Abstract
This study is a retrospective examination of our experiences with patients who underwent treatment of isolated synchronous brain metastases coupled with primary non-small cell lung cancer. From January 1995 to June 2004, 12 patients presented with isolated synchronous brain metastases coupled with primary non-small cell lung cancer. The patient was comprised of 8 men and 4 women. The median age was 52 yr, in a range of 32 to 75 yr. Median follow-up duration was 10.6 months, in a range of 2 to 55.8 months. Recurrence developed in 7 patients, and the median interval from 1st treatment to recurrence was 4.5 months (2.8-6.5 months). The overall 1-yr survival rate was 61.7%. The 1-yr survival rates for pathologic N0 and N1 cases were 75% and 66.7%, respectively. The median survival duration for pathologic N2 was 6.2 months (95% CI, 4.8-7.5 months). The 1-yr survival rate for cases of single brain metastasis was 75%. Based on our current observations, we could speculate that aggressive management of primary non-small cell lung cancer and isolated synchronous brain metastases was beneficial in a selected group of patients, as long as the brain lesions and pulmonary lesions were limited or resectable.
With regard to oncology, the brain is very closely related to the lung. Lung cancer is the most common cause of metastasis to the central nervous system (1). The brain is also one of the most commonly involved organs in metastases from non-small cell lung cancer (NSCLC) (2).
Unfortunately, once metastatic brain disease become clinically apparent, the cancer usually has already disseminated widely, which signifies extremely poor prognosis. The median survival duration of patients with brain metastases from NSCLC is approximately 1 month without treatment (3), 2-3 months when treated with steroids alone (4), and 3-6 months when treated with whole brain radiotherapy (WBRT) (5). As the survival of patients with brain metastases tends to be so short, quality of life and alleviation of symptoms are considered to be the principal therapeutic objectives.
Recently, however, aggressive treatment involving either surgical resection or radiosurgery has been applied, with potential curative intentions. Neurosurgical resection of solitary brain metastasis of various origins resulted in a prolongation of median survival to 3.5-8 months (6). Also, in lung cancer cases, several retrospective reviews have suggested that aggressive therapy, such as resection of the lung and isolated synchronous brain lesions, as well as metachronous brain metastases, may be associated with prolonged survival duration (7-9). Under the presumption that low-burden metastatic disease can be effectively surgically resolved in certain subsets of patients, we have treated patients exhibiting primary NSCLC and isolated synchronous brain metastases aggressively, by the combined control of lung and brain lesions.
This study retrospectively examined our experiences with patients who underwent treatment of isolated synchronous brain metastases coupled with primary NSCLC in the last ten years.
From January 1995 to June 2004, 1,590 patients underwent surgical resection for NSCLC at our institution. Twelve (0.7%) of these patients exhibited isolated synchronous brain metastases coupled with primary NSCLC.
Preoperative workups included computed tomography (CT) scanning of the chest and upper abdomen in all patients, bronchoscopy or percutaneous needle aspiration, when applicable, for the histologic evaluation of all patients, brain magnetic resonance imaging (MRI) in all patients with neurologic symptoms or adenocarcinoma, bone scans, and positron-emission tomography (PET) or PET-CT. Pathologic reviews of pulmonary and cerebral or cerebellar neoplastic tissue confirmed identical histological diagnoses for all patients who underwent craniotomies.
Synchronous brain metastases were defined as those metastases which were diagnosed less than 60 days from the time at which the primary NSCLC was diagnosed.
The medical records of each patient were examined with regard to age, sex, histologic type and grade, pathologic intrathoracic TN stage, surgical procedure, postoperative complications, adjuvant therapy, and survival duration. Follow-up included outpatient visits and correspondence. Every patient was completely traced. Cerebral resections were considered complete when all gross evidence of disease was removed. In all patients, pathologic staging was conducted according to the guidelines of the International Staging System for NSCLC (10). Operative mortality included patients who died within the first 30 days after the thoracic procedure, as well those who died later, but during the same period of hospitalization.
Our patient was comprised of 8 men and 4 women. Median patient age was 52 yr, in a range of 32 to 75 yr. Median time between the first cerebral treatment or pulmonary resection and the pulmonary resection or cerebral treatment was 15 days, in a range of 10 to 380 days.
No patients received neoadjuvant chemotherapy or radiotherapy. Pulmonary resection included pneumonectomy in 1 patient, bilobectomy in 4, lobectomy in 6, and wedge resection in 1. Mediastinoscopic lymph node biopsies were conducted in 3 patients, all of which generated negative findings. Complete pulmonary resections (R0) and mediastinal lymph node dissections were performed in all patients, with the exception of one, who underwent wedge resection. Adjuvant radiotherapy was administered in 2 patients with pathologic T2N2 stage. No patients received adjuvant chemotherapy.
The NSCLC histologic type was adenocarcinoma in 7 patients (58.3%), squamous cell carcinoma in 3 (25%), and adenosquamous cell carcinoma in 2. Lymph node metastases were present in 7 patients, and were staged N1 in 3 patients and N2 in 4. The locoregional NSCLC staging is shown in Table 1.
Six out of 12 patients exhibited neurological symptoms. These included headaches in 4, visual disturbances in 1, slurred speech in 1, motor weakness in 1, and gait disturbances in 1. The number and location of metastatic lesions is shown in Table 2.
Treatment for brain lesions included 5 craniotomies, 7 stereotactic radiosurgery (SRS), and 11 WBRT. WBRT was recommended to all patients, but one patient refused it. As modality to increase local control, either craniotomy or SRS was applied, and the decision on modality selection was made on an individual bases considering the advantages and the disadvantages of each modality. Craniotomy was favored if the lesions were rather superficially located and were causing distressing neurologic symptoms and signs, while SRS was favored if the lesions were in deep and eloquent areas. Further local treatment for the brain lesions was not performed in two patients following WBRT, who were with very small sized metastatic lesions. Treatment for brain lesions was carried out prior to that for pulmonary lesions in 7 patients, one of whom underwent craniotomy and WBRT at another hospital. Gross total removal of metastatic tumors was verified in all patients who underwent craniotomy at our institution. The radiation dose for WBRT was 30 Gy in 10 fractions in every patient. The combination of treatment modalities for brain lesions is shown in Table 3. SRS was conducted with linear accelerator-based radiosurgery system in 1 patient, and Gamma-Knife unit in 6 patients.
Survival was estimated by the Kaplan-Meier method, with the date on which treatment on cerebral or pulmonary lesion was initiated as the starting point, and the date of death or last follow-up as the end point. Comparisons of survival by univariate analysis were estimated by the log-rank test. Cox's proportional hazard model was used for multivariate analyses. A p value of less than 0.05 (p<0.05) was considered to be statistically significant. All analyses were performed using the SPSS software package (SPSS for Windows, Release 11.0, Standard Version).
There was no operative or in-hospital mortality. Follow-up was completed for all 12 patients for a median of 10.6 months and a range of 2 to 55.8 months.
Recurrence developed in 7 patients. Recurrence occurred in the brain in 2, distant organ in 2 (pelvic bone/ovary, adrenal gland/rib), and both the brain and distant organ in 3 (brain/extremity, brain/liver/pleura, brain/spine). The pathologic TN stages of patients developing recurrences were T2N0 in 3, T1N2 in 1, T2N2 in 2, and T3N1 in 1.
The median interval from initiation of treatment to recurrence was 4.5 months (2.8-6.5 months).
Treatment of recurrence included 2 WBRT and 4 SRS for cerebral lesions, radiotherapy for spine, extremities, ribs, and pelvic bones, adrenalectomy, and salphingooophrectomy.
Currently, 8 patients remain alive, and 4 of them have exhibited no signs of recurrence at 8.5, 12.9, 34.5, and 55.8 months after the initial treatment.
The overall 1-yr survival rate was 61.7% (Fig. 1).
The 1-yr survival rates for pathologic N0 and N1 were 75% and 66.7%, respectively. The median survival duration for pathologic N2 was 6.2 months (95% CI, 4.8-7.5 months) (Fig. 2). The difference between survival rates according to pathologic N stage evidenced a trend toward statistical significance (N0 vs. N2, p=0.0586).
The 1-yr survival rates for locoregional pathologic stages I and III were 75% and 53.3%, respectively (p=0.2492).
The 1-yr survival rates for solitary and multiple brain metastases were 75% and 44.4%, respectively (p=0.1442). The 1-yr survival rate for the 9 patients with brain metastases involving less than 4 lesions was 70%. Seven of these patients remain alive for between 5.6 and 55.8 months.
The 1-yr survival rate for the 4 patients with 2 or 3 cranial metastases was 66.7%, which was not significantly different from that for patients with solitary brain metastases (p=0.5). Currently, 3 patients of them remain alive, at 5.6, 8.5, and 12.8 months after the initial treatment.
Survival was not found to vary significantly with histologic type (adenocarcinoma vs. non-adenocarcinoma, p=0.9859).
Approximately 25% of patients with stage IV NSCLC exhibit brain metastases, as well as other incidences of metastatic disease (11). The natural course of untreated brain metastases included progressive neurological deterioration, with a median survival time of 1-2 months (6). The prognoses of brain metastasis patients tend to be poor, with a median survival of 2 months when treated with steroids alone, and 3 to 6 months when treated with WBRT.
Aggressive treatment of brain metastases may involve either the surgical resection of the metastases, or the ablation of the metastases by SRS. Removal of brain metastases has been determined to prolong survival and improve quality of life (12). The effect of treatment of brain metastases without treatment of the primary site, however, may be quite limited.
Retrospective series suggest that some patients with stage IV lung cancer, coupled with a solitary synchronous site of extrathoracic metastatic disease, can be effectively treated by the resection of both the primary tumor and the metastasis (7-9, 13).
Among patients with lung cancer that has metastasized to the brain, the most favorable prognoses are associated with complete resection of the primary lung tumor (14). Solitary metastases are associated with better prognoses than are multiple metastases (9). Whether brain metastases are metachronous or synchronous has not generally been found to influence survival. It remains unclear as to whether or not the lymph node status of the primary tumor is of prognostic significance in patients who undergo resection of a solitary brain metastasis (7).
Bonnette et al. suggested that it seemed legitimate to proceed with lung resection after the complete resection of a single brain metastasis, at least in patients with an adenocarcinoma and a small lung tumor and without abnormal mediastinal lymph nodes, as seen on the CT scans or during mediastinoscopic lymph node biopsies (15).
The overall 1-yr survival rate of our patients was 61.7%, which is consistent with the findings of other reviews. Our cases included two cases of brain metastases with more than 4 lesions. One was a patient who was discovered to have leptomeningeal seeding 48 days after pulmonary resections. The other was a patient whose multiple brain lesions had regarded as ischemic change, and thus the treatment of this patient's brain lesion was delayed. Excluding these cases from the survival analysis, the overall 1-yr survival rate was 70%.
Although no evident statistical differences were detected, the difference between survival rates according to pathologic N status tended toward statistical significance (p=0.0586). In addition, the survival of patients with pathologic N1 was not different from that of those with pathologic N0 (p=0.5316).
When deciding upon the most appropriate treatment option for an individual patient, the following factors should be taken into consideration: symptoms; general condition of the patient; extent and status of cerebral disease; and extent and status of extracranial disease. Craniotomy is the preferred treatment modality for solitary lesions associated with significant edema, large lesions (greater than 3 cm at maximal diameter), superficial lesions, lesions causing symptoms requiring immediate relief, and lesions associated with hemorrhage. SRS is recommended in cases in which the lesion is deep, but is less than 3 cm at maximal diameter, when there are medical contraindications to craniotomy, or in some cases, when the tumor recurs (16). There are benefits associated with both craniotomy and SRS. The decision to operate on lesions of intermediate size (which typically range from 1 to 3 cm in maximal diameter) is particularly challenging, as in many cases, surgery and SRS may be considered to be equally appropriate treatment methods (17). The advantages of craniotomy include the immediate resolution of mass effects, the acquisition of tissue for pathologic diagnosis, and no risk of radiation necrosis (18). The advantages of SRS include decreased risks of hemorrhage and infection, less invasiveness, and no risk of tumor seeding. The disadvantages of SRS include the potential exacerbation of peritumoral edema, the necessity for long-term steroid administration, and radiation necrosis (19). Tumors in eloquent cortex, or deep-seated tumors, are usually considered unresectable. In these cases, SRS constitutes a compelling alternative to surgery. With regard to resectable metastases, it remains unclear as to whether SRS or craniotomy provides better survival benefits, even for patients manifesting single brain metastases (18).
In our reviewed cases, we included patients with multiple cerebral metastatic lesions as well as patients with single lesions (Table 2). The survival rate associated with 2 or 3 cranial metastases was not significantly different from that associated with solitary brain metastases. A patient with T2N0 stage and 2 cranial metastases was successfully treated via a combination of SRS for the smaller lesion, craniotomy for the larger lesion, WBRT, and bilobectomy. This patient remains alive, 12.8 months after the inception of treatment (Fig. 3).
Based on our current observations, we could speculate that aggressive management of primary NSCLC and isolated synchronous brain metastases was beneficial in a selected group of patients, as long as the brain lesions and pulmonary lesions were limited or resectable. Admitting the positive role of surgery in the management of isolated synchronous brain metastases coupled with primary NSCLC, we are planning to design a prospective phase II study regarding the surgical treatment of NSCLC with isolated synchronous brain metastases.
Figures and Tables
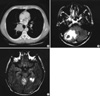
Fig. 3
Preoperative chest CT and brain MRI of 54-yr-old man with locoregional pathologic stage T2N0 coupled with two metastatic brain lesions. A 5-cm sized central mass at the orifice of the right lower lobar bronchus protrudes into the right bronchus intermedius (A). Axial views of T2-weighted fluid-attenuated inversion recovery (FLAIR) imaging show a solid mass in the right cerebellar hemisphere (B), and in the medial portion of the left temporal lobe (C).
References
1. Poggi MM, Sullivan FJ. Pass HI, Carbone DP, Johnson DH, Minna JD, Turrisi AT, editors. Palliative radiotherapy. Lung cancer principles and practice. 2005. 3rd ed. Philadelphia: Lippincott Williams & Wilkins;777–793.
2. Lee JL, Shin CJ, Kang HJ, Oh HA, Lee G, Choi JH, Bae SH, Lee KH, Hyun MS, Shin SO, Ryoo HM. Brain metastasis: Clinical characteristics and prognosis. Korean J Med. 2002. 62:444–452.
3. Kelly K, Bunn PA Jr. Is it time to reevaluate our approach to the treatment of brain metastases in patients with non-small cell lung cancer? Lung Cancer. 1998. 20:85–91.

4. Horton J, Baxter DH, Olson KB. The management of metastases to the brain by irradiation and corticosteroids. Am J Roentgenol Radium Ther Nucl Med. 1971. 111:334–336.

5. Posner JB. Management of central nervous system metastases. Semin Oncol. 1977. 4:81–91.
6. Penel N, Brichet A, Prevost B, Duhamel A, Assaker R, Dubois F, Lafitte JJ. Prognostic factors of synchronous brain metastases from lung cancer. Lung Cancer. 2001. 33:143–154.
7. Magilligan DJ Jr, Duvernoy C, Malik G, Lewis JW Jr, Knighton R, Ausman JI. Surgical approach to lung cancer with solitary cerebral metastasis: twenty-five years' experience. Ann Thorac Surg. 1986. 42:360–364.

8. Read RC, Boop WC, Yoder G, Schaefer R. Management of non-small cell lung carcinoma with solitary brain metastasis. J Thorac Cardiovasc Surg. 1989. 98:884–890.

9. Burt M, Wronski M, Arbit E, Galicich JH. Resection of brain metastases from non-small-cell lung carcinoma. Results of therapy. Memorial Sloan-Kettering Cancer Center Thoracic Surgical Staff. J Thorac Cardiovasc Surg. 1992. 103:399–410.
10. Mountain CF. Revisions in the International System for Staging Lung Cancer. Chest. 1997. 111:1710–1717.

11. Detterbeck FC, Jones DR, Molina PL. Detterbeck FC, Rivera MP, Socinski MA, Rosenman JG, editors. Extrathoracic staging. Diagnosis and treatment of lung cancer / an evidence-based guide for the practicing clinician. 2001. Philadelphia: W.B. Saunders Co.;94–110.
12. Hankins JR, Miller JE, Salcman M, Ferraro F, Green DC, Attar S, McLaughlin JS. Surgical management of lung cancer with solitary cerebral metastasis. Ann Thorac Surg. 1988. 46:24–28.

13. Macheers SK, Mansour KA. Management of isolated splenic metastases from carcinoma of the lung: a case report and review of the literature. Am Surg. 1992. 58:683–685.
14. Macchiarini P, Buonaguidi R, Hardin M, Mussi A, Angeletti CA. Results and prognostic factors of surgery in the management of non-small cell lung cancer with solitary brain metastasis. Cancer. 1991. 68:300–304.

15. Bonnette P, Puyo P, Gabriel C, Giudicelli R, Regnard JF, Riquet M, Brichon PY. Groupe Thorax. Surgical management of non-small cell lung cancer with synchronous brain metastases. Chest. 2001. 119:1469–1475.

16. Olak J, Ferguson MK. Pass HI, Mitchell JB, Johnson DH, Turrisi AT, Minna JD, editors. Surgical management of second primary and metastatic lung cancer. Lung cancer: principles and practice. 2000. 2nd edition. Philadelphia, PA: Lippincott Williams & Wilkins;730–741.
17. Lang FF, Chang EL, Abi-said D, Wildrick DM, Sawaya R. Richard WH, Youmans JR, editors. Metastatic brain tumors. Neurological surgery. Vol. 1. 2004:5th edition. Philadelphia: Lea & Febiger;1077–1097.

18. Loeffler JS, Alexander ER. Alexander E, Loeffler JS, Lunsford LD, editors. Radiosurgery for the treatment of intracranial metastases. Stereotactic radiosurgery. 1993. New York: McGraw-Hill;197–206.
19. Kondziolka D, Lunsford LD. Apuzzo MLJ, editor. Brain metastases. Brain surgery: complication avoidance and management. 1993. Vol. 1. New York: Churchill Livingstone;615–641.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download