Abstract
To investigate what heterogeneity exists in breast cancer, 228 consecutive patients with operable invasive duetal carcinoma (IDC), not otherwise specified, were categorized on the basis of the horizontal progression model of carcinogenesis. Using the reversed Black's nuclear grade (RBNG) in the IDC component and the association of ductal carcinoma in situ (DCIS), the patients were classified into pure IDC (IDC de novo or ab initio) as Group I, non-high grade (RBNG 1 and 2) IDC with DCIS as Group II, and high grade (RBNG 3) IDC with DCIS as Group III. The Groups classified in the present study appeared as a prognostic factor independent of known prognostic and predictive factors in multivariate test. Group I had the worst prognosis among the three groups and was the most non-responsive to tamoxifen. After performing stratifying analyses by group, it was found that metastasis-free survival was statistically associated with the status of hormone receptors estrogen receptor and progesterone receptor and tamoxifen therapy only in Group II. In addition, the status of c-erbB-2 expression had prognostic significance only within the Group III. Our results may be used to frame an alternative hypothetical model for breast cancer evolution and will lead us to reconsider the tailoring of the comprehensive therapeutic modality used at the present time.
In spite of recent advances in diagnosis and treatment, 10 to 20% of the patients with breast cancer die within 5 yr (1). However, 1 out of 5 patients with neglected breast cancer survived over 5 yr from the onset of symptoms even before the 1940s (2,3). Analysis of the survival curves of women with breast cancer suggests that there are two or more populations among patients with breast cancer. One subgroup represents approximately 40% of the total patients and has a relative mortality of about 25% per year. The other subgroup representing the remaining 60% has a relative mortality rate of about 2.5% per year (4). The relative mortality of 2.5% per year represents a relative mortality risk equivalent to that of cigarette smoking. These extreme outcomes have been believed to be due to heterogeneous nature of breast cancer.
Understanding the carcinogenesis of breast cancer may be the cornerstone for solving the enigma of heterogeneity. Of the many hypothetical models for cancer evolution, the conventional model (5), also called a vertical progression, is unlikely to apply to breast carcinogenesis. Instead, a horizontal progression model is more acceptable, in that the grade and biological profile of ductal carcinoma in situ (DCIS) correlate with the invasive tumor of the corresponding grade and biological profile when DCIS progresses to invasive ductal carcinoma (IDC). This model has gained persuasiveness by virtue of a pioneering study using loss of heterozygosity (LOH) analysis on the continua from the normal tissue, through potential precursors of breast cancer, to invasive cancer (6). The results also supported the presumption that proliferative disease without atypia and atypical hyperplasia could transform directly to invasive breast cancer without passing through the stage of carcinoma in situ. Buerger and colleagues supported the model by examining specific chromosomal alterations in DCIS and associated IDC by means of comparative genomic hybridization (CGH) (7). They reported that high-grade DCIS was genetically different from low and intermediate-grade DCIS, and that the evolution of high-grade DCIS might be along a different pathway from other grades. In the case with concurrent IDC, the genetic alterations were similar in both invasive and noninvasive component.
In the present study, we classified the patients with IDC into IDC de novo and IDC associated with DCIS. Then, we subdivided IDC associated with DCIS into two groups according to the nuclear grade of the invasive component. To determine what biological difference existed between the three groups, known prognostic and predictive factors (8-10) were assessed separately and the results between the groups were compared. For the purpose of identifying how predictive factors affected the survival of each group, we stratified the patients into groups and calculated the metastasis-free survival in each group by adjusting each predictive factor.
This study was designed on the premise that heterogeneity might be derived from the diversity of the original cells as well as from distinct subsets of genetic alterations. The results from this study will lead us to expand the concept of breast carcinogenesis, as well as force us to reconsider the paradigm of the comprehensive therapeutic approach to breast cancer.
256 consecutive patients diagnosed with primary operable invasive breast carcinoma who underwent surgery at Samsung Cheil Hospital of Sungkyunkwan University between 1996 and 1997 were reviewed. In order to guarantee at least 5 yr of follow-up, the end of 1997 was set as the cut-off date. The patients were identically submitted to receive adjuvant systemic therapy according to the contemporary therapeutic guidelines determined by their clinical and pathological findings. Any tumor that demonstrated at least 90% defining histologic characteristics of a special-type cancer was designated as that special type. Patients who had special types (17 cases), who refused the guideline-based adjuvant systemic therapy (3 cases), refused further resection and/or radiotherapy for pathologically positive resection margin (2 cases), who were diagnosed with the second metachronous breast cancer (2 cases), and who had inappropriate surgical specimens due to neoadjuvant therapy (5 cases) were excluded from the analysis to eliminate any confounding effect on clinical outcome.
228 IDC were reviewed retrospectively on the basis of hospital records and contact with patients or their families. Patients were observed through physical examination and radiological study every 6 months for the first 2 yr after surgery, and thereafter with biannually physical examination and annual radiological study. The median follow-up of the living patient was 62 months (range, 6 to 80). The median age of the patients was 46 yr (range, 24 to 76). Anyone who submitted to hormonal therapy received 20 mg of tamoxifen for 5 yr or until the last follow-up.
Pathologic information on nodal status and tumor size was obtained from the original reports. Paraffin block was made in 5 mm-thickness with the surgical specimen that had been grossly suspicious of tumor. A 4 µm-thick slide was prepared from each block and was examined for the original reports. When DCIS was suspected of focal invasion or pure IDC was suspected of associating focal DCIS, the 5 mm-thick paraffin block was silced in 2 mm-thickness. A slide was obtained from every 2 mm-thick paraffin block additionally and was examined. The association of DCIS was noted on all the pathologic reports when it was associated with IDC. The tumor size of invasive component was determined by gross measurements of the surgical specimen or by the largest diameter on the slide. The nuclear grade of the invasive component in each tumor was assessed according to a modification of Black's nuclear grade (reversed Black's nuclear grade, RBNG, Fig. 1) by peer-review (11). In order to minimize intra/inter-observer bias, all slides were repeatedly reviewed by a single pathologist until the result was uniform.
5 µm-sections of formalin-fixed, paraffin-embedded breast cancer specimens were prepared on polysine coated slides. Immunohistochemical staining was performed using the streptoavidin-biotin method, according to the supplier's protocol (DAKO, LSAB kit, Carpinteria, CA, U.S.A.). We used monoclonal mouse anti-(human Ig) antibodies directed against estrogen receptors (ER) (DAKO, 1:100), progesterone receptors (PR) (DAKO, 1:50), and p53 (DO-7, DAKO, 1:100). Immunohistochemistry for c-erbB-2 (DAKO, 1:150) was done with polyclonal rabbit anti-(human Ig) antibodies. The expression of ER, PR, and p53 showing more than 5% of nuclear immunostaining was defined as positive. For c-erbB-2, a four-tier system of scoring, as recommended by Dako corporation, was used (12). Complete cytoplasmic membrane staining (2+ or 3+ score) in more than 10% of the cells was read as positive. Partial membrane staining (1+ score) or no (0 score) membrane stain was read as negative.
The patients whose IDC was not associated with DCIS were classified as Group I. The patients with IDC associated with DCIS were divided into two groups according to the RBNG of the invasive component. IDC with RBNG 1 or 2 was arbitrarily defined as non-high grade IDC, and the patients with non-high grade IDC were classified as Group II. IDC with RBNG 3 was defined as high grade IDC, and the patients with high grade IDC were classified as Group III.
In order to compare malignant capacity among three groups, we used metastasis-free survival (MFS) as a clinical parameter. MFS was defined as the elapsed time from surgery to distant disease recurrence or death. The patients were censored at the last known follow-up as being without metastasis when metastasis was unknown. During the follow-up period, a patient died of congestive heart failure and was censored.
Statistical analyses were conducted in SPSS (version 9.0). We compared the three groups regarding the status of ER,PR, p53, c-erbB-2, and menopausal status using the Pearson chi-square test. Tumor size and nodal status were staged as T0, T1, T2, T3 or N0, N1, N2, and N3 according to the 6th edition of TNM classification. The distribution of T stage and N stage was compared among the three groups using the Pearson chi-square test. Cumulative MFS curve for each group was calculated using Kaplan-Meier method and compared among the three groups by log rank test. To identify what variables related independently to MFS, multivariate analysis was performed by Cox regression test including ER, PR, p53, c-erbB-2, tumor size, nodal status, RBNG, and the group. After stratifying patients by group, MFS for subgroups adjusted with the status of ER, PR, p53, c-erbB-2, and tamoxifen therapy within each group were calculated on the Kaplan-Meier cumulative survival curve. To investigate how the predictive factors and tamoxifen therapy affected survival in each group, the MFS for the subgroups were compared within each group by a log rank test. Statistical significance was accepted when the p-value was less than 0.05.
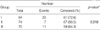
84 cases (36.8%) were included in Group I. Group II and III included 74 cases (32.5%) and 70 cases (30.7%) respectively (Table 1). The mean age was similar among the three groups, whereas the proportion of premenopausal women was largest in Group III (p=0.029). The primary surgical and adjuvant treatment were also similar in the three groups. Details of patient characteristics are listed in Table 1.
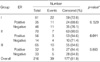
Table 2 shows the distribution of the prognostic and predictive factors in the three groups, and describes the relationship between the factors and groups. The distributions of T stage and N stage were similar in 3 groups. ER, PR, and p53 were assessed in 216, 216, and 211 cases, respectively. ER status was statistically different between the groups (p<0.001). ER was most frequently positive in Group II (80.0%). PR status was also statistically different between the groups (p=0.022). PR was most frequently positive in Group II (68.6%). The positive rate of p53 expression was significantly different between the groups (p=0.040). Of 228 cases, 211 cases were assessable for c-erbB-2 expression. There was no difference in the positive rate of c-erbB-2 expression between the groups (p=0.243).
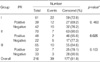
MFS analysis comparing groups is described in Table 3, and is depicted by the Kaplan-Meier cumulative curve (Fig. 2) Group II showed significantly favorable outcome (p=0.010) with 90.5% of MFS rate during the follow-up period in comparison to 72.6% in Group I and 84.3% in Group III. In the multivariate analysis, the independent factors associated with MFS were Group (p=0.025), nodal status (p=0.000), tumor size (p=0.038), and RBNG (p=0.024) whereas ER, PR, p53, c-erbB-2, and menopausal status did not emerge as a prognostic factor (Table 4). Table 5, 6 describe MFS for subgroups within each Group adjusted with ER and PR, respectively. Within Group II, the subgroup of patients with ER positive showed better survival function than the subgroup with ER negative (p=0.011) while no significant difference in survival function existed between the subgroups in either Group I or III. In Group II, the subgroup of patients with PR positive showed statistically better survival function than the subgroup with PR negative (p=0.025), while no significant difference in survival function existed between the subgroups in either Group I or III. In regards to the status of p53 expression, it had no statistically significant influence upon the patient's survival function in any group (p=0.405, 0.243, and 0.260 in Group I, II, and III, respectively). The subgroup with c-erbB-2 positive had worse prognosis than that with c-erbB-2 negative in Group III (p=0.035), but not in Group I (p= 0.167) or II (p=0.180). MFS for groups adjusted with tamoxifen therapy had a similar tendency to that with ER and PR. Within Group II, the subgroup of patients who received tamoxifen showed significantly better survival function than the subgroup of the patients who had not received it (p=0.018), while no difference in survival function existed between the two subgroups within either Group I or III (Fig. 3).
Breast cancer is well known for comprising a heterogeneous spectrum of malignant proclivities, and its initiation and early progression are associated with genetic abnormalities. There has been a presumptive mechanism that makes for the heterogeneity of breast cancer. The mechanism is that distinct series of genetic alterations result in heterogeneous phenotypes of breast cancer (5,6). According to the mechanism, there are at least three genetically different types of breast cancer, which are the pure IDC that dose not pass through the stage of DCIS, non-high grade IDC associated with DCIS, and high grade IDC associated with DCIS. When cancers clustered by certain series of genetic alterations express identical biological characteristics including their clinical outcome, this mechanism could be exclusively accepted. Recently a challenging mechanism has been proposed that the heterogeneity of breast cancer may be derived from the diversity of the original cells for neoplastic transformation, which is thought to exist in the terminal duct lobular unit of the human mammary gland (13,14). The cells in the terminal duct lobular unit basically consist of glandular and myoepithelial cells. If all the cancer expressing certain specific cellular lineage markers have the same natural history, the second hypothesis must be true. In the view of diachrony, however, details of genetic alterations in cancer change with progression in some breast cancers. Furthermore, the genetic alterations in a clone tend to increase substantially from DCIS to IDC (15-16). A group of investigators found that a certain genotype predisposes to the basal tumor subtype, resulting in poor clinical outcome (17). Therefore, it is much more reasonable to accept the combination of both mechanisms.
Notwithstanding the importance of the second mechanism, the present study has been designed on the basis of the first mechanism because the second is still in experimental stage. In parallel, authors have presumed that pure IDC would originate from the cell located at a place easily accessible to destroy the barrier to stromal invasion, namely, the basement membrane, from the beginning of its evolution. Previous studies have reported that pure IDC accounted for 20 to 40% of all diagnosed IDC, not otherwise specific (18,19). These wideranged proportions of pure IDC are thought to vary with the proportion of microscopically undetectable DCIS associated with IDC. Certain category of DCIS has progressed to IDC so fast that it might have been determined to be pure IDC at the time of diagnosis. Even with this uncertainty, one cannot help but accept the existence of pathologically pure IDC unless pathologists cut paraffin-blocks thick enough to examine all ducts or lobules and, thereafter, affirm concurrent DCIS.
The patients in the present study were divided into 3 groups as a group of pure IDC (Group I) and two groups of IDC with DCIS (Group II and III). There were significant differences in MFS among the groups, and Group I had the worst prognosis, as the authors had predicted. Silverberg et al. (18) also reported that the patients with pure IDC had worse prognosis than those with IDC with DCIS. Of the many factors indicating prognosis at the initial treatment of breast cancer, tumor size, nodal status, and histological grade are the prognostic factors for which clinical value have been confirmed (8,20). Because tumor size or nodal status is a momentary feature of diachronic change, the causal relation between the factors and prognosis needs no further explanation other than its terminology. In other words, there is no doubt that the size of tumor proportionally reflects the possibility of metastasis (21). A recent study revealed that the survival time after metastasis varied with the histological grade of the primary tumor, not the size or nodal status of the primary tumor (22). So what determines the histological grade of breast cancer? Should it be time, genotype, or the original cell? How can histological grade affect the fate of patients? These are theses that need to be demonstrated.
The lethality of regionally treated breast cancer without systemic therapy is directly related to nuclear grade (23). Nuclear grade can be assessed even in a minimal invasive carcinoma or in a specimen taken by preoperative core-needle biopsy. In addition, Leong et al. (24) found that the nuclear grade of DCIS produced significant correlation with the largest number of parameters known to be of prognostic relevance in both concurrent IDC as well as DCIS. These are the reasons that we have taken RBNG in the present study as the pathologic grade of IDC instead of the modification of the Bloom and Richardson criteria (20), which is used worldwide now.
Interobserver disagreement between low and intermediate nuclear grade was very high in one study (25). Many studies showed a statistically significant difference in the outcome only between high grade and non-high (low and intermediate) grade DCIS, and this concept has been confirmed by the study of biologic marker (26). We divided IDC with DCIS into two groups as the IDC with non-high grade nuclear grade (Group II) and that with high nuclear grade (Group III). In our study, Group II showed more favorable metastasis-free survival than Group III.
More than a few different biologic characteristics appeared among the three groups in the present study. There was no comparable data derived from the studies that use the same classification as we did, as well as that was performed with more refined design. In addition to the retrospective analysis, the population size of the present study is not sufficient to provide conclusive information. Nevertheless, the present study has yielded some intriguing results for which implications must be clarified.
First, the frequency of premenopausal women was remarkably higher in Group III (82.9%) compared to both Group I (64.3%) and II (67.6%), even though the mean age was similar in all three groups.
Second, there were statistically significant differences in MFS among the three groups in univariate analyses. In addition, the Group was a prognostic factor independent of tumor size, nodal status, nuclear grade, and important predictive factors in multivariate analyses.
Third, the nuclear grade appeared as an independent prognostic factor in multivariate analysis and the proportion of the patients with high nuclear grade IDC was larger in Group III (100%) than in Group I (63%), while Group III showed more favorable survival function that Group I (Table 1).
Fourth, in stratifying the patients by group, MFS was adjusted with tamoxifen treatment and four major predictive factors (ER, PR, p52, and c-erbB-2). Only in Group II, ER or PR positive subgroup as well as the tamoxifen-treated subgroup showed significantly better survival function than their counterparts, even though neither ER nor PR status was an independent prognostic factor in multivariate analysis for all the patients included in the present study. While c-erbB-2 was not an independent prognostic factor in multivariate analysis, the prognostic value of c-erbB-2 expression was demonstrated in Group III, but not in Group I or II.
Many controlled studies adjusting the subsets of nodal status or tumor size have been tried. The prognostic significance of c-erbB-2 overexpression has not yet been adequately validated (8). So what makes the prognostic value of c-erbB-2 statistically apparent in Group III in the present study? More sophisticated studies are needed to solve the question. There have been conflicting opinions on whether the ER or PR status itself is a significant predictor of clinical outcome, or not (8). In the present study there was a questionable tendency of tamoxifen having had no survival benefit in Group I and III, in addition to the fact that the subgroup that received tamoxifen in Group I showed an even lower MFS rate than its counter subgroup even though it had no statistical significance (Fig. 3). When this finding is reproduced in a large scale-controlled study, we will have to change the strategy of the systemic therapy has been recommended for the patients with breast cancer until now. The paradigm that breast cancer is a heterogeneous disease should be also shifted to the new one that breast cancer consists of at least two different diseases. The authors have formed a hypothesis that the original cell of the cancers in Group I would be biologically different from that of the cancers in the remaining two groups. This is the speculation that the authors are trying to derive from the present study.
Authors postulate that the pure IDC might originate from developmentally primitive cells that can differentiate into myoepithelial cell. The adult mammary epithelial stem cell, multipotent progenitor, and basal (or myoepithelial) progenitor can be proposed as these cells (13,14). With genetic mutations, these cells transformed to the cells that fail to differentiate into more differentiated cells, the glandular cells, the myoepithelial cells, or the alveolar cells. This might be the reason why there is no myoepitheial cell or alveolar cell in the invasive component of IDC. Of course, these cells are apt to grow without constructing the basement membrane, in other words, they grow with invading stromal tissue from the beginning. Even these cells could build the basement membrane, the spatial characteristic of progenitor cells allows the cancer to grow out of the basement membrane at birth. It serves as a crack on the bombshell and acts like a bomb that explodes as soon as its bombshell breaks. As a matter of course, it does not have enough time to develop a preneoplastic field such as that concept of field cancerization of Slaughter et al. (27), so the cancer never passes through DCIS. In consequence, metastasis can also occur from the early stages of cancer under such a condition. This postulation will be very practical for breast surgeons because pure IDC would define the real systemic category of breast cancer. Accordingly, preoperative systemic therapy and lumpectomy could be the standard treatment in patients with pure IDC. Moreover, the transformed stem or progenitor cells should respond to tamoxifen different from the cells that were transformed at more differentiated stage. It can be presumed that this may give rise to resistance, or even adverse effect to tamoxifen in Group I regardless of the status of ER or PR. From the viewpoint of the development of the human mammary gland, this category should define a small proportion of all breast cancers on account of the small population of the myoepithelial cells relative to the glandular cells in normal breast tissue. In the present study, Group I defined 36.8% of the total cases. This is too large a proportion in comparison with the range from 16% to 28% in the previous studies carried out with the immunohistochemistry using antibodies against breast basal (or myoepithelial) cell cytokeratins (14,28). The discrepancy between the proportion of Group I and the proportion of the patients with basal cytokeratin-expressing cancer in the studies is thought to stem from the fact either Group I could not directly reflect the biologic properties of pure IDC or because Group I was conflated with pure IDC and IDC associated with microscopically undetected DCIS. Therefore, an appropriate pathological guideline to characterize pure IDC should be created. In order to purify Group I as biologically pure IDC, an immunochemical study using biomakers that sort cancer cells by each developmental stage is needed. These biomarkers are thought to be glandular or basal cytokeratins, alpha-smooth muscle actin, and certain mammary stem cell markers. Now the expression of the biomarkers representing the characteristics of stem cell or of cellular lineages of the mammary gland is under investigation in various types of breast cancer as the next step of our project.
Expounding the hypothetical pathogenesis of cancer in Group II or III seems to be more complex (29). We have to take a rain check on it until we have a definitive result from our successive studies.
If biologically different subgroups are conflated into a group and are tailored by the same therapeutic modality, some of them may be deprived of the chance for receiving the correct regimen, or some others may lose the golden time for optimal systemic therapy. The limit of follow-up duration, insufficient size of population, and uncontrolled retrospective analysis are the criticizable drawbacks of the present study. The force of mortality in the overall survival curve is similar to virulence (the rate of appearance of distant metastasis), but competing mortality obscures metastagenicity (the ultimate likelihood of a tumor developing distant metastasis) when survival serves as the end point (9). Considering this and the fact that metastatic breast cancer is incurable, the time of distant metastasis can be more suitable as the end point of follow-up than death as a point at which to compare mortalities between subgroups in case the duration of follow-up does not reach 10 yr. Taking the time of distant metastasis as the end point can offset the limit of follow-up duration in this study. In order to overcome the problem of insufficient sample size and uncontrolled study design, we have only to apply this hypothetical classification to some larger- scale-controlled study already reported (30). If the results correspond to ours, this classification can be used to test the efficacy of newly developed drugs, and to determine the fashioning of a specific tailored therapy. Ultimately, we might have to treat the three groups as individual disease entities, just as hematologists define leukemia according to the cellular lineages derived from hematopoietic stem cell.
Figures and Tables
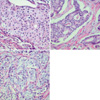 | Fig. 1Reversed Black's nuclear grade of invasive ductal carcinoma (H&E stain, ×400). Tumor cells in invasive component of ductal carcinoma, not otherwise specific, show grade 1 (A), 2 (B), and 3 (C), respectively. |
Table 1
Patient characteristics

*All p-values were calculated by the Pearson chi-square test, except the mean age of the patients (‡by ANOVA). †The group I consists of 31 invasive ductal carcinomas with non-high nuclear grade and 53 invasive ductal carcinomas with high nuclear grade. MRM, modified radical mastectomy; BCS, breast conservation surgery; RT, radiotherapy at the ipsilateral breast and axilla; LRRT, radiotherapy at the ipsilateral breast, axilla, and supraclavicular lymph nodes; CMF, cyclophosphamide+methotrexate+5-fluorouracil; FAC, 5-fluorouracil+doxorubicin+cyclophosphamide.
ACKNOWLEDGMENT
We would like to dedicate this paper to the late Mrs. Won-Soon Ku who offered financial support for this study and inspired us to challenge a project named 'STOP Breast Cancer (the Strategy for Ten percent Overall survival Promotion of Breast Cancer).
References
1. Sant M, Allemani C, Berrino F, Coleman MP, Aareleid T, Chaplain G, Coebergh JW, Colonna M, Crosignani P, Danzon A, Federico M, Gafa L, Grosclaude P, Hedelin G, Mace-Lesech J, Garcia CM, Moller H, Paci E, Raverdy N, Tretarre B, Williams EM. European Concerted Action on Survival and Care of Cancer Patients (EUROCARE) Working Group. European Concerted Action on Survival and Care of Cancer Patients (EUROCARE) Working Group. Breast carcinoma survival in Europe and the United States. Cancer. 2004. 100:715–722.
2. Bloom HJ, Richardson WW, Harries EJ. Natural history of untreated breast cancer (1805-1933). Comparison of untreated and treated cases according to histological grade of malignancy. Br Med J. 1962. 5299:213–221.
3. Johnstone PA, Norton MS, Riffenburgh RH. Survival of patients with untreated breast cancer. J Surg Oncol. 2000. 73:273–277.

5. Vogelstein B, Fearon ER, Hamilton SR, Kern SE, Preisinger AC, Leppert M, Nakamura Y, White R, Smits AM, Bos JL. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988. 319:525–532.

6. O'Connell P, Pekkel V, Fuqua S, Osborne CK, Allred DC. Molecular genetic studies of early breast cancer evolution. Breast Cancer Res Treat. 1994. 32:5–12.
7. Buerger H, Otterbach F, Simon R, Poremba C, Diallo R, Decker T, Riethdorf L, Brinkschmidt C, Dockhorn-Dworniczak B, Boecker W. Comparative genomic hybridization of ductal carcinoma in situ of the breast-evidence of multiple genetic pathways. J Pathol. 1999. 187:396–402.
8. Mirza AN, Mirza NQ, Vlastos G, Singletary SE. Prognostic factors in node-negative breast cancer: a review of studies with sample size more than 200 and follow-up more than 5 years. Ann Surg. 2002. 235:10–26.
9. Heimann R, Hellman S. Clinical progression of breast cancer malignant behavior: what to expect and when to expect it. J Clin Oncol. 2000. 18:591–599.

10. Clark GM. Harris JR, Lippman ME, Morrow M, Osborne CK, editors. Prognostic factors and Predictive Factors. Diseases of the breast. 2000. Philadelphia: Lippincott Williams & Wilkins;489–514.
11. Fisher ER, Redmond C, Fisher B. Histologic grading of breast cancer. Pathol Annu. 1980. 15:239–251.
12. Bose S, Mohammed M, Shintaku P, Rao PN. Her-2/neu gene amplification in low to moderately expressing breast cancers: possible role of chromosome 17/Her-2/neu polysomy. Breast J. 2001. 7:337–344.

13. Bocker W, Moll R, Poremba C, Holland R, Van Diest PJ, Dervan P, Burger H, Wai D, Ina Diallo R, Brandt B, Herbst H, Schmidt A, Lerch MM, Buchwallow IB. Common adult stem cells in the human breast give rise to glandular and myoepithelial cell lineages: a new cell biological concept. Lab Invest. 2002. 82:737–746.

14. Abd El-Rehim DM, Pinder SE, Paish CE, Bell J, Blamey RW, Robertson JF, Nicholson RI, Ellis IO. Expression of luminal and basal cytokeratins in human breast carcinoma. J Pathol. 2004. 203:661–671.

15. O'Connell P, Pekkel V, Fuqua SA, Osborne CK, Clark GM, Allred DC. Analysis of loss of heterozygosity in 399 premalignant breast lesions at 15 genetic loci. J Natl Cancer Inst. 1998. 90:697–703.
16. Farabegoli F, Champeme MH, Bieche I, Santini D, Ceccarelli C, Derenzini M, Lidereau R. Genetic pathways in the evolution of breast ductal carcinoma in situ. J Pathol. 2002. 196:280–286.
17. Sorlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, Deng S, Johnsen H, Pesich R, Geisler S, Demeter J, Perou CM, Lonning PE, Brown PO, Borresen-Dale AL, Botstein D. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA. 2003. 100:8418–8423.
18. Silverberg SG, Chitale AR. Assessment of significance of proportions of intraductal and infiltrating tumor growth in ductal carcinoma of the breast. Cancer. 1973. 32:830–837.

19. Lampejo OT, Barnes DM, Smith P, Millis RR. Evaluation of infiltrating ductal carcinomas with a DCIS component: correlation of the histologic type of the in situ component with grade of the infiltrating component. Semin Diagn Pathol. 1994. 11:215–222.
20. Elston CW, Gresham GA, Rao GS, Zebro T, Haybittle JL, Houghton J, Kearney G. The cancer research campaign (King's/Cambridge trial for early breast cancer: clinico-pathological aspects). Br J Cancer. 1982. 45:655–669.

21. Heimann R, Hellman S. Individual characterisation of the metastatic capacity of human breast carcinoma. Eur J Cancer. 2000. 36:1631–1639.

22. Engel J, Eckel R, Kerr J, Schmidt M, Furstenberger G, Richter R, Sauer H, Senn HJ, Holzel D. The process of metastasisation for breast cancer. Eur J Cancer. 2003. 39:1794–1806.

23. Black MM, Speer FD. Nuclear structure in cancer tissues. Surg Gynecol Obstet. 1957. 105:97–102.
24. Leong AS, Sormunen RT, Vinyuvat S, Hamdani RW, Suthipintawong C. Biologic markers in ductal carcinoma in situ and concurrent infiltrating carcinoma. A comparison of eight contemporary grading systems. Am J Clin Pathol. 2001. 115:709–718.
25. Douglas-Jones AG, Gupta SK, Attanoos RL, Morgan JM, Mansel RE. A critical appraisal of six modern classifications of ductal carcinoma in situ of the breast (DCIS): correlation with grade of associated invasive carcinoma. Histopathology. 1996. 29:397–409.

26. Moreno A, Lloveras B, Figueras A, Escobedo A, Ramon JM, Sierra A, Fabra A. Ductal carcinoma in situ of the breast: correlation between histologic classifications and biologic markers. Mol Pathol. 1997. 10:1088–1092.
27. Slaughter DP, Southwick HW, Smejkal W. Field cancerization in oral stratified squamous epithelium; clinical implications of multicentric origin. Cancer. 1953. 6:963–968.

28. Van de Rijn M, Perou CM, Tibshirani R, Haas P, Kallioniemi O, Kononen J, Torhorst J, Sauter G, Zuber M, Kochli OR, Mross F, Dieterich H, Seitz R, Ross D, Botstein D, Brown P. Expression of cytokeratins 17 and 5 identifies a group of breast carcinomas with poor clinical outcome. Am J Pathol. 2002. 161:1991–1996.

29. Man YG, Tai L, Barner R, Vang R, Saenger JS, Shekitka KM, Bratthauer GL, Wheeler DT, Liang CY, Vinh TN, Strauss BL. Cell clusters overlying focally disrupted mammary myoepithelial cell layers and adjacent cells within the same duct display different immunohistochemical and genetic features: implications for tumor progression and invasion. Breast Cancer Res. 2003. 5:R231–R241.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download