Abstract
The aim of this study was to evaluate the clinical efficacy of body mass index (BMI) as a predictor of in vitro fertilization and embryo transfer (IVF-ET) outcomes. Two hundred twenty-three IVF-ET cycles in 164 patients under 37 yr using GnRH agonist long protocols were included in this retrospective study. All of the selected cases were divided into two groups by a cutoff of 24 kg/m2 and these two groups were compared in regard to the outcomes of IVF-ET. There were no significant differences between group 1 (BMI <24 kg/m2) and group 2 (BMI ≥ 24 kg/m2) in age, basal serum FSH level, estradiol (E2) level and endometrial thickness on hCG day, number of retrieved oocytes and transferred embryos. However, higher doses of gonadotropins were used in group 2 (30.8±12.7 ampoules vs. 35.4±15.3 ampoules, p=0.051). The clinical pregnancy rate was significantly lower in group 2 (25.9% vs. 10.5%, p=0.041) and implantation rate tended to be lower in group 2 (12.7% vs. 6.8%, p=0.085). BMI ≥ 24 kg/m2 can be a candidate prognosticator of IVF-ET outcomes.
The effects of obesity and overweight have been studied in various diseases. It has been known that obesity may cause diabetes, osteoarthritis, cardiovascular diseases, sleep apnea, breast and uterine cancers and other reproductive disorders in women (1-4). Body mass index (BMI) has been widely used to assess the degree of obesity and overweight objectively and used as an indicator in many studies.
Detrimental impacts of obesity and overweight on pregnancy and delivery outcomes have long been investigated. Women with obesity and overweight have higher rates of abortion, preterm birth, cesarean delivery and neonatal complications (5, 6). Several hypotheses have been raised regarding an association between lower fecundity rate and obesity or overweight associated with polycystic ovary syndrome (PCOS) (7-9).
Despite the above mentioned studies, there are only few reports on the effects of obesity and overweight on the outcomes of in vitro fertilization and embryo transfer (IVF-ET) that had reported different results. While some studies reported a decrease in pregnancy and implantation rates in obese women (10-12), others reported no effects of extreme body weights (13, 14).
Average BMI and its impact on the IVF-ET can be different among different ethnic groups. Recently, a difference in the outcomes of IVF-ET between African American and white women was reported with a difference in BMI between the two (15). The effects of obesity and overweight on the IVF-ET outcomes are still unknown in Asian ethnic groups. Data on this is important since the optimal practice and prediction of prognosis in the treatment of infertile couples may be different among different races. The authors sought to elucidate the clinical efficacy of BMI as a predictor of IVF-ET outcomes in Korean women.
Two hundred and twenty-three IVF-ET cycles using GnRH agonist long protocols were retrospectively analyzed, and oocyte donation and cryopreserved embryo transfer cycles were excluded. All subjects were under 37 yr old. BMI (kg/m2) was calculated as body weight (kg) divided by height squared (m2). The outcomes of IVF-ET were compared between the two groups: BMI <24 kg/m2 (group 1) and BMI ≥24 kg/m2 (group 2).
Controlled ovarian hyperstimulation (COH) and IVF-ET was performed as reported previously (16-18). COH was undertaken using subcutaneous triptorelin (Decapeptyl®; Ferring, Sweden) in a long protocol combined with FSH (Metrodin HP®; Serono, Switzerland). Treatment with triptorelin (0.1 mg/day) began on day 21 of the preceding cycle and continued until the day of hCG treatment. As for the women with irregular menstrual cycles such as PCOS women, received GnRHa treatment with progesterone withdrawal. Treatment with 2-4 ampules of FSH, depending on the patients' previous or anticipated responses, was initiated on day 3 of the menstrual cycle. The treatment was then individualized and adjusted according to the response. When the leading follicle reached 18 mm in mean diameter with a serum estradiol (E2) level of 200 pg/mL per mature follicle, 10,000 IU of hCG (Profasi®; Serono, Switzerland) was administered. Oocyte retrieval was performed 36 hr after the hCG injection. The intracytoplasmic sperm injection (ICSI) was performed according to conventional protocols and only on the MII oocytes. Up to four embryos were transferred vaginally on the second or third day after retrieval. The luteal phase was supported by intramuscular progesterone. Cumulative embryo score (CES) was calculated as the number of blastomeres multiplied by the quality of embryo (I-V/V) and used as an indicator of implantation potential. Clinical pregnancy was diagnosed when fetal cardiac activity was confirmed by ultrasonography at 3-4 weeks after embryo transfer.
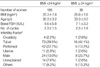
One hundred and eighty-five and 38 cycles fell into the group 1 (BMI <24 kg/m2) and group 2 (BMI ≥24 kg/m2), respectively. There was no difference in their clinical characteristics such as age, number of cycles and basal FSH levels between the two groups (Table 1).
No differences were observed in terms of peak E2 concentrations, endometrial thickness, number of retrieved oocytes and transferred embryos and cumulative embryo scores. However, higher doses of gonadotropins were used in group 2 (30.8± 12.7 ampoules vs. 35.4±15.3 ampoules, p=0.051). Clinical pregnancy rate was significantly higher in group 1 (25.9% vs. 10.5%, p=0.041). Implantation rate was also higher in group 1 (12.7% vs. 6.8%, p=0.085) (Table 2).
Various measures have been used to assess the degree of obesity and overweight including BMI, waist circumference (WC) and waist-hip ratio (WHR). WC is used to assess abdominal obesity, WHR to assess central adiposity, and BMI to assess general body composition (19, 20).
World Health Organization (WHO) defines 18.5 kg/m2 to 24 kg/m2 as 'normal', 25 kg/m2 to 30 kg/m2 as 'pre-obese' and higher than 30 kg/m2 as 'obese'. However, these criteria may not be adequate to be used in Asian women, and this necessitates provision of different standards (21-23).
The average BMI of study subjects was 21.2±2.8 kg/m2 (mean±S.D.), and as described previously, BMI of 24 kg/m2 was used as cutoff in this study. With this cutoff, only 38 cycles corresponded to high BMI group (group 2). A cutoff of 25 kg/m2 as in the WHO criteria may be inadequate as a prognostic indicator in IVF-ET cycles of Korean women since the distribution of BMI differs according to ethnicity and environment.
Underweight has also been known to negatively affect the outcomes of IVF-ET (24). Nichols et al. reported the harmful impact of both extremes of BMI on the IVF-ET outcomes (11, 25). From the data of our study subjects, BMI <18 kg/m2 showed a trend of lower pregnancy rates compared to BMI≥18 kg/m2 group (data not shown). When subjects of BMI <18 kg/m2 were eliminated from the group of BMI <24 kg/m2, the difference in pregnancy rate became more significant (p=0.027).
The mechanism of the effects of BMI is uncertain. From oocyte donation model, Wattanakumtornkul et al. reported no difference in the endometrial thickness among women with different BMI (26). Wang et al. reported that the quality of transferred embryos was worse in higher BMI women (27). With these reports and ours that also showed no difference in the endometrial thickness (Table 2), it may possibly assumed that BMI affect ovarian folliculogenesis rather than uterine receptivity.
A higher dose of gonadotropin was necessary in high BMI group in this study (Table 2). This finding is supported by a report of Fedorcsak et al. (28). In regard to the underlying mechanisms, hyperandrogenism and hyperinsulinemia as in the case of chronic anovulation has been suspected (29). Or whether this was just due to the gonadotropin concentrations per unit kg is also subject to further studies.
Intrafollicular hCG concentrations has been studied in relation to BMI by Carrell et al. (30). BMI was inversely related to intrafollicular levels of hCG. If this is a significant mechanism, an increase in the dose of hCG in higher BMI women should be considered, which needs to be confirmed by further studies.
An ethnic difference in the outcomes of IVF-ET was reported between white and African American women (15). In this report, a difference in the BMI was found between the two groups. Therefore, it should be differentiated whether the effects of BMI is confounded by a racial difference. As Korean women are of one nation, comparative studies between Korean and other Asian women would provide data for the explanation of the aforementioned findings.
We sought to evaluate the clinical efficacy of BMI as a predictor of IVF-ET cycles using GnRH agonist long protocols. With a cutoff of 24 kg/m2, higher BMI women showed a decrease in clinical pregnancy and implantation rates and an increase in the gonadotropin requirement. In Korean women, a lower cutoff seems to be efficacious in predicting the outcomes of IVF-ET cycles, rather than the WHO criteria of preobese and obese being ≥25 kg/m2. Further studies in a larger scale are necessary to confirm these data and to search the underlying mechanisms, and to evaluate the effects of BMI in women using other COH protocols. Whether the weight control of women with BMI of ≥24 kg/m2 prior to IVF-ET cycles has any therapeutic efficacy is also subject to further investigations.
Figures and Tables
References
1. Legato MJ. Gender-specific aspects of obesity. Int J Fertil Womens Med. 1997. 42:184–197.
2. Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, Hennekens CH, Speizer FE. Body weight and mortality among women. N Engl J Med. 1995. 333:677–685.

3. Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW Jr. Body-mass index and mortality in prospective cohort of U.S. adults. N Engl J Med. 1999. 341:1097–1105.
4. Taucher S, Gnant M, Hausmaninger H. The prognostic influence of body mass index in premenopausal breast cancer patients. Breast. 2003. 12:S18.

5. Isaacs JD, Magann EF, Martin RW, Chauhan SP, Morrison SC. Obstetric challenges of massive obesity complicating pregnancy. J Perinatol. 1994. 14:10–14.

6. Green BB, Weiss NS, Daling JR. Risk of ovulatory infertility in relation to body weight. Fertil Steril. 1988. 50:721–726.

7. Pasquali R, Casimirri F, Vicennati V. Weight control and its beneficial effect on fertility in women with obesity and polycystic ovary syndrome. Hum Reprod. 1997. 12:82–87.

8. Goswamy N, Feldman J, Grazi RV. Body mass index in patients with polycystic ovary syndrome: a comparison of treatment outcomes with clomiphene and gonadotropins. Fertil Steril. 2002. 78:S222.

9. Nam YS, Jeong CJ, Kim NK, Yoon TK, Cha KY. Clinical consideration of obese infertile women. Korean J Fertil Steril. 2002. 29:209–214.
10. Loveland JB, McClamrock HD, Malinow AM, Sharara FI. Increased body mass index has a deleterious effect on in vitro fertilization outcome. J Assist Reprod Genet. 2001. 18:382–386.
11. Nichols JE, Crane MM, Higdon HL, Miller PB, Boone WR. Extremes of body mass index reduce in vitro fertilization pregnancy rates. Fertil Steril. 2003. 79:645–647.

12. Merryman DC, Yancey CA, Dalton KE, Houserman VL, Long CA, Honea KL. Regardless of oocyte source, body mass index is predictive of in vitro fertilization success. Fertil Steril. 2003. 80:S169.

13. Lashen H, Ledger W, Bernal AL, Barlow D. Extremes of body mass do not adversely affect the outcome of superovulation and in-vitro fertilization. Hum Reprod. 1999. 14:712–715.

14. Lewis CG, Warnes GM, Wang X, Matthews CD. Failure of body mass index or body weight to influence markedly the response to ovarian hyperstimulation in normal cycling women. Fertil Steril. 1990. 53:1097–1099.

15. Nichols JE Jr, Higdon HL 3rd, Crane MM 4th, Boone WR. Comparison of implantation and pregnancy rates in African American and white women in an assisted reproductive technology practice. Fertil Steril. 2001. 76:80–84.

16. Kim SH, Ku SY, Jee BC, Suh CS, Moon SY, Lee JY. Clinical significance of transvaginal color Doppler ultrasonography of the ovarian artery as a predictor of ovarian response in controlled ovarian hyperstimulation for in vitro fertilization and embryo transfer. J Assist Reprod Genet. 2002. 19:103–112.
17. Ku SY, Suh CS, Kim SH, Choi YM, Kim JG, Moon SY. A pilot study of the use of low dose human menopausal gonadotropin in ovulation induction. Eur J Obstet Gynecol Reprod Biol. 2003. 109:55–59.

18. Jee BC, Ku SY, Suh CS, Choi YM, Kim JG, Moon SY, Kim SH. Cumulative ongoing pregnancy rate in intracytoplasmic sperm injection cycles. J Obstet Gynaecol Res. 2004. 30:372–376.

20. Hollmann M, Runnebaum B, Gerhard I. Impact of waist-hip-ratio and body-mass-index on hormonal and metabolic parameters in young, obese women. Int J Obes Relat Metab Disord. 1997. 21:476–483.

21. Park YW, Kim CH, Shin HC. Is the cut-off value of body mass lndex (BMI) appropriate for identifying obesity in Korea? Korean J Health Promotion Dis Prev. 2002. 2:10–16.
22. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004. 363:157–163.
23. Patel JK, Hughes EA, Mackness MI, Vyas A, Cruickshank JK. Appropriate body-mass index for Asians. Lancet. 2003. 361:85.

24. Rich-Edwards JW, Spiegelman D, Garland M, Hertzmark E, Hunter DJ, Colditz GA, Willett WC, Wand H, Manson JE. Physical activity, body mass index, and ovulatory disorder infertility. Epidemiology. 2002. 13:184–190.

25. Nichols JE, Miller PB, Boone WR, Crane MM. Effects of extremes of body mass index (BMI) on in vitro fertilization (IVF) pregnancy rates. Fertil Steril. 2001. 76:S74.

26. Wattanakumtornkul S, Damario MA, Stevens Hall SA, Thornhill AR, Tummon IS. Body mass index and uterine receptivity in the oocyte donation model. Fertil Steril. 2003. 80:336–340.

27. Wang JX, Davies M, Norman RJ. Body mass index and probability of pregnancy during assisted reproduction treatment: retrospective study. BMJ. 2000. 321:1320–1321.
28. Fedorcsak P, Dale PO, Storeng R, Ertzeid G, Bjercke S, Oldereid N, Omland AK, Abyholm T, Tanbo T. Impact of overweight and underweight on assisted reproduction treatment. Hum Reprod. 2004. 19:2523–2528.
29. Pasquali R, Pelusi C, Genghini S, Cacciari M, Gambineri A. Obesity and reproductive disorder in women. Hum Reprod Update. 2003. 9:359–372.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download