Abstract
A few cases of laparoscopic surgery for urachal remnant in children has been reported in English literature. With recent developments in minimal invasive surgery, laparoscopic approach for urachal remnant in adulthood is recommended by some laparoscopic surgeons because of its technical feasibility and safety as well as cosmesis. Recently we experienced a case of complicated urachal remnant in a 14-month-old girl, who was managed by laparoscopic approach. At presentation, she complained of high fever and lower urinary tract symptoms. After 6 weeks of antibiotics therapy, laparoscopic surgery was performed transperitoneally via 3 ports. Our experience suggests that laparoscopic excision of urachal remnant can be performed easily and safely in children.
Urachus is a vestigial fibrous cord which lies between the peritoneum and transversalis fascia. Progressive fetal development that is accompanied with bladder descent usually results in the complete obliteration of the urachus shortly after birth. The surgical management of urachal remnant is generally reserved for complications, especially in children.
Standard surgical management of benign urachal disease in children is known as the radical excision of all anomalous tissue with or without a cuff of bladder via hypogastric transverse or midline vertical incision. Laparoscopic approach to the complete excision of urachal abnormalities in adults has recently been advocated by some groups, but little has been reported in the pediatric literature (1-3). Recently we experienced a case of complicated urachal remnant in a child, which was managed efficaciously by laparoscopic approach.
A 14-month-old girl presented with high fever, markedly distended abdomen and painful urination. She has been under prescribed medication for several days by the primary physician, who diagnosed her as low urinary tract infection. The redness and swelling which were inspected on the skin below umbilicus were palpated as a tender mass on physical examination.
At presentation, she revealed a marked leukocytosis and pus discharge from the abscess. Staphylococcus aureus was identified from the pus culture. Other laboratory findings including urinalysis were normal. Abdominal ultrasonography and subsequent computed tomography revealed a 4×2.5 cm sized cystic mass within anterior abdominal wall, which was considered as a complicated abscess underlying urachal remnant (Fig. 1).
After immediate catheter drainage, cystography confirmed non-communication between the bladder dome and urachal remnant. She was managed with antibiotics for 6 weeks, and then the radical excision of urachal remnant via laparoscopic approach was followed.
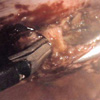
Under general anesthesia with supine position, we performed radical excision of urachal remnant through 3 ports; a, 10 mm camera port and the other two, 5 mm working ports. The camera port was placed in the midline a few centimeters caudal to the end of xiphoid process via open Hasson technique and a 30-degree telescope was inserted into the camera port. Under direct visualization after CO2 insufflation, 2 working ports were also inserted in each upper quadrant (Fig. 2).
Urachal remnant was found easily below umblicus. Except adhesions between anterior abdominal wall and omentum, other intraperitoneal findings were normal. The operative time was 130 min and no intraoperative complications occurred.
Urachus is a vestigial structure arising from the anterior bladder wall and extending cranially to the umbilicus within the extraperitoneal fat between the peritoneum and transversalis fascia. Embryologically, the urachus is said to arise as a result of the separation of the allantois from the ventral cloaca during the mid-trimester (4, 5). Normally urachus becomes progressively obliterated with advancing age, but in some patients the obliteration of urachus may fail and result in 4 different types of urachal remnants; patent urachus, vesicourachal diverticulum, urachal sinus and urachal cyst. Urachal cyst, the most common anomaly, occurs in approximately 1/5,000 births (6).
Although urachal anomaly is usually asymptomatic, they occasionally warrant intervention when infected and symptomatic. Especially, if the infection of urachal remnant result in the formation of abscess cavity, the use of broad spectrum antibiotics followed by staged removal of the remnant is warranted (7). Drainage only can be inadequate because the recurrence rate reaches 30 percent and the patient may face a risk of adenocarcinoma in the unresected remnant, although the incidence is extremely low (8). Actually, urachal carcinoma occurs most often at the junction of the urachal ligament and bladder dome (9) and are believed to originate either from enteric rests during embryological development or from metaplasia of the urachal ligament (10). Therefore the surgical management warrants to be performed through the radical excision of urachal remnant including the urachus and medial umbilical ligaments as well as the adjacent peritoneum from umbilicus to bladder dome with or without a cuff of bladder wall.
So far the traditional approach to the total excision of urachal lesions has been via hypogastric transverse or midline vertical incision. As the advancement of technique and experience of laparoscopic surgery, some groups have advocated laparoscopic approach for the complete excision of urachal abnormalities in adults. Also Khurana and Borzi described successful results of laparoscopic approach for the radical excision of urachal remnants in an infant. However, they reported that the role of laparoscopic surgery in children has not yet been well established, therefore more reports will be needed to establish its role (11).
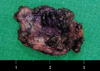
Before laparoscopic surgery, we stained the lumen of urachal abscess cavity with gentian violet through drainage catheter before inserting the ports. This procedure facilitated the identification of the urachus and surgical margin for complete removal. Actually we could identify purple-stained urachus easily under direct vision (Fig. 3). The operative procedure was started from the umbilicus to bladder base and first incision of peritoneum beneath umbilicus was performed after identifying the exact site through the penetration of needle into umbilicus. Pre-operative evaluation revealed a non-communication between the urachus and bladder, so we did not perform the resection of bladder cuff. During operation, intraabdominal pressure was maintained at 12 mmHg and venous return was not impaired. Also the sinus tract between abscess cavity and umbilicus was identified with ease (Fig. 4) and could be excised almost completely (Fig. 5). But relatively longer operative time when comparing to the open approach may be disadvantageous.
Although laparoscopic surgery for a complicated urachal remnant in children is not yet advocated unlike in adults, it may justify as the standard therapy if more cases are reported.
Our experience revealed the feasibility and safety of laparoscopic excision of complicated urachal remnant in children.
Figures and Tables
References
1. Siegel JF, Winfield HN, Valderrama E, Smith AD. Laparoscopic excision of a urachal cyst. J Urol. 1994. 151:1631–1633.
2. Stone NN, Garden RJ, Weber H. Laparoscopic excision of a urachal cyst. Urology. 1995. 45:161–164.

3. Cadeddu JA, Boyle KE, Fabrizio MD, Schulam PG, Kavoussi LR. Laparoscopic management of urachal cysts in adulthood. J Urol. 2000. 164:1526–1528.

4. Bauer SB, Retik AB. Urachal anomalies and related umbilical disorders. Urol Clin North Am. 1978. 5:195–211.

5. Scheye T, Vanneuville G, Amara B, Francannet P, Dechelotte P, Campagne D. Anatomic basis of pathology of the urachus. Surg Radiol Anat. 1994. 16:135–141.

6. Berman SM, Tolia BM, Laor E, Reid RE, Schweizerhof SP, Freed SZ. Urachal remnants in adults. Urology. 1988. 31:17–21.

7. Goldman IL, Caldamone AA, Gauderer M, Hampel N, Wesselhoeft CW, Elder JS. Infected urachal cysts: a review of 10 cases. J Urol. 1988. 140:375–378.

8. Blichert-Toft M, Nielsen OV. Diseases of the urachus simulating intra-abdominal disorders. Am J Surg. 1971. 122:123–128.

9. Henly DR, Farrow GM, Zincke H. Urachal cancer: role of conservative surgery. Urology. 1993. 42:635–639.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download