Abstract
This is to examine whether aggressive multimodality therapy improves the treatment outcomes in stage IIIA non-small cell lung cancer (NSCLC). Fifty-three consecutive NSCLC patients with N2 disease, confirmed by mediastinoscopic biopsy, received preoperative thoracic radiation therapy (45 Gy/5 weeks) concurrent with two cycles of oral etoposide and intravenous cisplatin and surgery. Postoperative radiation therapy (PORT, 18 Gy/2 weeks) was optionally recommended for those with the risk factors of loco-regional recurrence based on the surgical and pathological findings. Surgical resection was performed in 38 patients (71.7%), and down-staging was achieved in 19 patients (50%). The median survival period was 27 months in 38 patients who underwent resection, and the rates at 3-yr of overall survival, loco-regional control, distant metastasis-free survival, and disease-free survival were 44.3%, 87.9%, 32.9%, and 29.3%. Significantly favorable factor regarding overall survival was achieving p0/I stage by the multivariate analysis. PORT was successful in reducing locoregional recurrences in patients with the risk factors. Current preoperative concurrent radiochemotherapy and surgery by the authors resulted in comparable survival with other reports, however, further refinement of multimodality approach may be warranted for more effective reduction of distant metastasis.
Of newly diagnosed non-small cell lung cancer (NSCLC), stage III cancer is approximately 30-40%. The prognosis of patients with preoperative N2 disease treated with surgery or radiation therapy alone is poor (1). In efforts to improve local control and survival of patients with marginally resectable disease, various clinical trials particularly to determine the optimal ways to combine thoracic radiation therapy (TRT), chemotherapy, and surgery have been performed. Currently, the most common method is the induction chemotherapy with or without TRT and surgery, however, the results of several randomized trials of preoperative chemotherapy and surgery were conflicting (2-4). Non-randomized trials of preoperative concurrent radiochemotherapy (CRCT) produced encouraging results (5-11), and these trials have a few drawbacks as they may have included the patients with stage IIIB based on inconsistent clinical nodal staging, accrued small number of patients, and employed the various radiation and chemotherapy dose schedules.
We applied mediastinoscopic biopsy for potentially operable NSCLC patients and recommended preoperative CRCT and surgery for those with N2 disease. Here, we would report the treatment outcomes and discussed the role of preoperative CRCT and surgery.
We have adopted N-staging by mediastinoscopic biopsy for potentially operable NSCLC patients. Fifty-three patients with stage IIIA NSCLC with N2 disease confirmed by mediastinoscopic biopsy were treated with preoperative CRCT and surgery from August 1997 till April 2001. The eligibility for this treatment is that each patient should have 1) ECOG performance score of 2 or lower, 2) no major medical illness that might conflict with the aggressive treatment, 3) no significant weight loss (less than 10% during recent 6 months), 4) no history of malignancy other than the current illness, and 5) adequate pulmonary, renal, hepatic, and hematologic reserves. The pretreatment work-ups for the diagnosis and staging included simple chest radiography, chest computerized tomography (CT) scans, bronchoscopic evaluation with biopsy and/or washing cytology, complete blood counts, routine urinalyses, chemistry profiles and whole-body bone scan. Abdominal ultrasonography and brain CT or magnetic resonance imaging were performed when clinically indicated.
The tri-modality treatment consists of preoperative CRCT and surgery, and postoperative radiation therapy (PORT) was optionally recommended for those with risk factors of locoregional recurrence based on the surgical and pathological findings (Fig. 1). Preoperative CRCT consists of TRT (45 Gy/5 weeks) and two cycles of oral etoposide (100 mg/m2/day, days 1-14 and days 29-42) and intravenous cisplatin (100 mg/m2, day 1 and day 29) that were concurrently delivered during the TRT course. 10 MV radiography from a linear accelerator were used in all patients' TRT, and the TRT volume was individually determined to include the primary tumor, the ipsilateral hilum and the mediastinum based on the chest CT scans, but not the bilateral supraclavicular lymph node areas. The radiation dose to the spinal cord was kept at or below 45 Gy. Surgery was planned 4 to 6 weeks after CRCT completion. PORT (18 Gy/2 weeks) was optionally recommended for patients with risk factors of recurrence such as incomplete resection, positive/close bronchial resection margin (no more than 5 mm), and high risk N1 or persistent N2 disease based on the surgical and pathological findings. We defined high risk N1 disease as having any of the followings: multiplicity; proximal location; and extracapsular extension. The PORT volume mainly included the mediastinum, which optionally was extended to cover the bronchial stump.
Clinical response was evaluated by chest CT scans taken in 3 weeks of the completion of CRCT and just before surgery. The pathologic response and the down-staging rates were evaluated by thorough pathological examination. The regular follow-up examinations included chest CT scans and other necessary laboratory tests.
We analyzed the followings: 1) the overall compliance and the resection rate, 2) the incidence and severity of the acute side effects according to ECOG/RTOG toxicity criteria, 3) the results of pathologic evaluation and the down-staging rate, 4) the patterns of failure and survival results calculated by the Kaplan-Meier method, and 5) the significance of the possible prognostic factors by log-rank test. Survival was calculated from the day 1 of CRCT.
The median age was 60 (37-75) yr, and the ratio of male and female was 38:15. More patients were with adenocarcinoma than squamous cell carcinoma (33 vs. 19), where adenocarcinoma was far more common than squamous cell carcinoma among the female patients (14:1), while its incidence was about the same as squamous cell carcinoma among the male patients (19:18). The ECOG performance status was good to excellent in most patients: 0-1 in 51 patients (96.2%); and 2 in only 2 (3.8%). The degree of weight loss was 5% or lower in the majority of patients (84.9%; 45/53), while it was over 5% but not higher than 10% in 8 patients (15.1%). Clinical T-stages based on chest CT scans and bronchoscopic findings were cT1 in 7 patients, cT2 in 38, and cT3 in 8. The chest CT criteria for the clinically metastatic mediastinal lymph node(s) included that 1) the shortest dimension of the affected lymph node should be equal to or greater than 1 cm (1.5 cm in case of subcarinal lymph node) and/or that 2) there should be the findings compatible with extracapsular extension or necrosis. Thirty patients (56.6%) were with clinical N2 disease based on the chest CT findings. The characteristics of patients are summarized in Table 1.
TRT was completed in 49 patients (92.5%), and four patients who developed either distant metastasis or severe side effects during CRCT course could not complete TRT. Forty-one patients (77.4%) could complete two cycles of chemotherapy as planned, while twelve (22.6%) received only the first cycle. Thoracotomy was attempted in 39 patients, and resection was performed in 38 patients, as one patient was with unpredicted pleural seeding at the time of thoracotomy. The resulting surgical resection rate was 71.7% (38/53). The reasons for 'no resection' in 15 patients were as follows: six patients refused surgery; five developed loco-regional or distant disease progression; and four had severe acute morbidity disabling surgery. The surgery types were lobectomy in 27 patients (51.1%), bilobectomy in three (7.9%), and pneumonectomy in eight (21.1%). In three patients complete mediastinal lymph node dissection could not be performed: mediastinal fibrosis in two patients; and invasion of the superior vena cava and the pericardium by the lymph node in one patient. After surgery, 24 patients had risk factors of recurrence, among whom 17 patients received PORT, while seven refused PORT.
During CRCT, the most common grade III or IV acute morbidity was neutropenia (58.5%; 31/53). Most non-hematologic acute morbidities were grade 0-II: esophagitis in 51 patients (96.2%); nausea/vomiting in 52 patients (98.1%); and acute lung toxicity in 51 patients (96.2%). Grade III esophagitis, nausea/vomiting, and lung toxicity occurred in 2, 1, and 2 patients, respectively. Two treatment-related deaths (3.8%) occurred: one died of sepsis after CRCT; and the other died of respiratory failure after pneumonectomy and chest wall resection. The details of acute morbidities are shown in Table 2.
Pathologic responses to preoperative CRCT were evaluated in 38 resected patients. Post-surgical T-stages were pT0 in three patients, pT1 in 18, pT2 in 13, pT3 in two, and pT4 (satellite nodules) in two. Post-surgical N-stages were pN0 in 17 patients, pN1 in two, and pN2 in 19. Post-surgical overall stages were p0 in one patient, pIA in nine, pIB in five, pIIA in one, pIIB in three, pIIIA in 17, and pIIIB in two, and down-staging was achieved in half of the patients (19/38). Table 3 shows the changes of the stage after the completion of preoperative CRCT. After resection, 24 patients had risk factors of recurrence: pN2 was the most common in 19 patients; close or positive resection margins in seven patients; incomplete resection in three patients; high-risk pN1 in one patient; and chest wall invasion in one patient.
The pattern of the first failure site was analyzed in 38 resected patients. Local recurrence (LR), regional recurrence (RR), and distant metastasis (DM) were defined according to the AJCC staging criteria. LR was observed in five patients (13.2%), RR was in three (7.9%), and DM was in 24 (63.2%). The patterns of LR were pleural seeding (PS) in three patients and bronchial stump recurrence in two. All three patients with RR also had simultaneous LR: two with mediastinal lymph node recurrence had bronchial stump recurrence and PS, respectively; and one with mediastinal and supraclavicular lymph node recurrence had PS. Twenty-one patients developed DM only, two did combined DM+LR, and one did combined DM+LR+RR.
The patterns of failure were somewhat different according to the subgroups of patients based on the post-surgical risk factors and the addition of PORT. Among 14 patients who had no risk factors and did not receive PORT, only one developed combined PS+RR, and eight did DM, one of which was within the TRT volume. Among 17 patients who had risk factors and received PORT, only one developed combined PS+DM, and 11 did DM only, all of which were also outside the TRT volume. On the contrary, among seven patients who had risk factors but did not receive PORT, one developed combined LR (bronchial stump recurrence) +RR (mediastinal lymph node), one did combined LR (bronchial stump recurrence) +RR (mediastinal and supraclavicular lymph node) + DM, and one did combined PS+DM, two of which were within the TRT volume (Fig. 2).
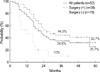
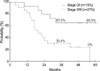
The median follow-up period for the survivors was 48 months (range: 20-74 months). For all 53 patients, the median survival duration was 22 months, and the 3- and 5-yr overall survival (OS) rates were 34.9% and 25.7%. In 38 patients who underwent surgical resection, the median survival duration was 27 months, and the 3- and 5-yr OS rates were 44.3% and 32.7%. In 15 patients who did not undergo surgical resection, the median survival duration was 12 months, and the 3-yr OS rate was 10%. In the patients who underwent surgical resection, the median disease-free interval was 16 months, the 3- and 5-yr disease-free survival (DFS) rates were 29.3% and 25.6%, the 3- and 5-yr loco-regional control (LRC) rates and distant metastasis-free survival (DMFS) rates were 87.9% and 81.6%, and 32.9% and 28.8%, respectively (Fig. 3, 4).
The prognostic implication of the possible prognostic factors including age, sex, histology, PORT, preoperative T-stage, postoperative T-stage, postoperative N-state, and postoperative overall stage were analyzed in 38 patients who underwent surgical resection. By the univariate analysis, surgical resection, achieving pN0, and achieving p0/I stage were significant favorable factors with respect to OS. With respect to DFS, achieving pN0 and p0/I stage were significant favorable factors. With respect to DMFS, low preoperative T-stage, achieving lower pT-stage (pT0/1 vs. pT2/3), achieving pN0, and achieving p0/I stage were significant favorable prognostic factors. For LRC, PORT was a significant favorable factor. By the multivariate analysis, only achieving p0/I stage was significant with respect to OS (Fig. 5, Table 4).
In newly diagnosed NSCLC patients, those with locally advanced stage III disease comprise approximately 30% to 40%. The stage IIIA NSCLC is a heterogenous group that includes unforeseen N2 disease that is unknown until thoracotomy, mediastinoscopic N2 disease, and clinically overt N2 disease based on chest CT scan (1). In unforeseen N2 disease, the complete resection rate ranged from 53% to 87%, and the long term survival rates ranged from 20% to 30% (12). In patients with N2 disease detected by radiologic or mediastinoscopic findings, the long-term survival rate following resection was usually lower than 10%, and these patients thus were thought to be unsuitable for upfront curative surgery (13, 14). To improve the local control and survival of patients with such marginally resectable or unresectable N2 disease, various clinical trials have been performed to find the optimal ways to combine TRT, chemotherapy, and surgery.
The potential advantages of the preoperative treatment strategy are the increased resection rate, decreased micrometastasis, and decreased surgical seeding, while the potential disadvantages are the possible delay in primary surgery and the increased surgical morbidity and mortality (15). Preoperative TRT and surgery, based on a few randomized trials, failed to improve survival rate when compared with surgery alone (16, 17). PORT for the patients with pN2 disease was the usually recommended practice, which, however, only contributed to the improvement in the loco-regional control, but not to the survival benefit (18). Most recent clinical trials, hence, applied preoperative chemotherapy and/or TRT and surgery for marginally resectable stage IIIA NSCLC. Randomized trials employing preoperative chemotherapy, however, showed controversial effects on the overall survival (2-4, 19). There are a few reports that survival rates were improved by preoperative chemotherapy (2, 3), however, these results were not conclusive as they are based on rather small number of patients, included patients with stage IIIB, and used inconsistent surgical nodal staging. Recent phase III report comparing preoperative chemotherapy and surgery versus surgery alone on histologically confirmed N2 positive stage IIIA NSCLC, failed to document the survival benefit by adding preoperative chemotherapy (median survival durations were 17 months and 16 months, respectively. p=0.527) (4).
There are less reports on preoperative CRCT and surgery than preoperative chemotherapy and surgery (5-10). Moreover, most of them were nonrandomized trials with a small number of patients, used inconsistent surgical nodal staging, included stage IIIB patients, and used variable dose schedules of TRT. Their results are generally encouraging, however. SWOG 8805 used conventional TRT (45 Gy, 1.8 Gy/fraction), concurrently with two cycles of cisplatin and etoposide for the patients with N2 or N3 disease proven by biopsy, and added CRCT boost if positive margins or positive nodes were detected on surgical specimen (5). The median survival duration was 13 months and the 3-yr overall survival rate was 27%. Choi et al. (6) used hyperfractionated TRT (42 Gy, 1.5 Gy/fraction, twice a day), concurrently with two cycles of chemotherapy (cisplatin, vinblastine, and fluorouracil) for the patients with N2 disease confirmed by mediastinoscopy, and administered postoperative TRT (12-18 Gy, 1.5 Gy/fraction, twice a day) concurrently with one cycle of chemotherapy. The median survival duration was 25 months and the 3-yr overall survival rate was 37%. We used conventional TRT (total 45 Gy, 1.8 Gy/fraction), concurrently with two cycles of cisplatin and etoposide for the patients with N2 disease confirmed by mediastinoscopy, and optional PORT if persistent N2 disease, positive/close resection margin, or high-risk N1 disease were found. In 38 resected patients, the median survival duration was 27 months and the 3-yr overall survival rate was 44%. A common finding of these three studies is that the survival benefit was observed in those who achieved down-staging following preoperative CRCT. Our study showed that the survival rate of the patients who achieved pN0 after preoperative CRCT was significantly increased compared with those who did not achieve pN0. Likewise, in SWOG 8805, the median survival durations and the 3-yr survival rates in patients with negative and positive lymph nodes on surgery were 30 months and 9 months, and 41% and 11%, respectively (5). Similar results were reported by Choi et al. (6): the 5-yr survival rates in patients with the postsurgical stage 0/I, II, and III were 79%, 42%, and 18%, respectively. Bueno et al. (20) also reported that pN0 after preoperative treatment was a favorable prognostic factor, where the 3-yr survival rates for the postsurgical state 0/I or II/III patients were 65% and 30%, respectively.
Recently, the long-term outcome of phase III randomized trial (INT 0139) comparing preoperative CRCT (45 Gy) and surgery with definitive CRCT (61 Gy) was reported (10). Although there was no significant difference in overall survival between two arms (median survival: 23.6 vs. 22.2 months, p=0.24; 5-yr survival: 27.2% vs. 20.3%, p=0.10), progression-free survival was significantly improved by adding surgical resection (median progression-free survival: 12.8 vs. 10.5 months, p=0.017; 5-yr progression-free survival: 22.4% vs. 11.1%, p=0.008). The treatment-related mortality rate, however, was higher by surgical resection (7.9% vs. 2.1%, p=0.021), especially when pneumonectomy was necessary, and achieving pN0 stage significantly improved long-term survival compared with pN1-3 and no surgery (41% vs. 24% vs. 8%, p<0.0001).
Roberts et al. (21) reported that preoperative treatment might have increased the perioperative morbidity and mortality, while, however, others reported no increased risk (22, 23). Choi et al. (6) and Weitberg et al. (7) reported approximately 5% perioperative mortality rates. In our study, only one patient died after pneumonectomy. Preoperative CRCT and surgery performed under the strong team work of the expert specialists is an important factor to improve the survival without increasing perioperative morbidity and mortality (24).
Although preoperative CRCT has been reported to effectively lower local recurrence in patients with locally advanced NSCLC, the optimal dose schedule of radiation therapy is yet unclear. Vora et al. (8) applied high dose TRT (total 59.4 Gy) concurrently with chemotherapy followed by surgery in 33 patients with stage IIIA or IIIB NSCLC, and reported that no local failure was observed among 9 patients who achieved complete pathologic response following preoperative CRCT (27%). Weitberg et al. (7), who applied 55.8 Gy preoperative TRT concurrently with chemotherapy in 27 stage IIIA patients, reported that tumors were not detected in 44% of the resection specimens (12/27), among who two patients developed local relapse. These suggest that preoperative CRCT with high dose TRT be an effective way to improve local control. SWOG 8805 (5) applied boost CRCT (14.4 Gy) to patients with unresectable disease, positive margin, incomplete resection, or positive mediastinal nodes, and reported that the grade 4 toxicities occurred in 11% of the patients and three mortality cases were related to boost CRCT. Choi et al. (6) applied 12 Gy boost CRCT to the patients with pathologic complete or near complete remission, or alternately, 18 Gy boost CRCT to the patients with residual disease at the resection margins or resected specimen, however, did not analyze the impact of boost CRCT. We applied less aggressive TRT dose (45 Gy) and decided to add boost irradiation optionally based on the surgical and pathologic findings. There were two recurrences within the TRT volume among 7 patients who were with risk factors but did not receive PORT, however, there was only one recurrence within the TRT volume among 14 patients who had no risk factors and did not receive PORT, and no loco-regional recurrence within the TRT volume among 17 patients who had risk factors and received PORT. Hence, our treatment protocol of adding PORT optionally based on the surgical and pathologic findings is considered quite reasonable in the respect of selecting the patients who would have more benefit from PORT. In general, PORT, however, did not influence distant metastasis, disease-free survival, and overall survival. Study with more patients and longer follow-up would be necessary to investigate the exact role of PORT.
In many studies with preoperative CRCT including ours, distant metastasis occurred in 40% to 60% of patients, whereas loco-regional failure occurred in approximately 10% (5, 6, 8, 11). It has been shown that the response to the preoperative chemotherapy or CRCT has the impact on survival rate (5, 6, 20). Therefore, further study is needed to develop more effective chemotherapy regimen that can prevent distant metastasis and improve the response to the preoperative treatment.
By applying preoperative CRCT and surgery for N2 positive stage IIIA NSCLC patients, authors could achieve improved survival results comparable with other reports. The postoperative disease stage is a significant prognostic factor of overall survival, and further refinement of multimodality combined treatment approach for more effective reduction of distant metastasis may be warranted.
Figures and Tables
Fig. 1
Treatment scheme. Risk factors, by which the addition of postoperative radiation therapy was considered, included incomplete resection, positive/close resection margins, pN2, and high-risk pN1 diseases.

Fig. 2
The patterns of failure in relation to post-surgical risk factors and postoperative radiation therapy (PORT). DM, distant metastasis; LR, local recurrence; NED, no evidence of disease; PS, pleural seeding; RR, regional recurrence. Asterisk denotes failure within the thoracic radiation therapy volume.

Fig. 4
Disease-free survival rates of 38 patients who underwent resection. DFS, disease-free survival rate; LRRFS, loco-regional recurrence-free survival rate; DMFS, distant metastasis-free survival rate.
References
1. Shields TW. The significance of ipsilateral mediastinal lymph node metastasis (N2 disease) in non-small cell carcinoma of the lung. A commentary. J Thorac Cardiovasc Surg. 1990. 99:48–53.
2. Roth JA, Atkinson EN, Fossella F, Komaki R, Bernadette RM, Putnam JB Jr, Lee JS, Dhingra H, De Caro L, Chasen M, Hong WK. Long-term follow-up of patients enrolled in a randomized trial comparing perioperative chemotherapy and surgery with surgery alone in resectable stage IIIA non-small-cell lung cancer. Lung Cancer. 1998. 21:1–6.

3. Rosell R, Gomez-Codina J, Camps C, Javier SJ, Maestre J, Padilla J, Canto A, Abad A, Roig J. Preresectional chemotherapy in stage IIIA non-small-cell lung cancer: a 7-year assessment of a randomized controlled trial. Lung Cancer. 1999. 26:7–14.

4. Nagai K, Tsuchiya R, Mori T, Tada H, Ichinose Y, Koike T, Kato H. A randomized trial comparing induction chemotherapy followed by surgery with surgery alone for patients with stage IIIA N2 non-small cell lung cancer (JCOG 9209). J Thorac Cardiovasc Surg. 2003. 125:254–260.

5. Albain KS, Rusch VW, Crowley JJ, Rice TW, Turrisi AT 3rd, Weick JK, Lonchyna VA, Presant CA, McKenna RJ, Gandara DR. Concurrent cisplatin/etoposide plus chest radiotherapy followed by surgery for stages IIIA (N2) and IIIB non-small-cell lung cancer: mature results of Southwest Oncology Group phase II study 8805. J Clin Oncol. 1995. 13:1880–1892.

6. Choi NC, Carey RW, Daly W, Mathisen D, Wain J, Wright C, Lynch T, Grossbard M, Grillo H. Potential impact on survival of improved tumor downstaging and resection rate by preoperative twice-daily radiation and concurrent chemotherapy in stage IIIA non-small-cell lung cancer. J Clin Oncol. 1997. 15:712–722.

7. Weitberg AB, Yashar J, Glicksman AS, Posner M, Cummings F, Browne M, Clark J, Calabresi P, Beitz J, Murray C. Combined modality therapy for stage IIIA non-small cell carcinoma of the lung. Eur J Cancer. 1993. 29A:511–515.

8. Vora SA, Daly BD, Blaszkowsky L, McGrath JJ, Bankoff M, Supran S, Dipetrillo TA. High dose radiation therapy and chemotherapy as induction treatment for stage III nonsmall cell lung carcinoma. Cancer. 2000. 89:1946–1952.

9. Ahn YC, Park K, Kim DY, Kim KM, Kim J, Shim YM, Lee KS, Han J, Kim HJ, Kwon J, Lim DH, Noh YJ, Lee JE, Huh SJ. Preoperative concurrent chemoradiotherapy for stage IIIA non-small cell lung cancer. Acta Oncol. 2001. 40:588–592.
10. Albain KS, Swann RS, Rusch VR, Turrisi AT, Shepherd FA, Smith CJ, Gandara DR, Johnson DH, Green MR, Miller RC. Phase III study of concurrent chemotherapy and radiotherapy (CT/RT) vs CT/RT followed by surgical resection for stage IIIA (pN2) non-small cell lung cancer (NSCLC): Outcomes update of North American Intergroup 0139 (RTOG 9309). J Clin Oncol. 2005. 23:16S. 7014.
11. DeCamp MM, Rice TW, Adelstein DJ, Chidel MA, Rybicki LA, Murthy SC, Blackstone EH. Value of accelerated multimodality therapy in stage IIIA and IIIB non-small cell lung cancer. J Thorac Cardiovasc Surg. 2003. 126:17–27.

12. De Leyn P, Schoonooghe P, Deneffe G, Van Raemdonck D, Coosemans W, Vansteenkiste J, Lerut T. Surgery for non-small cell lung cancer with unsuspected metastasis to ipsilateral mediastinal or subcarinal nodes (N2 disease). Eur J Cardiothorac Surg. 1996. 10:649–654.
13. Pearson FG, DeLarue NC, Ilves R, Todd TR, Cooper JD. Significance of positive superior mediastinal nodes identified at mediastinoscopy in patients with resectable cancer of the lung. J Thorac Cardiovasc Surg. 1982. 83:1–11.

14. Martini N, Flehinger BJ. The role of surgery in N2 lung cancer. Surg Clin North Am. 1987. 67:1037–1049.

15. Vokes EE, Weichselbaum RR. Concomitant chemoradiotherapy: rationale and clinical experience in patients with solid tumors. J Clin Oncol. 1990. 8:911–934.

16. Warram J. Preoperative irradiation of cancer of the lung: final report of a therapeutic trial. A collaborative study. Cancer. 1975. 36:914–925.
17. Shields TW, Higgins GA Jr, Lawton R, Heilbrunn A, Keehn RJ. Preoperative x-ray therapy as an adjuvant in the treatment of bronchogenic carcinoma. J Thorac Cardiovasc Surg. 1970. 59:49–61.

18. PORT Meta-analysis Trialists Group. Postoperative radiotherapy in non-small-cell lung cancer: systematic review and meta-analysis of individual patient data from nine randomised controlled trials. Lancet. 1998. 352:257–263.
19. Depierre A, Milleron B, Moro-Sibilot D, Chevret S, Quoix E, Lebeau B, Braun D, Breton JL, Lemarie E, Gouva S, Paillot N, Brechot JM, Janicot H, Lebas FX, Terrioux P, Clavier J, Foucher P, Monchatre M, Coetmeur D, Level MC, Leclerc P, Blanchon F, Rodier JM, Thiberville L, Villeneuve A, Westeel V, Chastang C. Preoperative chemotherapy followed by surgery compared with primary surgery in resectable stage I (except T1N0), II, and IIIa non-small-cell lung cancer. J Clin Oncol. 2002. 20:247–253.

20. Bueno R, Richards WG, Swanson SJ, Jaklitsch MT, Lukanich JM, Mentzer SJ, Sugarbaker DJ. Nodal stage after induction therapy for stage IIIA lung cancer determines patient survival. Ann Thorac Surg. 2000. 70:1826–1831.

21. Roberts JR, Eustis C, Devore R, Carbone D, Choy H, Johnson D. Induction chemotherapy increases perioperative complications in patients undergoing resection for non-small cell lung cancer. Ann Thorac Surg. 2001. 72:885–888.

22. Sonett JR, Krasna MJ, Suntharalingam M, Schuetz J, Doyle LA, Lilenbaum R, Gamliel Z. Safe pulmonary resection after chemotherapy and high-dose thoracic radiation. Ann Thorac Surg. 1999. 68:316–320.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download