Abstract
Heat shock proteins (HSP) have been identified as an important factor of a very complex and highly conserved cellular defense mechanism to preserve cell survival under adverse environmental conditions. HSP 60 are immunodominant antigens of microbe such as Chlamydia trachomatis and have a potentiality to become a target antigen due to antigenic similarity between chlamydial and human HSP. This study was conducted to investigate the effects of Vero cell coculture to anti-HSP 60 on the early mouse embryo development in vitro. The 2-cell mouse embryos (ICR) were cultured and mouse embryo development was observed every 24 hr for 3 days. 45% and 22.1% of the embryos cultured in Ham's F-10 plus anti HSP 60 with Vero cells developed to the 4- to 8-cell stage (day 1) and morular stage (day 2) as compared with 29.2% and 2.7% of those cultured without Vero cells respectively. But at day 3, the beneficial effect of Vero cells was not noted. These findings suggest that Vero cells have some roles to overcome the detrimental effect of anti-HSP 60 to some degree. These results suggest that Vero cells coculture will promote reproductive outcome in patient previously sensitized to microbial (e.g. Chlamydia trachomatis) HSP 60.
Heat shock proteins (HSP) are highly conserved cellular stress proteins present in every organism from bacteria to man. It was first observed in 1962 that the salivary gland chromosomes of the fruit fly, Drosophila melanogaster, exhibited a characteristic puffing pattern after exposure to heat (1).
HSP act under physiological condition as molecular chaperones which are involved in mediating the folding and transport of other intracellular proteins and in some cases their assembly into oligomeric structures. HSP act as chaperones by participating in assembly of proteins without being part of the final protein structure (2). They are induced in response to cellular stress which includes changes in temperature, the presence of free oxygen radicals, viral and bacterial infections, heavy metals, ethanol and ischemia (3).
HSP production is enhanced during in vitro embryo culture and they are among the first proteins produced during mammalian embryo growth and presence or absence of HSP influences various aspects of reproduction in many species.
HSP are classified into different families according to their molecular weight, the 27, 60, 70 and 90 kDa HSP. HSP 60 and HSP 70 are most important in the field of reproduction. HSP 60 is located in the cell surface (4), mainly in the mitochondria (5, 6). HSP are immunodominant antigens of microbes such as Chlamydia trachomatis, which have been recognized as the main cause of tubal infertility. Many couples with fertility problems have had a previous genital tract infection, have become sensitized to microbial HSP and a prolonged and asymptomatic infection may trigger immunity to microbial HSP epitopes that are also expressed in man (7). Antibodies to both chlamydial and human HSP are found at high titre in sera and hydrosalpinx fluid and in a mouse embryo culture model (8), these antibodies impaired the mouse embryo development at unique developmental stage.
Numerous studies have demonstrated the beneficial effects of cellular monolayer of various somatic cell types on mammalian embryonic development (9-11). Many different somatic cell types have been used for coculture, including human oviductal epithelial cells (9), human endometrial fibroblasts (12), bovine oviductal epithelial cells (9). However, the use of human or animal cell lines for the coculture of embryos pose many problems such as viral infections. Vero cells, derived from African green monkey kidney, share a common embryonic origin with cells from genital tracts. However in addition, they are potentially safe to use since they are highly controlled for viruses and other contaminants. Therefore coculture using Vero cell has been widely utilized to enhance embryo viability and development (13).
The aim of this study was to investigate the detrimental effects of HSP 60 on the development of mouse embryos in vitro and to demonstrate whether Vero cells overcome these adverse effects.
5-6 week female mice were superovulated with injection of 7.5 I.U. pregnant mare's serum gonadotropin (PMSG; Sigma Chemical Co., St. Louis, MO, U.S.A.), followed 48 hr later by 7.5 I.U. human chorionic gonadotropin (PMSG; Sigma). After mating overnight, females exhibiting vaginal plug were killed 48 hr post hCG administration and 2-cell embryos were flushed from the oviducts with Dulbecco's phosphate buffered saline (D-PBS, Gibco BRL, N.Y., U.S.A.) supplemented with 0.4% bovine serum albumin (BSA, Sigma) (Fig. 1).
From the frozen cells, flasks were washed with Ham's F-10 (Gibco BRL)+10% FBS and Vero cells, 2-3×106 per well were cultured in tissue culture flask (75 cm2, Falcon) in a 5% CO2 humidified air incubator. After trypsinization, the cell suspension was divided into three parts. One third was frozen, another one third was used to seed again in a new flask, and the remaining portion was used to seed wells at a concentration of 105 cells per well reaching confluence within 3 days. The cells must not be passaged repeatedly because the growth is significantly reduced after four subpassages.
Ham's F-10 supplemented with 10% FBS was used as culture medium in the control group. The 2-cell embryos in culture medium supplemented with 100 µg/mL of monoclonal antibody specific for mammalian HSP 60 (StressGen, Canada) with or without Vero cells were incubated at 37℃ in a 5% CO2 humidified air chamber respectively and we observed mouse embryo development every 24 hr for 3 days.
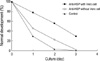
At day 1, 45% of the embryos cultured in Ham's F-10 plus anti-HSP 60 with Vero cells developed to 4- to 8-cell stage as compared with 29.2% of those without Vero cells (Table 1) (Fig. 2). Similarly at day 2, morulae were well observed in 22.1% of cultures with Vero cells as opposed to 2.7% of those without Vero cells (Table 1) (Fig. 3). In blastocystic process, however, the beneficial effects of Vero cells were not noted (Table 1) (Fig. 4).
The spontaneous expression of HSP as an essential part of embryo development is well documented and the presence or absence of HSP influences various aspects of reproduction in many species. It was reported that 2-cell mouse embryos were cultured in the presence or absence of monoclonal antibodies specific for mammalian HSP 60, HSP 70 and HSP 90 and these antibodies impaired the mouse embryo development at unique developmental stages (14). Our data in the previous study showed that anti-HSP 60 elicited a strong inhibitory effect on mouse embryo growth (15).
The detrimental effects of HSP on reproduction are based on several mechanisms. Firstly, HSP can induce a persistent inflammatory response (16). Secondly, HSP molecules serve as antigenic targets for the immune system (7). Finally, the extensive amino acid sequence homology between human and microbial HSP could result in autoimmune mediated reproductive failure (17).
The Chlamydia trachomatis infection is common and the major cause of infertility due to occluded Fallopian tubes. During the course of an acute Chlamydia trachomatis infection, immunity is restricted to HSP 60 epitopes that are specific to the invading micro-organism. Most patients with infertility problems due to tubal occlusion have experienced a chronic persistent chlamydial infection (7). The cells chronically infected with C. trachomatis synthesize only low levels of structural components but continue to produce chlamydial HSP 60 at high levels (18). Thus, some women with asymptomatic and untreated C. trachomatis infections and tubal infertility have experienced a long-term exposure to chlamydial HSP 60. Since chlamydial and human HSP share extensive amino acid sequence homology (17), it has been proposed that a prolonged exposure of the immune system to chlamydial HSP 60 and a concomitant exposure to both the chlamydial and human HSP 60 may lead to autoantibody formation (7).
Human (host) HSP 60 expression is physiologically expressed during pre- and peri-implantation stages by the embryo and the maternal deciduas. Host HSP 60 expression in early pregnancy reactivates lymphocytes previously sensitized to chlamydial HSP 60. The activated lymphocytes release proinflammatory cytokines, which induce also other lymphoid cells to release inflammatory and cytotoxic mediators. Cellular and humoral immune system activation disturbs immune regulatory mechanisms necessary to implantation and maintenance of embryos. Antibodies to HSP impair embryo development as our previous study was shown (15). Embryos are less protected from adverse environmental conditions and are more likely to degenerate or undergo apoptosis.
The mechanism of anti-HSP60 related inhibition of mouse embryo development in vitro is completely unknown. The zona pellucida of mouse oocytes and zygotes is permeable to macromolecules. Molecules up to 170 kDa have been shown to penetrate through the zona pellucida of post-ovulated mouse oocytes (19). In addition the permeability of mouse zona pellucida to IgG with induction of embryo damage has been demonstrated (20).
It is now generally accepted that Vero cells provide beneficial effects on improving embryo quality in many animal species. Cocultured embryos on the Vero cell monolayer have higher cell numbers and less fragmentation during cleavage than conventionally cultured ones (21). In addition, Vero cells have been shown to provide significant improvements in morphology and cleavage embryos (22). The resulting embryos, therefore, are more likely to implant and develop progressively.
Somatic cells such as Vero cells may provide beneficial effects on embryo development by manufacturing an in vitro environment that is compatible with normal embryo development (23). However, it is unclear why the coculture with Vero cells improves embryo development. Some claim that they remove toxic compounds from the culture medium, such as heavy metal divalent cations and metabolic inhibitors (11, 24), but others support the hypothesis that various soluble factors, including mitogenic factors secreted by Vero cells, are more important for better embryos development, although their physiologic roles are yet to be determined (10, 23).
Serum proteins decrease embryotoxicity in the conventional embryo culture system by chelating toxic components in the media (25). The fact that coculture in a simple serumfree medium exerted beneficial effects on embryos suggests that toxic substances were removed by the cells in culture (26). Hypoxanthine, which is commonly found in most good culture medium formulations, has been shown to induce the 2-cell block in mouse embryos and this agent can be removed by the somatic cells to overcome the block (27). All these observations suggest that Vero cells seem to function by removing the inhibitory substances in media rather than by producing specific factors that enhance embryonic development. We found that Vero cells are likely to overcome the detrimental effect of anti-HSP 60 to some degree (Fig. 5).
We suggest that Vero cell coculture will promote reproductive outcome in patient previously sensitized to microbial (e.g. Chalmydia trachomatis) HSP 60 which is common cause of female infertility.
Figures and Tables
 | Fig. 1Two-cell stage mouse embryos were collected at 48 hr after hCG injection from oviducts of mated ICR mice (×200). |
 | Fig. 2Photographs of the mouse embryos in vitro cultured for 24 hr in media containing anti-HSP 60 (100 µg/mL) with Vero cell coculture (A), and containing anti-HSP 60 without Vero cell coculture (B) (×200). |
 | Fig. 3Photographs of the mouse embryos in vitro cultured for 48 hr in media containing anti-HSP 60 (100 µg/mL) with Vero cell coculture (A), and containing anti-HSP 60 without Vero cell coculture (B) (×200). |
 | Fig. 4Photographs of the mouse embryos in vitro cultured for 72 hr in media containing anti-HSP 60 with Vero cell coculture (×200). |
References
1. Ritossa FA. A new puffing pattern induced by a temperature shock and DNP in Drosophila. Experientia. 1962. 18:571–573.
4. Soltys BJ, Gupta RS. Immunoelectron microscopic localization of the 60-kDa heat shock chaperonin protein (HSP 60) in mammalian cells. Exp Cell Res. 1996. 222:16–27.
5. Jindal S, Dudani AK, Singh B, Harley CB, Gupta RS. Primary structure of a human mitochondrial protein homologous to the bacterial and plant chaperonins and to the 65-kilodalton mycobacterial antigen. Mol Cell Biol. 1989. 9:2279–2283.

6. Ellis J. Stress proteins as molecular chaperones. 1996. New York: Marcel Decker;1–26.
7. Witkin SS, Neuer A, Giraldo P, Jeremias J, Tolbert V, Korneeva IL, Kneissl D, Bongiovanni AM. Chlamydia trachomatis infection, immunity, and pregnancy outcome. Infect Dis Obstet Gynecol. 1997. 5:128–132.

8. Spandorfer SD, Neuer A, LaVerda D, Byrne G, Liu HC, Rosenwaks Z, Witkin SS. Previously undetected Chlamydia trachomatis infection, immunity to heat shock proteins and tubal occlusion in women undergoing in vitro fertilization. Hum Reprod. 1999. 14:60–64.
9. Sakkas D, Trounsen AO, Kola I. In vivo cleavage rates and viability obtained for early cleavage mouse embryos in co-culture with oviductal cells. Reprod Fertil Dev. 1989. 1:127–136.
10. Menezo YJ, Guerin JF, Czyba JC. Improvement of human early embryo development in vitro by coculture on monolayers of Vero cells. Biol Reprod. 1990. 42:301–306.
11. Ouhibi N, Hamidi J, Guillaud J, Menezo Y. Co-culture of 1-cell mouse embryos on different cell supports. Hum Reprod. 1990. 5:737–743.

12. Bongso A, Gajra B, Lian NP, Wong PC, Soon-Chye N, Ratnam S. Establishment of human endometrial cell cultures. Hum Reprod. 1988. 3:705–713.

13. Menezo Y, Hazout A, Dumont M, Herbaut N, Nicollet B. Coculture of embryos on Vero cells and transfer of blastocysts in humans. Hum Reprod. 1992. 7:101–106.

14. Neuer A, Mele C, Liu HC, Rosenwaks Z, Witkin SS. Monoclonal antibodies to mammalian heat shock proteins impair mouse embryo development in vitro. Hum Reprod. 1998. 13:987–990.

15. Lee IH, Chung KN, Kim YB. Studies on the effects of monoclonal antibodies to mammalian heat shock protein 60 on mouse embryo development in vitro. Korean J Obstet Gynecol. 2003. 46:2216–2220.
16. Moseley PL. Heat shock proteins and the inflammatory response. Ann NY Acad Sci. 1998. 856:206–213.

17. Shinnick TM. Heat shock proteins as antigens of bacterial and parasitic pathogens. Curr Top Microbiol Imminol. 1991. 167:145–160.

18. Beatty WL, Byrne GI, Morrison RP. Morphologic and antigenic characterization of interferon-γ mediated persistent Chlamydia trachomatis infection in vitro. Proc Natl Acad Sci USA. 1993. 90:3998–4002.
19. Legge M. Oocyte and zygote zona pellucida permeability to macromolecules. J Exp Zool. 1995. 271:145–150.

20. Alarcon-Segovia D, Ruiz-Arguelles A, Llorente L. Broken dogma: penetration of autoantibodies into living cell. Immunol Today. 1996. 17:163–164.
21. Goodeaux LL, Thibodeaux JK, Voelkel SA, Anzalone CA, Roussel JD, Cohen JC, Menezo YJ. Collection, co-culture, and transfer of Rhesus preimplantation embryos. Assit Reprod Technol Androl. 1990. 1:370–379.
22. Van Blerkom J. Development of human embryos to the hatched blastocyst stage in the presence or absence of a monolayer of Vero cells. Hum Reprod. 1993. 8:1525–1539.

23. Gandolfi F, Brevini TA, Moor RM. Effect of oviduct environment on embryonic development. J Reprod Fertil Suppl. 1989. 38:107–115.
24. Bongso A, Fong CY, Ng SC, Ratnam S. The search for improved in vitro systems should not be ignored: embryo coculture may be one of them. Hum Reprod. 1993. 8:1155–1162.
25. Flood L, Shirley B. Reduction of embryotoxicity by protein in embryo culture media. Mol Reprod Dev. 1991. 30:226–231.

26. Fukui Y, McGowan LT, James RW, Pugh PA, Tervit HR. Factors affecting the in-vitro development to blastocysts of bovine oocytes matured and fertilized in-vitro. J Reprod Fertil. 1991. 92:125–131.
27. Loutradis D, John D, Kiessling AA. Hypoxanthine causes a 2-cell block in random bred mouse embryos. Biol Reprod. 1987. 37:311–316.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download