Abstract
TNF-α mediated apoptosis of the hematopoietic cells has been thought to contribute to the ineffective hematopoiesis observed in myelodysplastic syndrome (MDS). The combination of pentoxifylline (P) and ciprofloxacin (C) has been shown to reduce the serum levels of TNF-α, and an earlier trial of P and C with dexamethasone (D) provided good palliation for patients with MDS. The purpose of this study is to assess the hematologic response to PCD therapy for patients suffering with MDS. 21 of 25 patients who completed at least of 12 weeks of treatment were evaluable for the treatment efficacy. At baseline, the patient's median age was 60 yr (range: 18-75 yr). The diagnoses according to WHO classification included: RA (n=5), RCMD (n=10), RARS (n=1), RCMD/RS (n=1), RAEB (3), and CMML (n=1). 11 patients (52%) had at least single lineage response. 3 patients (11%) showed improvement of triple lineage cytopenia. There were no differences in the response rates between the FAB subtypes. The median time to response was 4 weeks (range: 2-12 weeks), and it is interesting that 9 of 11 patients who had a response remained without relapse for a median of 177 days (range: 78-634 days). These preliminary results indicate that anti-cytokine therapy with PCD is an effective and well tolerated palliative treatment for patients with MDS.
Myelodysplastic syndrome (MDS) refers to a heterogenous group of acquired bone marrow disorders that is characterized by dysplastic growth of the hematopoietic progenitors, a hypercellular bone marrow with peripheral cytopenia and a propensity for these disease to progress onward to acute leukemia (1). The overproduction of the proapoptotic cytokines such as tumor necrosis factor-alpha (TNF-α), soluble Fas ligand, MIP-1α, TGF-β, IL-1β, IL-6 and interferon-gamma (IFN-γ) has been demonstrated in the bone marrow microenvironment and in the plasma of the patients with MDS, and this may contribute to the excessive apoptotic cell death observed in MDS (2, 3). TNF-α is a pleotropic immunomodulatory cytokine and a potent inhibitor of hematopoiesis; in vitro, TNF-α suppresses colony formation and the proliferation of normal hematopoietic progenitor cells and the malignant hematopoietic cell lines (4-7). Further, neutralization of TNF-α enhances the outgrowth of the hematopoietic progenitor cells in MDS (8). Elevation of the plasma TNF-α level correlates with oxidative DNA injury and depletion of cellular glutathione in CD34+ cells, as well as caspase-3 activity (9, 10). These findings support an effector or potentiating role for these cytokines in the ineffective hematopoiesis of MDS.
Pentoxifylline is known to interfere with the lipid-signaling pathway used by TNF-α, TGF-β and IL-1β, and it reduces the activity of these cytokines. Ciprofloxacin is known to reduce the hepatic metabolism of pentoxifylline and dexametasone, and it down-regulates the translation of the mRNA for TNF-α (11, 12).
Pentoxifylline, ciprofloxacine and dexamethasone (PCD) therapy induced positive hematologic responses in 18 of 43 patients with MDS. The mechanism of action was found to be cytokine related by the the fact that the responders showed a sustained reduction of their TNF-α levels (12). The purpose of this study was to verify the response rate and the toxicity profile for the PCD therapy that was observed in the first study by Raza (12).
From April 2002 to December 2003, 17 female patients and 8 male patients with untreated MDS were enrolled in this study. The diagnosis of MDS was established based on the characteristic morphological abnormalities in the bone marrow and/or by the presence of cytogenetic abnormalities and peripheral cytopenia: all the patients were subclassified according to both the French-American-British (FAB) nomenclature and the WHO classification scheme (13-15). The study protocol was reviewed and approved by the Institutional Review Boards of the Yeungnam University Medical Center and Daegu Catholic University Hospital. All the patients provided us with a written informed consent.
Twenty-one of 25 patients completed at least 12 weeks of treatment, and so 21 patients are finally evaluable for the treatment efficacy.
The patients were treated with 1,200 mg of pentoxifylline (P) that was divided into three doses per day, 500 mg of ciprofloxacin (C) that was divided into two doses per day, and 4 mg of dexamethasone (D) that was divided into two daily doses, and this combined treatment was given for 4 weeks. After this 4-week course, P 800 mg and C 500 mg were given 3 times a week with 4 mg of D being given for 5 days every month for 2 months. The therapy was stopped for the nonresponding patients at this time and they were taken off the study. The protocol called for continuing all the drugs for 1 yr for the responders if the side effects were tolerable and the responses were persistently observed.
The complete blood counts with differentials were obtained every week for all the patients. The hematologic response was evaluated using the International Working Group criteria (16).
The erythroid response (HI-E) was classified as follows: a major response was defined for those patients with a pretreatment hemoglobin level less than 11 g/dL as greater than a 2 g/dL increase in their hemoglobin level; for the RBC transfusion-dependent patients, a major response was independence from RBC transfusions. A minor response was defined for those patients with a pretreatment hemoglobin level less than 11 g/dL as a 1 to 2 g/dL increase in their hemoglobin level; for the RBC transfusion-dependent patients, a major response was a 50% decrease in the transfusion requirement.
The platelet response (HI-P) was identified as follows: a major response for patients with a pretreatment platelet count of less than 100,000/µL was defined as an absolute increase of 30,000/µL or more; for the platelet transfusion-dependent patients, a major response was defined as stabilization of the platelet counts and independence from platelet transfusion. A minor response was defined for patients with a pretreatment platelet count of less than 100,000/µL as a 50% or more increase in the platelet count with a net increase greater than 10,000/µL, but less than 30,000/µL.
The neutrophil response (HI-N) was classified as follows: a major response was defined for the patients with an absolute neutrophil count (ANC) less than 1,500/µL before therapy as at least a 100% increase or an absolute increase of more than 500/µL. A minor response was defined for patients with an ANC less than 1,500/µL before therapy as an ANC increase of at least 100%, but an absolute increase less than 500/µL.
To be considered as a major or minor improvement, the hematologic improvements must have lasted for at least 2 months in the absence of ongoing cytotoxic therapy.
Karyotypic analysis using GTG banding was initially performed for every patient by using unstimulated 24 hr cultures and/or methotrexate-thymidine synchronized cultures.
Paired t-tests were used for 2 sample comparisons of the continuous variables. The comparisons of the categorical variables were performed by using χ2-tests or Fisher's exact tests as appropriate. All the tests were two-sided and the p-values less than 5% were considered statistically significant. The analyses were performed using SPSS for Windows version 12.0 (SPSS Inc., Chicago, IL, U.S.A.).
Of the 25 patients enrolled in this study, 1 patient died of sepsis immediately after registration to this study, and 1 other patient was registered, but that patient could not keep taking the medication due to a concomitant herniated cervical disc that required an operation. Of the 23 patients who were evaluable for toxicity, 2 patients prematurely stopped their therapy because of intolerable nausea and epigastric sores, respectively.
Twenty-one patients completed at least a 12-week course of therapy and so they were evaluable for a response to treatment. The patients' demographics and baseline disease characteristics are summarized in Table 1.
The hematologic improvement (HI) is summarized in Table 2 and the individual patient data and their baseline characteristics are listed in Table 3. The median time to response varied depending upon the nature of the response: the median time to response was 4 weeks for HI-E (range; 2-8 weeks), 6 weeks for HI-P (range; 2-8 weeks), and 3 weeks for HI-N (range; 2-16 weeks). Fig. 1, 2, and 3 depicts the serial hemoglobin levels, the RBC requirements, the platelet counts and the neutrophil counts for the responding patients. With the exception of the patient 8, whose disease progressed on to acute myelogenous leukemia at 8.2 months after PCD therapy, the other 10 responding patients were still responding at the time of analysis. Therefore the median duration of response was not reached with a range of 3.6-20.9 months.
Of the 23 patients who could be evaluated for drug toxicities, 39% of the patients experienced some type of toxicities, and 2 patients discontinued their therapy prematurely because of their intolerable epigastric sores and nausea, respectively. However there was no grade 3 or worse severe toxicities, and the treatment was relatively well tolerated (Table 4). Although we were concerned about infectious complications due to the long term steroid therapy, there was no significant incidence of infection.
The platelet responders had a shorter disease duration (p=0.03) and they had a tendency for higher pretreatment neutrophil, hemoglobin and platelet counts (p=0.19, 0.06 and 0.19 respectively). The RBC responders had a trend of a better karyotype risk (p=0.17), and the neutrophil responders had a tendency for a lower international prognostic scoring system (IPSS) (p=0.25) (Table 5).
Since TNF-α may be the proximal inhibitor of a variety of proinflammatory cytokines, those treatment strategies that have employed a number of therapeutic agents with anti-TNF properties such as amifostine, pentoxyphylline-ciprofloxacin-dexamethasone, thalidomide, soluble tumor necrosis factor-α receptor and monoclonal anti-TNF antibody have been conducted with varying degree of success (17-24). Based on these previous results, we evaluated an experimental regimen that consisted of modified doses of pentoxifylline (P), ciprofloxacin (C) and dexamethasone (D) in an attempt to improve the toxicity profile and to maintain the treatment efficacy for myelodysplastic syndrome. The results of this trial are summarized as follows: Of the 21 evaluable patients, eleven patients (52%) showed an improvement of their cytopenia. 3 patients had a triple lineage response, 1 patient had a dual lineage response, and 7 patients had a single lineage response. No differences were noted for the response rates among the 3 lineages. There were no differences in the response rates between the FAB subtypes, but the responders had a shorter disease duration and a tendency for higher pretreatment neutrophil, hemoglobin and platelet counts, a better karyotype risk and a lower IPSS. These findings are similar to the results of the other anti-cytokine therapies (17, 23).
The mechanism of the treatment response is thought to involve the suppression of the proinflammatory cytokines such as TNF-α, with the consequent suppression of apoptosis in the hematopoietic cells, and there is a resultant regression of the MDS clones and stimulation of hematopoiesis in the normal cells (21). Yet in some studies that have used soluble TNF-α, the clinical response rate was low and there was no correlation between the level of TNF-α production and any of the clinical parameters or features of MDS (22). This result may suggest that the apoptotic pathways in MDS are redundant and they are mediated by many cytokines with overlapping specificities, or that the dosage, duration of therapy and frequency of administration may not have been optimal. More recently, one study has reported a 20-38% response rate when using an anti-TNF monoclonal antibody, Remicade (24).
Meanwhile, in addition to the standard chemotherapeutic drugs, a variety of novel agents like decitabine, Mylotarg, farnesyl transferase inhibitors and arsenic have been employed in attempt to eliminate the MDS clones. While each strategy has produced important clinical responses for some of the patient subset, none of these strategies is of universal benefit for all MDS patients (25-27). The nucleoside analogues 5-azacytidine have activity both as a DNA methyltransferase inhibitor and as a cytotoxic agent, and the patients treated with this drug have shown a 60% response rate and a survival benefit over the best supportive care for patients with MDS (28).
There are several limitations to our study. First of all, the use of multiple agents precluded a precise dissection of the mechanism of response, and another limitation was that the TNF-α concentrations were not measured. Thus, whether the hematologic improvements we observed were a direct result of the anti-TNF effect of the PCD therapy remains uncertain. Still another limitation was that the clinical benefit and the improvement of the quality of life after treatment were not assessed.
Since the therapy was well tolerated, it is worthwhile to consider a combination therapy with an agent that directly affects the MDS cell clones such as topotecan, arsenic trioxide, farnesyl-transferase inhibitor, 5-azacytidine or decitabine.
In conclusion, these preliminary results indicate that anti-cytokine therapy with PCD is well tolerated for patients with MDS. Although this approach may not prove to be wholly curative in the long run, it provides substantial palliative support for at least some of the MDS patients.
Figures and Tables
Fig. 1
Graphic presentation of the hemoglobin levels and RBC requirements for the patients with a RBC response after PCD treatment.
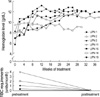
Fig. 2
Graphic presentation of the platelet levels for the patients with a platelet response after PCD treatment.
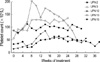
Fig. 3
Graphic presentation of the neutrophil levels for the patients with a neutrophil response after PCD treatment.

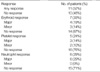
Table 1
The patients' demographics and baseline characteristics (n=21)

*Good, normal, -Y, del(5q), del(20q); Poor, complex (≥3 abnormalities) or chromosome 7 abnormalities; Intermediate, other abnormalities.
RA, refractory anemia; RCMD, refractory cytopenia with multilineage dysplasia; RARS, refractory anemia with ringed sideroblasts; RCMD-RS, refractory cytopenia with multilineage dysplasia with ringed sideroblasts; CMML, chronic myelomonocytic leukemia; MDS/MPD, myelodysplastic/myeloproliperative disease; IPSS, international prognostic scoring system; ANC, absolute neutrophil count.
References
2. Gersuk GM, Beckham C, Loken MR, Kiener P, Anderson JE, Farrand A, Troutt AB, Ledbetter JA, Deeg HJ. A role for tumour necrosis factor-alpha, Fas and Fas-Ligand in marrow failure associated with myelodysplastic syndrome. Br J Haematol. 1998. 103:176–188.
4. Broxmeyer HE, Williams DE, Lu L, Cooper S, Anderson SL, Beyer GS, Hoffman R, Rubin BY. The suppressive influences of human tumor necrosis factors on bone marrow hematopoietic progenitor cells from normal donors and patients with leukemia: synergism of tumor necrosis factor and interferon-gamma. J Immunol. 1986. 136:4487–4495.
5. Roodman GD, Bird A, Hutzler D, Montgomery W. Tumor necrosis factor-alpha and hematopoietic progenitors: effects of tumor necrosis factor on the growth of erythroid progenitors CFU-E and BFU-E and the hematopoietic cell lines K562, HL60, and HEL cells. Exp Hematol. 1987. 15:928–935.
6. Means RT Jr, Krantz SB. Inhibition of human erythroid colony-forming units by tumor necrosis factor requires beta interferon. J Clin Invest. 1993. 91:416–419.

7. Sato T, Selleri C, Anderson S, Young NS, Maciejewski JP. Expression and modulation of cellular receptors for interferon-gamma, tumour necrosis factor, and Fas on human bone marrow CD34+ cells. Br J Haematol. 1997. 97:356–365.
8. Sawanobori M, Yamaguchi S, Hasegawa M, Inoue M, Suzuki K, Kamiyama R, Hirokawa K, Kitagawa M. Expression of TNF receptors and related signaling molecules in the bone marrow from patients with myelodysplastic syndromes. Leuk Res. 2003. 27:583–591.

9. Mundle SD, Reza S, Ali A, Mativi Y, Shetty V, Venugopal P, Gregory SA, Raza A. Correlation of tumor necrosis factor alpha (TNF alpha) with high Caspase 3-like activity in myelodysplastic syndromes. Cancer Lett. 1999. 140:201–207.
10. Peddie CM, Wolf CR, McLellan LI, Collins AR, Bowen DT. Oxidative DNA damage in CD34+ myelodysplastic cells is associated with intracellular redox changes and elevated plasma tumour necrosis factor-alpha concentration. Br J Haematol. 1997. 99:625–631.
11. Raza A, Venugopal P, Genzer S. Hiddemann W, Buchner T, Wormann B, editors. Pilot study of pentoxifylline and ciprofloxacin with or without dexamethasone produces encouraging results in myelodysplastic syndromes: acute leukemias VII. Experimental Approaches and Novel Therapies. 1998. New York: Springer-Verlag;42–51.
12. Raza A. Anti-TNF therapies in rheumatoid arthritis, Crohn's disease, sepsis, and myelodysplastic syndromes. Microsc Res Tech. 2000. 50:229–235.

13. Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982. 51:189–199.

14. Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J, Lister TA, Bloomfield CD. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting-Airlie House, Virginia, November 1997. J Clin Oncol. 1999. 17:3835–3849.

15. Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, Sanz M, Vallespi T, Hamblin T, Oscier D, Ohyashiki K, Toyama K, Aul C, Mufti G, Bennett J. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997. 89:2079–2088.

16. Cheson BD, Bennett JM, Kantarjian H, Pinto A, Schiffer CA, Nimer SD, Lowenberg B, Beran M, de Witte TM, Stone RM, Mittelman M, Sanz GF, Wijermans PW, Gore S, Greenberg PL. World Health Organization (WHO) international working group. Report of an international working group to standardize response criteria for myelodysplastic syndromes. Blood. 2000. 96:3671–3674.
17. Raza A, Meyer P, Dutt D, Zorat F, Lisak L, Nascimben F, du Randt M, Kaspar C, Goldberg C, Loew J, Dar S, Gezer S, Venugopal P, Zeldis J. Thalidomide produces transfusion independence in long-standing refractory anemias of patients with myelodysplastic syndromes. Blood. 2001. 98:958–965.

18. List AF, Brasfield F, Heaton R, Glinsmann-Gibson B, Crook L, Taetle R, Capizzi R. Stimulation of hematopoiesis by amifostine in patients with myelodysplastic syndrome. Blood. 1997. 90:3364–3369.

19. Deeg HJ, Gotlib J, Beckham C, Dugan K, Holmberg L, Schubert M, Appelbaum F, Greenberg P. Soluble TNF receptor fusion protein (etanercept) for the treatment of myelodysplastic syndrome: a pilot study. Leukemia. 2002. 16:162–164.

20. Raza A, Qawi H, Andric T, Dar S, Lisak L, Huang RW, Venugopal P, Gezer S, Gregory SA, Hsu WT, Loew J, Robin E, Rifkin S, Shah R, Divgi A, Taylor R, Grosset A. Pentoxifylline, ciprofloxacin and dexamethasone improve the ineffective hematopoiesis in myelodysplastic syndrome patients; malignancy. Hematology. 2000. 5:275–284.
21. Raza A, Qawi H, Lisak L, Andric T, Dar S, Andrews C, Venugopal P, Gezer S, Gregory S, Loew J, Robin E, Rifkin S, Hsu WT, Huang RW. Patients with myelodysplastic syndromes benefit from palliative therapy with amifostine, pentoxifylline, and ciprofloxacin with or without dexamethasone. Blood. 2000. 95:1580–1587.

22. Maciejewski JP, Risitano AM, Sloand EM, Wisch L, Geller N, Barrett JA, Young NS. A pilot study of the recombinant soluble human tumour necrosis factor receptor (p75)-Fc fusion protein in patients with myelodysplastic syndrome. Br J Haematol. 2002. 117:119–126.

23. Deeg HJ, Jiang PY, Holmberg LA, Scott B, Petersdorf EW, Appelbaum FR. Hematologic responses of patients with MDS to antithymocyte globulin plus etanercept correlate with improved flow scores of marrow cells. Leuk Res. 2004. 28:1177–1180.
24. Raza A, Candoni A, Khan U, Lisak L, Tahir S, Silvestri F, Billmeier J, Alvi MI, Mumtaz M, Gezer S, Venugopal P, Reddy P, Galili N. Remicade as TNF suppressor in patients with myelodysplastic syndromes. Leuk Lymphoma. 2004. 45:2099–2104.

25. Daskalakis M, Nguyen TT, Nguyen C, Guldberg P, Kohler G, Wijermans P, Jones PA, Lubbert M. Demethylation of a hypermethylated P15/INK4B gene in patients with myelodysplastic syndrome by 5-Aza-2'-deoxycytidine (decitabine) treatment. Blood. 2002. 100:2957–2964.

26. Kurzrock R, Albitar M, Cortes JE, Estey EH, Faderl SH, Garcia-Manero G, Thomas DA, Giles FJ, Ryback ME, Thibault A, De Porre P, Kantarjian HM. Phase II study of R115777, a farnesyl transferase inhibitor, in myelodysplastic syndrome. J Clin Oncol. 2004. 22:1287–1292.

27. List A, Beran M, DiPersio J, Slack J, Vey N, Rosenfeld CS, Greenberg P. Opportunities for Trisenox (arsenic trioxide) in the treatment of myelodysplastic syndromes. Leukemia. 2003. 17:1499–1507.

28. Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R, Stone RM, Nelson D, Powell BL, DeCastro CM, Ellerton J, Larson RA, Schiffer CA, Holland JF. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol. 2002. 20:2429–2440.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download