Abstract
During a four-week period, four healthy term newborn infants born at a regional maternity hospital in Korea developed late-onset neonatal group B Streptococcus (GBS) infections, after being discharged from the same nursery. More than 10 days after their discharge, all of the infants developed fever, lethargy, and poor feeding behavior, and were subsequently admitted to the Korea University Medical Center, Ansan Hospital. GBS was isolated from the blood cultures of three babies; furthermore, GBS was isolated from 2 cerebral spinal fluid cultures. Three babies had meningitis, and GBS was isolated from their cerebral spinal fluid cultures. This outbreak was believed to reflect delayed infection after early colonization, originating from nosocomial sources within the hospital environment. This report underlines the necessity for Korean obstetricians and pediatricians to be aware of the risk of nosocomial transmissions of GBS infection in the delivery room and/or the nursery.
Group B streptococcus (GBS), also known as Streptococcus agalactiae, constitutes one of the leading pathogens associated with both early and late-onset neonatal sepsis (1, 2). Early-onset sepsis is normally related to vaginal carriage in the mother, and subsequent vertical transmission during birth. The origin of late-onset disease remains less clear. It is believed to be transmitted both vertically and horizontally, from maternal and nosocomial sources, and resulted in persistent colonization.
During a four-week period, four healthy term newborn infants, all of whom were born at the same regional maternity hospital in Korea, developed late-onset neonatal GBS infections, after being discharged from the same nursery. This outbreak was believed to reflect delayed infection after early colonization, originating from nosocomial sources within the delivery room and/or the nursery.
To our knowledge, this outbreak represents the first documented nosocomial transmission of GBS infections in healthy newborn infants born at the same maternity hospital in Korea.
Between 14 March and 10 April 2002, four healthy newborn infants, all of whom had been born at the same regional maternity hospital, and had developed late-onset neonatal GBS infections while at home, were admitted to the Korea University Medical Center, Ansan Hospital. The medical charts of these infants were reviewed, and demographic, clinical, and microbiological data were collected.
This presumedly nosocomial outbreak occurred in a regional maternity hospital, located in Ansan City. This maternity hospital logged about 600 total deliveries in 2002. The average length of nursery stay was reported to be 3 days (6 days for babies delivered by cesarean section). All premature or sick babies were routinely referred to a tertiary care hospital.
All infants were less than 1 month of age, and had been delivered and cared for in the same hospital. Their mothers' obstetric histories were unremarkable, and the current pregnancies had been otherwise uncomplicated. There was no history, in any of the patients, of premature rupture of the amniotic membrane more than 12 hr before delivery. In addition, we found no histories indicative of consanguinity, structural anomalies, or genetic disorders on either side of any of the families. After delivery, all infants were cared for in the same newborn nursery. However the duration of stay of the infants did not overlap each other. Either 3 or 6 days after birth, these infants were discharged from the same newborn nursery, and all appeared normal and healthy at the time of discharge.
More than 10 days after their discharge, however, all of the infants developed fever, lethargy, and poor feeding behavior, and were subsequently admitted to the general pediatric ward of our hospital. One infant experienced generalized seizure and mild respiratory difficulty, but no infants exhibited symptoms necessitating intensive care.
The time course of the outbreak is illustrated in Fig. 1. None of the infants were matched in the hospital. All cases exhibited a late-onset of the disease, occurring after 7 days after birth.
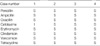
Demographic, clinical, and laboratory findings in these patients are summarized in Table 1. Fever and lethargy with refusal to feed constitute the principal presenting features. Three babies were determined to have leukopenia (total WBC count <5,000/µL) and one had a total WBC count of 27,700/µL. GBS was isolated from the blood cultures of 3 babies; furthermore, GBS was isolated from 2 cerebral spinal fluid cultures. Three babies had meningitis, and GBS was isolated from their cerebral spinal fluid cultures.
All GBS isolates proved to be sensitive to penicillin, cefotaxime, and erythromycin, and exhibited the same antibiotic susceptibility patterns (Table 2).
When GBS infection had been confirmed in the infants, we tested maternal vaginal swabs, which were collected about 1 month after delivery, and all tested negative for GBS. Although no maternal breast milk cultures were taken, we found no clinical evidence of mastitis. One baby was not fed on breast milk.
All infants were treated with ampicillin, coupled with either gentamicin or cefotaxime, for at least 20 days. There were no deaths related to this outbreak, and all infections were successfully resolved. However, the Case 1 infant, who had exhibited generalized seizures and mild respiratory difficulty upon admission, was also found to be suffering from encephalomalacia. A brain MRI, taken on the 36th day after birth, revealed lacunar infarction and lamina hemorrhage in the right frontal and temporal lobes. The remainder of the infant's hospital course was uncomplicated.
After the inception of infection control procedures at the maternity hospital, no further cases of GBS have occurred in the past 2 yr since the last case.
GBS remains the most important pathogen which causes neonatal invasive infections in developed countries, despite the great improvements achieved by maternal antimicrobial prophylaxis programs. Furthermore, preterm delivery or late-onset sepsis cannot be completely prevented, and emerging antibiotic resistance has become a major concern in developed countries (3, 4).
In Korea, the estimated incidence of neonatal GBS infection has been much lower than in other developed and developing countries (5), due to the low prevalence rate of GBS colonization in pregnant women, resulting in low rates of early-onset neonatal GBS infection (6, 7). However, GBS is known to be a leading cause of neonatal sepsis and meningitis, and is associated with significant morbidity and mortality during the neonatal period in Korea. In addition, recent reports (8, 9) have indicated that late-onset disease (more than seven days after birth) accounts for 84-93% of neonatal invasive GBS infections in Korea.
The pathogenesis of late-onset disease remains less clear. Late-onset disease is believed to reflect delayed infection after early colonization, due to either vertical or horizontal transmission. In our cases, early colonization within the mother's genital tract is less likely, as there appeared to be no maternal carriage of GBS. The presence of GBS in the maternal genital tract at delivery is a significant determinant of colonization and infection in neonates. Exposure of neonates to this organism can occur either by the ascending route, in utero through ruptured membranes, or via contamination during passage through the birth canal (10, 11). In our reports, although maternal vaginal swabs were taken about 1 month after delivery, the results of all of the bacterial cultures proved to be negative.
Besides vertical transmission, other sources of GBS colonization in neonates have been established. Horizontal transmission from hospital (12-16) or community (15, 16) sources to neonates is one of the predominant modes for the transmission of infection. Cross-contamination from maternally infected to uninfected neonates can occur from the hands of nursery personnel. An epidemic report (17) of late-onset sepsis due to type Ib/c GBS sepsis in a neonatal intensive care unit revealed that none of the index cases had been colonized at birth, establishing that nosocomial acquisition was responsible. Their epidemiologic analysis suggested infant-to-infant spread via the hands of medical/healthcare personnel, but acquisition from two nurses who had been colonized by the same serotype Ib/c GBS strain was not excluded. This and other reports (18-20) have indicated that, during an outbreak, cohorting of culture-positive infants and enforced hand washing and gloving before any infant contact significantly diminish the rates of nosocomial acquisition.
Another potential source for GBS transmission to the neonate is community acquisition. Indirect evidence suggests that this acquisition of GBS by uncolonized infants occurs only very infrequently (16-18, 21). Gardner and colleagues (22) determined that only 2 out of 46 (4.6%) neonates who had tested culture-negative for GBS when discharged from the newborn nursery had acquired mucous membrane infections, at 6 to 8 weeks of age.
Whether the organism is acquired via vertical or horizontal transmission, infants who are asymptomatically colonized often experience persistent GBS infection at mucous membrane sites for weeks or months, after which time, delayed infection occurs (16, 19, 23). The epidemiology and pathogenesis of GBS infection occurring beyond the first week of life remain less well defined than they are for early-onset disease. Although serotype III strains, which account for the majority of isolates obtained from infants with late-onset infection, must be uniquely virulent for the infant between 8 days and 3 months of age, the virulence factors in these organisms, as well as the specific host defense mechanisms have yet to be completely elucidated.
The route of transmission in the outbreak described here could not be defined precisely, as the infection control measures at the regional maternity hospital were not properly performed at the time during which the outbreak occurred. However, the hospital personnel of the maternity hospital were urged to keep a strict regimen of infection control procedures, including hand washing, sterilization, decontamination and cleaning techniques, as well as aseptic techniques for invasive procedures. These general practices were designed to prevent further spread of GBS in the hospital. This fact strongly indicates that the infants had been infected during admittance to the hospital, as the result of nosocomial cross-contamination. In many instances, these general infection control procedures can disrupt an outbreak before the source has even been identified (24, 25).
As shown in our case, neonatal GBS infections, which are normally quite rare in Korea, were documented after patients had been discharged from the same hospital, and the fact that same organisms isolated from the four infants exhibited the same antibiotic susceptibility pattern, this outbreak was most likely due to nosocomial cross-infection, which culminated in late-onset infection in the healthy newborn infants.
Consequently, hospital personnel should be very aware of their potential to spread nosocomial pathogens in the hospital environment, and should implement Centers for Disease Control and Prevention (CDC) recommendations for hospital infection control, in order to reduce the incidence of nosocomial infection.
Figures and Tables
Fig. 1
Time courses of outbreak between nursery stay and hospital admission. Black arrows indicate the onset of symptoms at home.

ACKNOWLEDGMENT
The authors thank the physicians and nursing staff working in the pediatric general ward of Korea University Medical Center Ansan Hospital, for their cooperation and support.
References
1. Berner R. Group B streptococci during pregnancy and infancy. Curr Opin Infect Dis. 2002. 15:307–313.

2. Gladstone IM, Ehrenkranz RA, Edberg SC, Baltimore RS. A ten-year review of neonatal sepsis and comparison with the previous fifty-year experience. Pediatr Infect Dis J. 1990. 9:819–825.

3. Schrag SJ, Zywicki S, Farley MM, Reingold AL, Harrison LH, Lefkowitz LB, Hadler JL, Danila R, Cieslak PR, Schuchat A. Group B streptococcal disease in the era of intrapartum antibiotic prophylaxis. N Engl J Med. 2000. 342:15–20.

4. Arisoy AS, Altinisik B, Tunger O, Kurutepe S, Ispahi C. Maternal carriage and antimicrobial resistance profile of group B Streptococcus. Infection. 2003. 31:244–246.
5. Kim KA, Shin SM, Choi JH. A nationwide survey on the causative organisms of neonatal sepsis in Korea. J Korean Pediatr Soc. 2002. 45:55–63.
6. Kim TH, Park SE, Kim KH. A study of group B streptococcal infection in pregnant women, by LIM broth media. Korean J Pediatr. 2004. 47:1072–1075.
7. Choi KU, Koh SK, Lee JY, Park JH, Hwang SO, Lee BI, Lee WY. Clinical significance of group B streptococcal infection in pregnant women. Korean J Obstet Gynecol. 2002. 45:811–815.
8. Lee JH, Kim SM, Lee HS, Kim SY, Choi SD, Sung IK, Kang JH, Chun CS. A clinical study of group B streptococcal infection: Five years experience. J Korean Soc Neonatol. 2003. 10:226–234.
9. Lee SY, You SJ, Kim DS, Ko TS. Clinical study of group B beta-hemolytic streptococcal meningitis. J Korean Pediatr Soc. 2003. 46:1224–1229.
10. Dillon HC Jr, Khare S, Gray BM. Group B streptococcal carriage and disease: a 6-year prospective study. J Pediatr. 1987. 110:31–36.

11. Jones DE, Kanarek KS, Lim DV. Group B streptococcal colonization patterns in mothers and their infants. J Clin Microbiol. 1984. 20:438–440.

12. Aber RC, Allen N, Howell JT, Wilkenson HW, Facklam RR. Nosocomial transmission of group B streptococci. Pediatrics. 1976. 58:346–353.
13. Easmon CS, Hastings MJ, Blowers A, Bloxham B, Deeley J, Marwood R, Rivers RP, Stringer J. Epidemiology of group B streptococci: one year's experience in an obstetric and special care baby unit. Br J Obstet Gynaecol. 1983. 90:241–246.

14. Gerards LJ, Cats BP, Hoogkamp-Korstanje JA. Early neonatal group B streptococcal disease: degree of colonisation as an important determinant. J Infect. 1985. 11:119–124.

15. Anthony BF, Okada DM, Hobel CJ. Epidemiology of the group B streptococcus: maternal and nosocomial sources for infant acquisitions. J Pediatr. 1979. 95:431–436.

16. Paredes A, Wong P, Mason EO Jr, Taber LH, Barrett FF. Nosocomial transmission of group B Streptococci in a newborn nursery. Pediatrics. 1977. 59:679–682.
17. Noya FJ, Rench MA, Metzger TG, Colman G, Naidoo J, Baker CJ. Unusual occurrence of an epidemic of type Ib/c group B streptococcal sepsis in a neonatal intensive care unit. J Infect Dis. 1987. 155:1135–1144.

18. Easmon CS, Hastings MJ, Clare AJ, Bloxham B, Marwood R, Rivers RP, Stringer J. Nosocomial transmission of group B streptococci. Br Med J. 1981. 283:459–461.

19. Band JD, Clegg HW 2nd, Hayes PS, Facklam RR, Stringer J, Dixon RE. Transmission of group B streptococci. Traced by use of multiple epidemiologic markers. Am J Dis Child. 1981. 135:355–358.
20. Steere AC, Aber RC, Warford LR, Murphy KE, Feeley JC, Hayes PS, Wilkinson HW, Facklam RR. Possible nosocomial transmission of group B streptococci in a newborn nursery. J Pediatr. 1975. 87:784–787.

21. Yow MD, Leeds LJ, Thompson PK, Mason EO Jr, Clark DJ, Beachler CW. The natural history of group B streptococcal colonization in the pregnant woman and her offspring. I. Colonization studies. Am J Obstet Gynecol. 1980. 137:34–38.
22. Gardner SE, Mason EO Jr, Yow MD. Community acquisition of group B Streptococcus by infants of colonized mothers. Pediatrics. 1980. 66:873–875.
23. Wald ER, Snyder MJ, Gutberlet RL. Group B beta-hemolytic streptococcal colonization. Acquisition, persistence, and effect of umbilical cord treatment with triple dye. Am J Dis Child. 1977. 131:178–180.
24. Moore DL. Mayhall CG, editor. Nosocomial infections in newborn nurseries and neonatal intensive care units. Hospital epidemiology and infection control. 1995. Baltimore: Williams & Wilkins;535–564.
25. Moore DL. Olmstead RN, editor. Newborn nursery and neonatal intensive care. Infection control and applied epidemiology principles and practice: Association for Professionals in Infection Control and Epidemiology. 1996. 94. St. Louis: Mosby;1–14.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download