Abstract
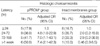
This study evaluated the risk of brain damage in neonates delivered at <34 weeks following a prolonged latency after preterm premature rupture of membranes (pPROM). The medical records of 77 singletons delivered at <34 weeks with pPROM and 66 singletons delivered at <34 weeks with preterm labor and intact membranes were reviewed. Latency was divided into four intervals: ≤24, >24-≤72, >72-≤168 hr, and >1 week. Outcomes in the longer three intervals were compared with those in neonates delivered at ≤24 hr after pPROM. The documented outcomes were placental (histologic chorioamnionitis, vasculitis, funnisitis) and neonatal (intraventricular hemorrhage, ventriculomegaly, germinal matrix hemorrhage, periventricular leukomalacia). Odds ratios and 95% CI for the risk of histologic chorioamnionitis according to the respective latency intervals were 4.8 (1.0-22.9), 7.0 (1.1-43.1), 7.4 (2.1-42.3) in patients with pPROM. The risks of intracranial ultrasonic abnormalities, however, did not increased with prolonged latency. In the patients with preterm labor and intact membranes, the both risks did not increased with increasing latency. Therefore, this study was suggested that the risk of histologic chorioamnionitis increased with increasing latency, but there was no relationship between neonatal brain damage and latency interval after pPROM.
The premature rupture of membranes is a common event, and during the preterm period, it occurred in 1% of all pregnancies. Despite recent advances in perinatal care, preterm premature rupture of membranes (pPROM) continues to lead to important obstetric complications (1). The frequency and severity of neonatal complications after pPROM vary with the gestational age at which rupture and delivery occur. In particular, the risk of complications increases with decreasing gestational age at membrane rupture and delivery (2). Moreover, the optimal management of pPROM is uncertain and many controversies remain (3).
The risks of immediate delivery include the major sequelae of prematurity, such as, hyaline membrane disease and intracranial hemorrhage. Latency is an important factor for neonatal survival in these patients. However, these patients face several factors that lead fetal morbidity and mortality. Amnionitis, advanced labor, and nonreassuring fetal status usually force the clinician to affect delivery despite fetal immaturity. And, it has been reported that histologic chorioamnionitis is the one of the various causes of neonatal brain damage, such as, intraventricular hemorrhage (IVH) and germinal matrix hemorrhage (GMH) (4-6). Chorioamnionitis or intrauterine fetal infection has been recognized in humans and animal models as possible precursors to fetal cerebral injury (7,8).
In 1993, Leviton (9) hypothesized that intrauterine infection activates the fetal production of proinflammatory cytokines (TNF, IL-6), which subsequently contribute to perinatal injury, including white matter damage and periventricular leukomalacia. Several years later, Yoon et al. (10) and Gomez et al. (11) supported this hypothesis by reporting a significant association between umbilical cord plasma IL-6 concentrations and IVH and periventricular leukomalacia. Thus, the intensity of intrauterine infection appears to increase with increasing latency (12,13), conservative treatment might potentiate neurologic damage. To evaluate this hypothesis, we assessed the relationship among latency interval, the risks of histologic chorioamnionitis and neonatal brain damage.
Between January 1998 and March 2003, the medical records of 115 singletons delivered prior to 34 weeks and complicated by pPROM and of 251 singletons delivered prior to 34 weeks complicated with preterm labor but with intact membranes were reviewed at the Samsung Cheil Hospital in Seoul, Korea. Patients without results of placental pathology and neonatal cranial ultrasound results and those with placental abruption and preeclampsia were excluded. Accordingly, 77 mothers and neonates for pPROM group and 66 mothers and neonates for preterm labor with intact membranes met the entry criteria. This study was approved by institutional review board.
The term "latency" refers to the time between membrane rupture and delivery (2). However, in this study, we considered that pregnant women that did not remember the accurate time of rupture. So, latency was defined as the time from arrival at delivery room to delivery. The latency was divided into four clinically relevant intervals: ≤24, >24-≤72, >72-≤168 hr, and >1 week, which correlated with steroid therapy to reduce respiratory distress syndrome. This was also applied to intact membranes group.
PROM was diagnosed by a sterile speculum examination with a combination of vaginal pooling, nitrazine, and fetal fibronectin testing. A diagnosis of preterm labor was made in the presence of contractions occurring at a frequency of 4 in 20 min or 8 in 60 min plus progression in the cervix or a cervical dilatation ≥1 cm or a cervical effacement ≥80%. We defined steroid exposure as any exposure to steroids, regardless of completion of the full 48 hr course because even partial exposure is known to confer pulmonary and neurologic benefit (14,15) and antibiotic exposure as any antenatal antibiotic administration after admission.
Histologic chorioamnionitis was performed by examining tissue samples from umbilical cord, chorionic plate, and membranes fixed with 10% neutral buffered formalin, and embedded in paraffin. Sections of tissue block were stained with hematoxylin and eosin. Clinical chorioamnionitis was diagnosed in the presence of a temperature elevation to 37.8℃ or higher and two or more of the following four criteria; uterine tenderness, malodorous vaginal discharge, fetal tachycardia >160 beats/min, and maternal leukocytosis >15,000 cells/µL as described by Gibbs and colleagues (16).
Cranial ultrasound scans were obtained before day of life 3, on days 7, at discharge or at days 30. In cranial ultrasound scans we examined for intraventricular hemorrhage (IVH), ventriculomegaly, periventricular leukomalacia, germinal matrix hemorrhage (GMH). As described by Salafia and colleagues (4), early GMH was defined as a diagnosis of GMH within 72 hr of birth, and late GMH as all other cases of diagnosed GMH after 72 hr of life.
A diagnosis of neonatal sepsis was made in the presence of a positive culture of blood, urine, or cerebrospinal fluid. Suspected neonatal sepsis was diagnosed in the absence of a positive culture when two or more of the following criteria was present; 1) a white blood cell count of <5,000 cells/µL; 2) a polymorphonuclear leukocyte count of <1,800 cells/µL; 3) an I:T ratio (ratio of bands to total neutrophils) >0.2; 4) Creactive protein positive; and 5) a platelets count of <80,000 cells/µL. These criteria have been previously used in the pediatric and obstetrics literature (11). Necrotizing enterocolitis was diagnosed in the presence of abdominal distention and feeding intolerance for at least 24 hr (vomiting or increased gastric residual) with clear radiologic evidence of intramural air, perforation, and meconium plug syndrome.
Results were presented as means±tandard deviations for continuous variables and percentages for nominal variables. Statistical tests utilized were one-way analysis of variance and chi-square testing. To evaluate possible confounding, we carried out univariable analyses. Logistic regression was used to investigate the regression relationships between the latency interval and histologic chorioamnionitis after controlling for gestational age at delivery, the uses of antibiotics and corticosteroid, neonatal birthweight at delivery, and delivery mode; early GMH, late GMH. SPSS version 10.0 was used and a p value of <0.05 was considered significant.
There were no statistically significant differences between study groups with regard to maternal age, gestational age at admission, gestational age at delivery, and neonatal birthweight, but 1-, 5-min Apgar scores were higher in the pPROM group (Table 1). There were five perinatal deaths. In the pPROM group, two neonates died; one at 27 weeks (1,185 gram) and the other at 29 weeks (1,240 gram) died from disseminated intravascular coagulation (DIC) and pulmonary hemorrhage. The latency interval was 1 hr in one and 3 hr in the other. In the intact membrane group, neonatal death occurred in three neonates; one at 25 weeks (1,040 gram), another at 26 weeks (820 gram), and the other at 27 weeks (1,300 gram) died from respiratory distress syndrome and DIC, respectively. The latency interval was 23 hr in one, 32 hr in another, and 12 hr in the other (Table 2).
In the pPROM group, clinical chorioamnionitis, vasculitis, funisitis did not increase with increasing latency interval. However, histologic chorioamnionitis increased with increasing latency interval. In the intact membranes group, vasculitis and funisitis were not observed (Table 4).
In patients with pPROM, two neonates had ventriculomegaly. One was strongly suggested aqueductal stenosis and the other was spontaneously recovered. No relationship was observed between latency interval and neonatal brain damage in either group (Table 3, 5). We reevaluated neonatal cranial ultrasound results of pPROM patients without results of placental pathology. In total 115 patients with pPROM, no statistically significant relationship was observed between latency interval and neonatal brain damage.
A positive blood culture was obtained in 3 infants of the pPROM group and in 4 infants of the intact membrane group. Within 24 hr after birth, the results of blood culture were positive in 2 infants of the pPROM group and in 2 infants of the intact membrane group. The microbial isolates were Coagulase negative Staphylococcus (n=3), Klebsiella pneumoniae (n=1), Candida rucidase (n=1), Enterobacter cloacae (n=1), Xanthomonas maltophila (n=1). In four cases (4/7), histologic chorioamnionitis was accompanied by a positive blood culture. However, latency interval was not associated with neonatal sepsis in either group (Table 3).
In the present study, we found that the risk of histologic chorioamnionitis increases with latency, but no relationship was between the neonatal brain damage and latency intervals in patients with pPROM. In the patients with preterm labor and intact membranes, histologic chorioamnionitis and neonatal brain damage were not associated with latency interval. These results were accorded with those of McElrath et al. (17). Chorioamnionitis was found to be increase with increasing latency due to ascending trans-cervical infection, but it was suggested that ascending infection after PROM did not affect neonatal brain damage. We suggest that conservative management reduces respiratory distress syndrome due to premature lung maturation and a low birthweight without increasing the risk of neonatal brain damage, and the risk of neonatal brain damage is increased in the presence of an intrauterine infection due to ascending infection before PROM.
Diagnostic methods of intrauterine infection include amniotic fluid culture and placental pathologic examination. However, these methods are invasive, and in particular, placental pathologic examination is used only after delivery, and has limited to before delivery. Recently, several studies has been reported upon diagnostic methods of intrauterine infection is found. In Korea, Yoon et al. (18) and Kim and Yoon (19) reported that amniotic fluid interleukin-6 and amniotic fluid WBC count are a sensitive test for the prospective diagnosis of acute histologic chorioamnionitis and for the identification of neonates at risk of significant morbidity and mortality. We found that 4 pPROM patients were diagnosed as having clinical chorioamnionitis before delivery. However, 25 pPROM patients was diagnosed as histologic chorioamnnionitis after delivery. Three pPROM pateints (12%) with clinical chorioamnionitis was diagnosed as histologic chorioamnionitis. This result was lower than reported by Yoon et al. (41%) (18). It is suggested that in patients with expectant management without symptoms of clinical chorioamnionitis, the delay of delivery is risk of intrauterine infection. Thus, accurate, rapid and less invasive diagnostic methods of intrauterine infection before delivery are required.
Intraventricular hemorrhage and periventricular leukomalacia have a strong association with subsequent development of cerebral palsy. Although the cause of cerebral palsy is uncertain, it has been reported that white matter damage is an important cause (20,21). Several studies about the relationship between histologic chorioamnionitis and neurologic sequelae such as cerebral palsy or neurodevelopment impairment of infants have been reported (22-25). However, no studies of the relationship between cerebral palsy or neurodevelopemental impairment of infants and latency after pPROM have been reported.
This study has several limitations. First, this is a cohort of women who have been evaluated retrospectively. Although they were managed by a uniform policy of expectant management with standardized protocols for steroid and antibiotic administration and antepartum fetal surveillance, each was cared for by variety of different caregivers. The ultimate decision to proceed with delivery is often dependent on the attending physician's decisions. This could have biased our results. Second, adverse long term neurologic sequelae such as cerebral palsy and neurodevelopemental impairment are not observed in pregnancies complicated by prolonged pPROM. Additional research needs to be evaluated the relationship between the latency interval and long term neurologic sequelae.
Figures and Tables
References
1. Naylor CS, Gregory K, Hobel C. Premature rupture of membranes: An evidence-based approach to clinical care. Am J Perinatol. 2001. 18:397–413.
2. Mercer BM. Preterm premature rupture of membranes. Obstet Gynecol. 2003. 101:178–193.
3. Aagaard-Tillery KM, Nuthalapaty FS, Ramsey PS, Ramin KD. Preterm premature rupture of membranes: perspectives surrounding controversies in management. Am J Perinatol. 2005. 22:287–297.

4. Salafia CM, Minior VK, Rosenkrantz TS, Puzullo JC, Popek EJ, Cusick W, Vinzileos AM. Maternal, placental and neonatal associations with early germinal matrix/intraventricular hemorrhage in infants born before 32 weeks' gestation. Am J Perinatol. 1995. 12:429–436.

5. Vergani P, Patane L, Doria P, Borroni C, Cappellini A, Puzello JC, Ghidini A. Risk factors for neonatal intraventricular hemorrhage in spontaneous prematurity at 32 weeks gestation or less. Placenta. 2000. 21:402–407.
6. Thorp JA, Jones PG, Clark RH, Knox E, Peabody JL. Perinatal factors associated with severe intracranial hemorrhage. Am J Obstet Gynecol. 2001. 185:859–862.

7. Adinolfi M. Infectious disease in pregnancy, cytokines and neurological impairment: an hypothesis. Dev Med Child Neurol. 1993. 6:58–61.
8. Selmaj KW, Raine CS. Tumor necrosis factor mediates myelin and oligodendrocytes damage in vitro. Ann Neurol. 1998. 6:58–61.
9. Leviton A. Preterm birth and cerebral palsy: Is tumor necrosis factor the missing link? Dev Med Child Neurol. 1993. 35:553–558.

10. Yoon BH, Romero R, Yang SH, Jun JK, Kim IO, Choi JH, Syn HC. Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. Am J Obstet Gynecol. 1996. 174:1433–1440.

11. Gomez R, Romero R, Ghezzi F, Yoon BH, Mazor M, Berry SM. The fetal inflammatory response syndrome. Am J Obstet Gynecol. 1998. 179:194–202.

12. Kim WS, Choi CH, Lee SH, Choi SJ, Kim JU, Les ES, Son YS, Kim JH, Roh CR. Maternal and fetal outcomes according to the latency period in preterm premature rupture of membrane. Korean J Perinatol. 2004. 15:369–378.
13. Gopalani S, Krohn M, Meyn L, Hitti J, Crombleholme WR. Contemporary management of preterm premature rupture of membranes: Determinants of latency and neonatal outcome. Am J Perinatol. 2004. 21:183–190.

14. Ikegami M, Polk D, Jobe AH. Minimal interval from fetal betamethasone treatment to postnatal lung responses in preterm lambs. Am J Obstet Gynecol. 1996. 174:1408–1413.
15. Wright LL, Verter J, Younes N, Stevenson D, Fanaroff AA, Shankaran S. Antenatal corticosteroid administration and neonatal outcome in very low birth weight infants: the NICHD Neonatal Research Network. Am J Obstet Gynecol. 1995. 173:169–174.

16. Gibbs RS, Blanco JD, St Clair PJ, Castaneda YS. Quantitative bacteriology of amniotic fluid from women with clinical intraamniotic infection at term. J Infect Dis. 1982. 145:1–8.

17. McElrath TF, Allred EN, Leviton A. Prolonged latency after preterm premature rupture of membranes: An evaluation of histologic condition and intracranial ultrasonic abnormality in the neonate born at <28 weeks of gestation. Am J Obstet Gynecol. 2003. 189:794–798.
18. Yoon BH, Romero R, Kim CJ, Jun JK, Gomez R, Choi JH, Syn HC. Amniotic fluid interleukin-6: A sensitive test for antenatal diagnosis of acute inflammatory lesions of preterm placenta and prediction of perinatal morbidity. Am J Obstet Gynecol. 1995. 172:960–970.

19. Kim MH, Yoon BH. The diagnostic and prognostic value of amniotic fluid white blood cell count in patients with preterm premature rupture of membranes. Korean J Obstet Gynecol. 2002. 45:101–111.
20. Grether JK, Nelson KB. Maternal infection and cerebral palsy in infants of normal birth weight. JAMA. 1997. 278:207–211.

21. Wu YW, Colford JM Jr. Chorioamnionitis as a risk factor cerebral palsy: A meta- analysis. JAMA. 2000. 284:1417–1424.
22. Yoon BH, Romero R, Park JS, Kim CJ, Kim SH, Choi JH, Han TR. Fetal exposure to intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am J Obstet Gynecol. 2000. 182:675–681.
23. Dexter SC, Pinar H, Malee MP, Hogan J, Carpenter MW, Vohr BR. Outcome of very low birth weight infants with histologic chorioamnionitis. Obstet Gynecol. 2000. 96:172–177.
24. Morales WJ. The effect of chorioamnionitis on the developmental outcome of the preterm infants at one year. Obstet Gynecol. 1987. 70:183–186.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download