Abstract
Granulocytic sarcoma is a rare extramedullary tumor composed of myeloid progenitor cells. Primary involvement of the biliary tract without evidence of leukemia is exceedingly rare. Here, we report an isolated biliary granulocytic sarcoma in a 30-yr-old man who presented with jaundice, fever, and chill without any evidence of leukemia. However, five months after the diagnosis, he developed acute myelogenous leukemia with multilineage dysplasia and chromosomal abnormality. A rare possibility of biliary granulocytic sarcoma should be considered as a differential diagnosis in patients with obstructive jaundice. A histologic evaluation by aggressive diagnostic intervention is important and may improve prognosis.
Granulocytic sarcoma is an extramedullary collection of myeloblasts. It was first described by Burns (1) in 1811, and named "chloroma" by King (2) in 1853 because of its green color, which is due to the presence of myeloperoxidase enzymes in the immature myeloid cells. Rappaport first used the term "granulocytic sarcoma" in 1966 (3). This disease usually arises during the course of acute myelogeneous leukemia, although it also occurs infrequently in chronic myelogeneous leukemia and other myeloproliferative disorders. The most common sites of involvement are the periosteum, soft tissue, bone, lymph nodes, and skin, but almost any site may be involved, e.g., the brain, breasts, urinary bladder, and gastrointestinal tract, and multiple organ involvement is also common (4). However, isolated granulocytic sarcoma in the biliary tract without evidence of leukemia is exceedingly rare.
Here, we describe a case of granulocytic sarcoma of the proximal common bile duct, and right and left hepatic ducts causing obstructive jaundice in a patient without evidence of bone marrow disease; this was followed by acute myelogeneous leukemia with multilineage dysplasia.
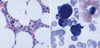
A 30-yr-old man was admitted to our hospital because of jaundice and mild fever with a chill. The patient had been well until 3 months earlier, when he began to develop right upper quadrant pain. One month before admission, the pain worsened and at times radiated into his back. On admission, a physical examination was unremarkable except for icteric sclera. An abdominal examination revealed right upper quadrant tenderness but did not disclose hepatosplenomegaly or a palpable mass. Laboratory tests on admission showed elevated total bilirubin (6.9 mg/dL; normal range 0-0.5), serum aspartate aminotransferase (201 µ/L; normal range 0-40), serum alanine aminotransferase (814 mg/dL; normal range 0-40), and alkaline phosphatase (158 µ/L; normal range 53-128). Complete blood cell counts were within normal limits, with no blast cells. Ultrasonography (US) revealed thickening of the gallbladder wall and multiple tiny stones with some sludge in the gallbladder. Endoscopic retrograde cholangiopancreatography (ERCP) revealed bile duct strictures (Fig. 1). Endoscopic nasobiliary drainage (ENBD) was performed using a 5-Fr. plastic stent. Abdominal computed tomography after ENBD disclosed a low density rim around the ENBD tube, but no definitive abnormal enhancing lesion of the wall or mass was recognized (Fig. 2). The jaundice was temporally relieved after ENBD and the patient received open cholecystectomy under the impression of cholelithiasis with bile duct stricture. The histologic diagnosis of the gallbladder was chronic cholecystitis with cholelithiasis. Because jaundice had not resolved after cholecystectomy, right lobectomy with hepaticojejunostomy was performed. During the operation a diffuse stricture from the middle common bile duct extending to right and left hepatic ducts with wall thickening was observed. A pathologic examination showed a monomorphous and discohesive infiltration of tumor cells along the bile duct wall (Fig. 3A, B). Tumor cells were of medium size with large nuclei showing dispersed chromatin, and one or more distinct but not prominent nucleoli. The cytoplasm was deeply eosinophilic and granular reminiscent of metamyelocytes, and indicative of myeloid differentiation (Fig. 3B). Immunohistochemistry showed positivity for myeloperoxidase (1: 20,000, Dako, Denmark)(Fig. 3C), CD34 (1:100, Dako, Denmark), and lysozyme (1:100, Zymed, New Zealand) but negativity for CD3 (1:200, Novocastra, U.K.) and CD20 (1:500, Novocastra, U.K.). The liver was not involved by the tumor. The histologic diagnosis was granulocytic sarcoma involving the right and left hepatic ducts, superior bile duct, and cystic duct. A bone marrow biopsy taken at the time was normal, and the patient had no symptoms or signs of leukemia. The patient was then followed without other therapies such as chemotherapy or radiotherapy. Five months after the initial diagnosis of granlocytic sarcoma, peripheral blood smear showed normochromic normocytic anemia (Hb 11.4 g/dL, Hct 33.1%) with aniso- and poikilo-cytosis, neutropenia (3,700/µL) with 10% blasts, and thrombocytopenia (73,000/µL) with giant forms. Bone marrow aspiration and biopsy showed leukemic blasts with abnormal nuclear folding, and cytoplasmic blebs which were counted up to 40.1% of all nucleated cells and infiltrated between normal and dyshematopoietic erythoid and myeloid cells(Fig. 4). Those blasts were positive for myeloperoxidase, Sudan-black B, and peroxidase in cytochemical stain and expressed CD13, CD33, myeloperoxidase, and CD34 in flow cytometric analysis. Megakaryocytes with dysplasia were hardly observed in aspiration smear but increased in number in biopsy. A diagnosis of acute myelogeneous leukemia with multilineage dysplasia was made according to the WHO classification or M2 by the French-American-British (FAB) classification. A chromosomal study showed 45,XY,del(3)(q21q27),-16,add (21)(q22) [18]/46,XY[2]. The patient received induction chemotherapy with idarubicin and cytarabine. A follow up bone marrow examination 21 days after the induction chemotherapy showed persistent acute myelogenous leukemia (AML) with multilineage dysplasia (Blasts: up to 4.3% of all nucleated cells).
Granulocytic sarcoma usually occurs in one of the following three clinical settings. The first is in patients with previous or current AML, and the second in patients as a sign of blast transformation of CML or of some other chronic myeloproliferative disorder. Third setting is in patients with no other clinical evidence of hematologic disease at the time of diagnosis. Neiman et al. (5) reported 61 patients with granulocytic sarcoma, in which 48% of the cases were associated with myeloproliferative disorder, 30% presented with no overt leukemia, and 22% occurred as the initial presentation or during the course of AML. The most common sites of involvement were the periosteum, soft tissue and bone followed by the lymph nodes and skin, however it may be found in any location including gingiva, pancreas, breast, testis, spinal cord, or ovary (5-13).
Isolated biliary involvement by granulocytic sarcoma is extremely rare. Only four cases of biliary granulocytic sarcoma have been reported in the English literature (Table 1). The first case (14) was presented with a sign of AML relapse. The patient received chemotherapy because of AML M2 and reached complete remission. However, 29 months later, the patient developed jaundice and abdominal pain, and was diagnosed as having a granulocytic sarcoma in the common bile duct. The second case (15) was of a 45-yr-old man who underwent allogenic bone marrow transplantation (BMT) because of chronic myelogeneous leukemia in blast crisis. On day 69 after BMT, he presented with anorexia and jaundice and was diagnosed as having a granulocytic sarcoma by open biopsy. Third case (16) was of an 84-yr-old man presented with jaundice. A CT scan showed a low-density mass at the porta hepatis, and thickening of the gallbladder wall which suggests gallbladder carcinoma. Endoscopic retrograde biliary drainage was performed. Other therapies, such as laparotomy, chemotherapy, and radiotherapy were not performed because of old age. Fifty-one days after first admission, a peripheral blood examination showed a white cell count of 16,400/µL with 60% blast cells. A bone marrow examination revealed AML (FAB type M0), and he died 1 month after diagnosis. At autopsy, the suspected gallbladder carcinoma turned out to be granulocytic sarcoma associated with AML. The forth case (17) was of a 75-yr-old woman who presented with severe obstructive jaundice. A bile duct carcinoma arising in the hilum of the liver (a so-called Klatskin tumor) was clinically suspected. A right hepatectomy was performed and revealed a granulocytic sarcoma. Subsequently, a bone marrow biopsy showed acute myelomonocytic leukaemia. The patient died of disease 1 month after surgery.
The present case also presented with abdominal pain and jaundice. Likewise to the case reported by Matsueda et al. (16), the patient had no preceding leukemia. Neiman et al. (5) reported that among 15 patients of granulocytic sarcoma without leukemia, 13 patients developed AML between 1 and 49 months (mean: 10.5 months) after diagnosis. Most nonleukemic granulocytic sarcomas left untreated will progress to acute nonlymphoblastic leukemia (ANLL), and patients initially administered chemotherapy for ANLL showed longer disease free intervals and overall survival (18-20). The present patient did not receive chemotherapy until development of leukemia, which may have caused the early development of acute leukemia.
Granulocytic sarcoma occurs in only 2 to 8% of AML cases, which are mainly of the M2 morphology, although the disease has also been associated with M3, M4, M5, and M7 morphologies (21). A patient having AML type M2 with t(8;21) showed a greater tendency to develop granulocytic sarcoma than others, as demonstrated by a study which found that 4.5 to 38% of patients with t(8;21)(q22;q22) developed granulocytic sarcoma (22,23). The acute leukemia that developed in the current patient was FAB type M2 with chromosomal abnormality affecting chromosome 21(q22).
A diagnosis of biliary granulocytic sarcoma is difficult to make by radiographic examination only, and is virtually impossible in a nonleukemic patient. Biliary granulocytic sarcoma may be misdiagnosed as inflammatory lesion such as cholangitis or cholecystitis or as a malignancy. Biliary granulocytic sarcoma reported previously, and the current case commonly presented with obstructive jaundice with extrinsic bile duct compression. Therefore, biliary granulocytic sarcoma should be included in the differential diagnosis of patients with obstructive jaundice. Early diagnostic intervention with histologic evaluation is important, and may lead to a better prognosis.
Figures and Tables
Fig. 1
Endoscopic retrograde cholangiopancreatography (ERCP) reveals the common bile duct stricture.

Fig. 2
Computed tomogram discloses a low density rim around the ENBD tube, but no definitive abnormal enhancing lesion or mass is recognized.

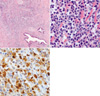
Fig. 3
Microscopic finding of bile duct shows a monomorphous and discohesive cellular infiltration along the bile duct wall (A) having medium to large nuclei with one or more distinct but not prominent nucleoli and a dispersed chromatin (H&E, ×40) (B). Tumor cells are positive for myeloperoxidase (PAP, ×400) (C).
References
1. Burns A. Observations on the surgical anatomy of the head and neck. 1811. Edinburgh: Thomas Royce;364–366.
2. King A. A case of chloroma. Monthly J Med. 1853. 17:97.
3. Rappaport H. Tumors of the hematopoietic system. Atlas of tumor pathology. 1966. Washington D.C.: Armed forces institute of pathology;241–243.
4. Meis JM, Butler JJ, Osborne BM, Manning JT. Granulocytic sarcoma in nonleukemic patients. Cancer. 1986. 58:2697–2709.

5. Neiman RS, Barcos M, Berard C, Bonner H, Mann R, Rydell RE, Bennett JM. Granulocytic sarcoma: a clinicopathologic study of 61 biopsied cases. Cancer. 1981. 48:1426–1437.

6. Mehta J, Kane S. Primary granulocytic sarcoma of ovary-a rare presentation. Leuk Lymphoma. 2004. 45:845–847.

7. Eggener SE, Abrahams A, Keeler TC. Granulocytic sarcoma of the testis. Urology. 2004. 63:584–585.

8. Servin-Abad L, Caldera H, Cardenas R, Casillas J. Granulocytic sarcoma of the pancreas. A report of one case and review of the literature. Acta Haematol. 2003. 110:188–192.
9. Antmen B, Haytac MC, Sasmaz I, Dogan MC, Ergin M, Tanyeli A. Granulocytic sarcoma of gingiva: an unusual case with aleukemic presentation. J Periodontol. 2003. 74:1514–1519.

10. Dutta Roy S, Stafford JS, Scally J, Selvachandran SN. Granulocytic sarcoma of the breast antedating acute myelogenous leukemia. Breast. 2004. 13:242–246.

11. Jordan RC, Glenn L, Treseler PA, Regezi JA. Granulocytic sarcoma: case report with an unusual presentation and review of the literature. J Oral Maxillofac Surg. 2002. 60:1206–1211.

12. Landis DM, Aboulafia DM. Granulocytic sarcoma: an unusual complication of aleukemic myeloid leukemia causing spinal cord compression. A case report and literature review. Leuk Lymphoma. 2003. 44:1753–1760.

13. King DJ, Ewen SW, Sewell HF, Dawson AA. Obstructive jaundice. An unusual presentation of granulocytic sarcoma. Cancer. 1987. 60:114–117.

14. Case records of the Massachusetts General Hospital Weekly clinicopathological exercises. Case 32-1988. Obstructive jaundice in a man with treated colon cancer and leukemia. N Engl J Med. 1988. 319:356–364.
15. Rotter AJ, O'Donnell MR, Radin DR, Marx HF. Peribiliary chloroma: a rare cause of jaundice after bone marrow transplantation. Am J Roentgenol. 1992. 158:1255–1256.

16. Matsueda K, Yamamoto H, Doi I. An autopsy case of granulocytic sarcoma of the porta hepatis causing obstructive jaundice. J Gastroenterol. 1998. 33:428–433.

17. Ascani S, Piccaluga PP, Pileri SA. Granulocytic sarcoma of main biliary ducts. Br J Haematol. 2003. 121:534.

18. Yamauchi K, Yasuda M. Comparison in treatments of nonleukemic granulocytic sarcoma: report of two cases and a review of 72 cases in the literature. Cancer. 2002. 94:1739–1746.
19. Eshghabadi M, Shojania AM, Carr I. Isolated granulocytic sarcoma: report of a case and review of the literature. J Clin Oncol. 1986. 4:912–917.

20. Imrie KR, Kovacs MJ, Selby D, Lipton J, Patterson BJ, Pantalony D, Poldre P, Ngan BY, Keating A. Isolated chloroma: the effect of early antileukemic therapy. Ann Intern Med. 1995. 123:351–353.

21. Morel F, Herry A, Le Bris MJ, Le Calvez G, Marion V, Berthou C, De Braekeleer M. Isolated granulocytic sarcoma followed by acute myelogenous leukemia type FAB-M2 associated with inversion 16 and trisomies 9 and 22. Leukemia. 2002. 16:2458–2459.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download