (stage I, grade I).
A 36-yr-old woman visited in our infertility clinic, complaining of primary infertility for 1 yr. Her menstrual cycle was irregular, about 60-120 days, body mass index was 27.5 (body weight: 73 kg, height: 163 cm). She had a history of explo-laparotomy due to endometriosis. Neither she nor any other members of her family had diabetes or hypertension. Abdomino-pelvic examination showed the unremarkable findings and transvaginal ultrasonogram showed small uterine myoma, 24-21 mm, normal contour of endometrium, 10 mm, and well defined normal both ovaries. Full infertility work up was performed, results of semen analysis was normal, hormonal study (LH, FSH, Estradiol, Prolactin, TSH, Testosterone, DHEA-S) showed normal findings except high FSH level of 9.66 mIU/mL. The office endometrial aspiration biopsy showed secretory phase and finding of luteal phase defect. Hysterosalpingogram revealed one point filling defect in the uterine cavity and mild dilatation of ampullary portion of Fallopian tubes, but good intraperitoneal spillage (Fig. 1A). On laparoscopic examination, peritubal adhesion was detected and adhesiolysis was performed. On hysteroscopic examination, there was a polypoid mass on fundal area and hysteroscopic biopsy and curettage was done. The pathologic evaluation of endometrial tissue revealed well differentiated endometrial adenocarcinoma (Grade 1, Fig. 2A) with positive estrogen and progesterone receptors. After curettage, we confirmed that there was no detectable endometrial mass or myometrial invasion or cervical involvement by MRI imaging (Fig. 1B). Final diagnosis was primary infertility accompanying endometrial carcinoma, FIGO grade I without myometrial invasion.
After counseling, the patient wished to retain her ability to conceive, so high dose progestin therapy was recommended. Oral megestrol acetate was prescribed 600 mg daily for 8 weeks. On follow-up hysteroscopic examination, she still got a small protruding mass on fundal area. We performed hysteroscopic biopsy and endometrial curettage. The pathologic evaluation of endometrium revealed complex hyperplasia without cellular atypia (Fig. 2B). She continued to receive megestrol acetate but complained intolerable weight gain from 73 to 88 kg. We decided to reduce the dose to 400 mg, daily for 4 weeks, then 320 mg, daily for 12 weeks. After megestrol medication of total 71,680 mg during 24 weeks, we found smooth atrophic endometrium by hysteroscopic examination, and this was confirmed as atrophic endometrium through the histological examination of tissue obtained by curettage. Then we decided to perform IVF program in order to optimize the patient's potential for fertility and achieve a viable pregnancy without further delay.
After pituitary down-regulation by the GnRHa (Buserelin acetate, Superfact®, Hoechst), follicle-stimulating hormone preparation (Follimon®, LGIC, Korea) was administrated, 375 IU daily for 12 days. The follicular growth was monitored from gonadotropin day 5 by 3 days interval and human chorionic gonadotropin (IVF-C®, LGIC, Korea) 10,000 IU was administrated when the at least 3 or more follicles reached 18 mm in diameter. And 35 hr later, oocytes aspiration was performed under the guidance of transvaginal ultrasonography. Two mature oocytes were retrieved and inseminated with her husband's prepared spermatozoa. Fifty seven hours after oocyte retrieval, the two high grade 4-cell embryos were transferred. Measurement of β-hCG revealed 3,449 mIU/mL on 19 days after embryo transfer, and on 23 days after embryo transfer, intrauterine single gestational sac with yolk sac and right tubal pregnancy were identified by transvaginal ultrasonogram. Right salpingectomy was performed under the epidural anesthesia, on 27 days after embryo transfer, we could detect the fetal pole with heart beat in the intrauterine gestational sac after that procedure. Then she received routine obstetrical care and delivered by Cesarean section at 38 weeks in gestational periods. The baby was female, 2,590 g, and the Apgar score was 8 at 1 min, 9 at 5 min. Placenta was grossly and microscopically normal, there was no evidence of residual tumor in the uterus and adnexa or abdominal organ.
Twelve weeks after delivery, endometrial thickness measured by transvaginal ultrasonography was 4 mm and endometrial biopsy revealed no evidence of recurrent disease. Two years after delivery, she was healthy without any evidence of recurrent disease.
Endometrial carcinoma is the most common malignant tumor of the female genital tract in western country. But in Korea, endometrial carcinoma is the third frequent malignant tumor of the female genital tract (10.4% of the female genital tract) and only 13.5% of them are under age 40 yr, but its incidence has been increasing steadily.
The standard therapy for endometrial carcinoma is staging laparotomy with total abdominal hysterectomy and bilateral salpingo-oophorectomy, followed by adjuvant radiation for patients judged to be at high risk for local recurrence. Several lines of evidence have suggested that two different pathogenic types of endometrial cancers exist according to hyperestrogenic state or not. The type of endometrial cancer associated with hyperestrogenism typically develops via a characteristic sequence from hyperplastic lesion of the endometrium to premalignant lesion, finally invasive cancer and has tendency to be diagnosed in early stage, as low grade, with estrogen and progesterone receptors (6). In such a setting, conservative treatment with progestin may be the alternative treatment modality in patient who wishes to preserve fertility (7).
In a case of series, three of eight patients with grade 1 adenocarcinoma, limited to the endometrium, were successfully treated with progesterone followed by dilatation and curettage (8). A review of the pathology records at Johns Hopkins Medical Center between 1990 and 1996 yield 12 patients younger than 40 yr of age who had well-differentiated adenocarcinoma of the endometrium were treated with progestin alone for 3 to 18 months. Nine of 12 patients had regression of lesion and remained free of disease at a mean follow up duration of 40 months (9). Kim et al. also reported that progestin treatment for well-differentiated adenocarcinoma in young women was successful in 13 out of 20 cases (10).
But no consensus exists about specific conservative treatment for well-differentiated endometrial cancer, that is, the dose and duration of progestins treatment have not yet been established. The reported daily doses of progestins were variable, from 40 mg to 400 mg of megestrol acetate or 200 mg to 600 mg of medroxyprogesterone acetate, and the durations of medication were from 3 months to 18 months (9-13).
The conservative therapy has apparent risks and some investigators have strongly opposed to use conservative treatment because the treatment with progestins may not always achieve remission (14). The risk of disease progression occurring during or after progestin therapy would be approximately 5% (8), while Randall and Kurman did not experience the patients with progressive disease except patients with persistent lesions (9).
Before the decision of conservative treatment, it is prerequisite to know the depth of myometrial invasion and grade of tumor cells, that is, conservative treatment is indicated only in the case of well-differentiated, early stage disease without extrauterine lesions. For these purposes, MRI would be helpful for evaluation of invasion depth of tumor and detecting extrauterine tumor and the endometrial biopsy should be performed for grading of tumor. There were several reports about inaccuracy of endometrial biopsy, incorrect diagnoses of 28 percents were reported with office Novak curette biopsy with 18% having a higher grade tumor in hysterectomy (15), although the dilatation and curettage was more accurate than office endometrial biopsy in predicting tumor grade, the dilatation and curettage also incorrectly graded approximately 25% of the patients, with higher grade tumor being missed in about 10% (16). For the reduction of misdiagnosis, as additional diagnostic tool, hysteroscopic examination such as in our case would be helpful.
After the conservative treatment of endometrial carcinoma, the pregnancy rate was somewhat disappointing, that is, only 3 of 24 patients delivered viable infants (10). To permit subsequent pregnancy as well as to prevent the recurrence of disease, it is important to induce ovulation following regression of carcinoma. Given the high incidence of chronic anovulation and infertility in young women with endometrial carcinoma, it is likely that trial of assisted reproductive technologies would have resulted in a higher pregnancy rate. Kimmig et al. reported successful pregnancy achieved by gamete intrafallopian transfer and Pinto et al. reported successful pregnancy through the in vitro fertilization after controlled overian hyperstimulation and recently Lowe et al. reported successful pregnancy through the oocyte donation program (7,11,17).
This is another report of conservative treatment of endometrial carcinoma followed by successful pregnancy through the IVF program. We believe that hysteroscopic examination during the infertility work up would be helpful not only in the evaluation of abnormal findings of hysterosalpingography but also of endometrial pathology in patients with highly suspicion of endometrial disease due to prolonged unopposed estrogen exposure.
We prescribed initially megestrol acetate, 600 mg daily that was the highest dose of progestins ever reported, and observed the regression of the endometrial carcinoma through the complex hyperplasia without cellular atypia to atrophic endometrim. And we agree with Kimmig et al. in that progestin treatment should be followed immediately by downregulatory therapy with GnRHa in order to prevent reinduction of the menstrual cycles and unnecessary prolonged exposure to estrogens, and assisted reproductive technologies would be helpful in women who wish to conceive.
In conclusion, we report a case of successful live birth through the IVF program after conservative treatment of endometrial cancer (stage I, grade 1). The fertility-preserving treatment is an option in endometrial cancer patients if carefully selected, and assisted reproductive technologies would be helpful.
Figures and Tables
Fig. 1
(A) Hysterosalpingogram shows a small filling defect in the uterine cavity. (B and C) MRI reveals no residual tumor in the endometrium nor myometrial involvement after curettage.
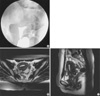
Fig. 2
(A) A well-differentiated endometrioid adenocarcinoma. Light micrograph shows anaplastic proliferation of the endometrial glands associated with foci of squamoid differentiation (H&E stain, ×200). (B) After progestin therapy for 8 weeks, the endometrium shows complex hyperplasia without nuclear atypia in the dilated endometrial glands (H&E stain, ×200).

References
1. Ostor AG, Adam R, Gutteridge BH, Fortune DW. Endometrial carcinoma in young women. Aust N Z J Obstet Gynecol. 1982. 22:38–42.

2. Hull MG, Glazener CM, Kelly NJ, Conway DI, Foster PA, Hinton RA, Coulson C, Lambert PA, Watt EM, Desai KM. Population study of causes, treatment, and outcome of infertility. Br Med J. 1985. 291:1693–1697.

3. Ron E, Lunenfeld B, Menczer J, Blumstein T, Katz L, Oelsner G, Serr D. Cancer incidence in a cohort of infertile women. Am J Epidemiol. 1987. 125:780–790.

4. Meirow D, Schenker JG. The link between female infertility and cancer: epidemiology and possible aetiologies. Hum Reprod Update. 1996. 2:63–75.

5. Salha O, Martin-Hirsch P, Lane G, Sharma V. Endometrial carcinoma in a young patient with polycystic ovarian syndrome: first suspected at time of embryo transfer. Hum Reprod. 1997. 12:959–962.

6. Emons G, Heyl W. Hormonal treatment of endometrial cancer. J Cancer Res Clin Oncol. 2000. 126:619–623.

7. Lowe MP, Bender D, Sood AK, Davis W, Syrop CH, Sorosky JI. Two successful pregnancies after conservative treatment of endometrial cancer and assisted reproduction. Fertil Steril. 2002. 77:188–189.

8. Farhi DC, Nosanchuk J, Silverberg SG. Endometrial adenocarcinoma in women under 25 years of age. Obstet Gynecol. 1986. 68:741–745.

9. Randall TC, Kurman RJ. Progestin treatment of atypical hyperplasia and well differentiated carcinoma of the endometrium in women under age 40. Obstet Gynecol. 1997. 90:434–440.
10. Kim YB, Holschneider CH, Ghosh K, Nieberg RK, Montz FJ. Progestin alone as primary treatment of endometrial carcinoma in premenopausal women. Cancer. 1997. 79:320–327.

11. Kimmig R, Strowitzki T, Muller-Hocker J, Kurzl R, Korell M, Hepp H. Conservative treatment of endometrial cancer permitting subsequent triplet pregnancy. Gynecol Oncol. 1995. 58:255–257.

12. Mitsushita J, Toki T, Kato K, Fujii S, Konishi I. Endometrial carcinoma remaining after term pregnancy following conservative treatment with medroxyprogesterone acetate. Gynecol Oncol. 2000. 79:129–132.

13. Jobo T, Imai M, Kawaguchi M, Kenmochi M, Kuramoto H. Successful conservative treatment of endometrial carcinoma permitting subsequent pregnancy: report of two cases. Eur J Gynaecol Oncol. 2000. 21:119–122.
14. Greenblatt RB, Gambrell RD Jr, Stoddard LD. The protective role of progesterone in the prevention of endometrial cancer. Pathol Res Pract. 1982. 174:297–318.

15. Daniel AG, Peters WA. Accuracy of office and operating room curettage in the grading of endometrial carcinoma. Obstet Gynecol. 1988. 71:612–614.
16. Larson DM, Johnson KK, Broste SK, Krawisz BR, Kresl JJ. Comparison of D&C and office endometrial biopsy in predicting final histopathologic grade in endometrial cancer. Obstet Gynecol. 1995. 86:38–42.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download