Abstract
We reviewed our experience with resection of recurrent lung cancer to evaluate the benefit and risk of the procedure. From December 1994 to December 2003, 29 consecutive patients underwent pulmonary resections for recurrent lung cancer. The mean duration from the first resection to second surgery was 25.4±15.1 months for the definite 2nd primary lung cancer (n=20) and 8.9±5.7 months for metastatic lung cancer (n=9). The procedures at the second operations were completion-pneumonectomy in 11 patients, lobectomy in 5 patients, wedge resection in 12 patients and resection and anastomosis of trachea in 1 patient. Morbidity was observed in 6 (21%) of the patients and the in-hospital mortality was two patients (7%) after the repeated lung resection. Tumor recurrence after reoperation was observed in 14 patients (48%). The actuarial 5-yr survival rate was 69% and the 5-yr disease free rate following reoperation was 44%. No significant difference was found in overall survival and disease free survival between the 2nd primary lung cancer group and the metastatic lung cancer group. The recurrence rate following reoperation was significantly different between the wedge resection group and lobectomy/completion pneumonectomy group (p=0.008), but the survival rate was not significantly different (p=0.41). Surgical intervention for recurrent lung cancers can be performed with acceptable mortality and morbidity. If tolerable, completion pneumonectomy or lobectomy is recommended for resection of recurrent lung cancer.
The recurrence of lung cancer after complete resection generally results in a poor prognostic situation with less than one year of life expectancy. When a single lung nodule is detected during follow-up, it is usually one of the manifestations of the systemic metastasis. However, one distinct feature is a second primary metachronous lung cancer appearing after the initial treatment of the primary lung cancer. Although there are criteria that can be applied in this situation, it is sometimes very difficult in clinical practice to distinguish between a new lung cancer and a metastatic one. Therefore, some researchers have insisted an aggressive surgical approach, whenever possible, as the survival rate after surgery is quite good (1-7). On the other hand, many doubts have been expressed concerning the utility of repeated surgery for recurrent lung cancer, as it is associated with a poor overall survival (8, 9).
We are convinced of the value of the aggressive surgical approach for all the cases whose the functional condition makes resection possible. The aim of this study is to report the result of re-resection for recurrent lung cancer while focusing on the rationale for this aggressive surgical approach.
There were 1,461 patients who underwent operations for primary lung cancer from December 1994 to December 2003. The operations were performed by a group of three thoracic surgeons in a single hospital. Every patient was followed-up by the same surgeons on a regular follow-up schedule (every 3-4 months for 2 yr, every 6 months for the next 3 yr and then every year). A chest CT was performed at every visit. When recurrent disease in the lung was suspected, repeated CT scan were performed at 2 months intervals, and positron emission tomography (PET), bronchoscopy and/or percutaneous needle aspiration (PCNA) were also performed. There were 29 consecutive patients who underwent repeated surgical resections for recurrent lung cancer after curative resection for lung cancer. At the time of initial operation, histology and pathological staging are shown in Table 1. The diagnostic methods of recurrent lung cancer were chest CT in 11 patients, PET in 9 patients, PCNA in 6 patients, and bronchoscopic biopsy in 3 patients. The second primary lung cancers were defined using the criteria outlined by Martini and Melamed (10). A neoplasm was defined as a metastatic lung cancer if it was a same histology occurring in the same anatomic site within 2 yr after first operation. A second primary cancer was a tumor of different histology, or if histology was the same, the disease free interval of recurrent cancers was at least 2 yr or the second cancer was in different lobe or lung, or origin from carcinoma in situ in the absence of other extrapulmonary or common lymphatic metasitasis. On the repeated lung operations, mediastinoscopy was not performed because most of the patients already had had mediastinoscopy performed at the first lung resection. However, careful intraoperative nodal staging was performed by dissecting the intrapulmonary, hilar and ipsilateral mediastinal nodes. Although the extent of resection of recurrent lung cancer in early period was dependent on the surgeon's preference, thereafter we have made an attempt to avoid limited resection if patients had predictive post-operative FEV1 of more than 1.0 L and acceptable cardiac function. Postoperatively, the same follow-up plan was applied as for the first lung operation.
We analyzed included types of operation, the time between two surgical interventions, operative findings and histology, operative and post-operative complications and the hospital mortality as well as late death. The descriptive statistics are summarized as the median or mean for the continuous variables and as frequencies and percentages for the categorical variables. Survival and the disease free rate were analyzed by the Kaplan-Meier and log-rank methods on SPSS for Window, release 10.0 (SPSS Inc., Chicago, IL, U.S.A.). All differences were considered significant at a p value less than 0.05.
29 consecutive patients underwent surgical resections for recurrent lung cancer after curative resection for lung cancer. The second primary lung cancer, by definition, was found in 20 cases. The remainder 9 cases were metastatic lung cancers. The median age of patients was 61 yr (range, 45 to 75 yr) and the male/female (22/7) ratio was 3.1:1. The smoking history was observed in 16 patients (55%). The second primary tumor was discovered on the same side as the first tumor in 19 patients. One had a histologically different tumor.
The mean time interval between the first operation and the second operation was 20.3±15 months (Table 1). The mean time interval between the first resection and the second resection was 25.4±15.1 months for the second primary lung cancers and 8.9±5.7 months for the metastatic lung cancer. The mean interval between the second operation and the second recurrence was 12.5±10.2 months.
The second operations were completion pneumonectomy in 11 patients, lobectomy in 5 patients, wedge resection in 12 patients, and resection and anastomosis of the trachea in 1 patient (Table 2). The patient of tracheal resection was recurred at right lower paratracheal lymph node. Three patients received adjuvant chemotherapy and one patient received radiation therapy. The operative mortality rate was 6.8%. The causes of death were pulmonary embolism in one patient and respiratory failure in the other patient. Major morbidity was observed in 6 (21%) patients after the repeated lung resection; bronchopleural fistula was noted in 3 patients, myocardial infarction and cerebral vascular accident were noted in 1 patient, pulmonary artery embolism occurred in 1 patient and respiratory failure occurred in 1 patient. Tumor recurrence after reoperation was observed in 14 patients (48%). In four of these 14 patients, we performed the third operation; a completion pneumonectomy in 1 patient, wedge resection in 2 patients and multiple rib resection and chest wall reconstruction in 1 patient. The remaining ten patients were referred for radiation therapy, chemotherapy or supportive care only (Table 4).
Overall follow-up after reoperation ranged from 3 to 103 months with a mean of 41.4±22.3 months. The overall actuarial 5-yr survival rate was 69% and the 5-yr disease free rate following reoperation was 44% (n=29). No significant difference was detected in survival and the disease free rate between the second primary lung cancer patients and the metastatic lung cancer patients (Table 3, Fig. 1, 2). The disease free rate following reoperation was significantly different between the wedge resection group and anatomically curative resections such as lobectomy/completion pneumonectomy group (p=0.008), but the survival rate was not significantly different (Fig. 3).
Recent improvements of such diagnostic tools as high-resolution CT scan or PET scan allow physicians to detect recurrent lung cancer much earlier than before. However, there is not yet a consensus for the postoperative follow-up strategy of patients after complete resection for NSCLC. Westeel et al. (11) and Angeletti et al. (1) reported that intensive follow-up may improve patient survival by detecting recurrences at an asymptomatic stage after surgery for NSCLC. It has been reported that for detecting residual or recurrent NSCLC, PET had a sensitivity of 100% and a specificity of 61.5-92%, but chest CT only had a sensitivity of 67% and a specificity of 85% for the detection of tumor recurrence (12). In our study, when the lesion was centrally located and the percutaneous needle aspiration was difficult to perform, PET was then used as a very effective diagnostic method. In our series, the diagnostic methods of recurrent lung cancer were chest CT in 11 patients, PET in 9 patients, PCNA in 6 patients, and bronchoscopic biopsy in 3 patients. When the recurrent lung cancer was difficult to diagnose with using chest CT or PET, we then performed invasive diagnostic methods. The initiation of earlier therapy with the early detection of recurrences may have improved the outcome compared with the therapy given when the patient becomes symptomatic from the tumor (1, 3, 4, 6). Major complications occurred in 24% of our patients after the second resections, which is comparable to the previously reported results of pulmonary resection for recurrent lung cancers (3, 4, 17).
Martini and Melamed (10) in 1975 outlined the criteria for differentiation between a second primary lung cancer and a metastatic or recurrent lung cancer. Some reports have suggested that patients with a second primary lung cancer have a more favorable prognosis than patients with locally recurrent or metastatic disease (13-15). However, other reports did not reveal a significantly different survival between patients operated on for a second primary lung cancer or those patients operated on for locally recurrent or metastatic disease (4, 5, 8, 9). Our data showed that the 5-yr survival rates were not different between second primary lung cancer and the possible second primary or metastatic lung cancer. Yet the 5-yr disease free rates for lobectomy/completion pneumonectomy group were better than for wedge resection group. It may be explained by the fact that the second operations had been wedge resections for eight patients of the second primary lung cancer subgroup (n=12) who had suffered a second tumor recurrence. The Lung Cancer Study Group (16) reported that a resection that is less extensive than lobectomy for primary lung cancer places the patient at an increased risk of local recurrence and this decreases the chances of long term survival. The limited resections used in second primary lung cancer group might have resulted in an increased risk for locoregional recurrence, but the extents of the resection of recurrent lung cancer did not influence the survival in another study (6, 17). Donington et al. (7) reported that pulmonary resection of bronchogenic carcinoma after pneumonectomy was associated with acceptable morbidity and mortality. Wedge resection, when feasible, is the treatment of choice.
Voltolini et al. (4) has reported on the type of surgical treatment used in case of metachronous second primary lung tumor. The wedge resection was a reasonable and safe alternative to the standard resections in the elderly patients or in those patients with a poor respiratory reserve and after a pneumonectomy. If the tumor was not in the periphery and if it was less than 2 cm in diameter, they consider lobectomy as the treatment of choice even for the second resection. The recurrence rate was lower in the lobectomy/completion pneumonectomy group than in the wedge resection group.
The mean disease free time for lobectomy/completion pneumonectomy patients was longer than for the wedge resection patients. Eight patients, who had undergone wedge resection of second primary lung cancer, were proven to show recurrence. Therefore, lobectomy or completion pneumonectomy is preferred to wedge resection as an operation for a second primary lung cancer.
Surgical intervention for recurrent lung cancers can be performed with an acceptable mortality and morbidity. If it is tolerable, completion pneumonectomy or lobectomy are recommended procedures of choice for recurrent lung cancer.
Figures and Tables
Fig. 1
Actuarial survival for recurrent lung cancer with 2nd primary and metastatic tumor after the second operations.
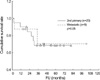
Fig. 2
Cumulative disease free rates of recurrent lung cancer with 2nd primary and metastatic tumor.
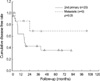
Fig. 3
Cumulative disease free rates for patients with lobectomy/c-pneumonectomy and wedge resection.
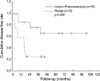
Table 4
The second recurrent lung cancer

s-RUL, sleeve right upper lobectomy; RML, right middle lobectomy; RLL, right lower lobectomy; LUL, left upper lobectomy; LLL, left lower lobectomy; LP, left pneumonectomy; W-, wedge resection; R & A, resection and anastomosis of trachea; c-RP, completion right pneumonectomy; c-LP, completion left pneumonectomy; RT, radiation therapy; Op., multiple ribs resection and chest wall reconstruction.
References
1. Angeletti CA, Mussi A, Janni A, Lucchi M, Ribechini A, Chella A, Fontanini G. Second primary lung cancer and relapse: treatment and follow-up. Eur J Cardiothorac Surg. 1995. 9:607–611.

2. Antakli T, Schaefer RF, Rutherford JE, Read RC. Second primary lung cancer. Ann Thorac Surg. 1995. 59:863–867.

3. Asaph JW, Keppel JF, Handy JR Jr, Douville EC, Tsen AC, Ott GY. Surgery for second lung cancers. Chest. 2000. 118:1621–1625.

4. Voltolini L, Paladini P, Luzzi L, Ghiribelli C, Bisceglie MD, Gotti G. Iterative surgical resections for local recurrent and second primary bronchogenic carcinoma. Eur J Cardiothorac Surg. 2000. 18:529–534.

5. Fujimoto T, Zaboura G, Fechner S, Hillejan L, Schroder T, Marra A, Krbek T, Hinterthaner M, Greschuchna D, Stamatis G. Completion pneumonectomy: current indications, complications, and results. J Thorac Cardiovasc Surg. 2001. 121:484–490.

6. Aziz TM, Saad RA, Glasser J, Jilaihawi AN, Prakash D. The management of second primary lung cancers. A single centre experience in 15 years. Eur J Cardiothorac Surg. 2002. 21:527–533.

7. Donington JS, Miller DL, Rowland CC, Deschamps C, Allen MS, Trastek VF, Pairolero PC. Subsequent pulmonary resection for bronchogenic carcinoma after pneumonectomy. Ann Thorac Surg. 2002. 74:154–159.

8. Regnard JF, Icard P, Magdeleinat P, Jauffret B, Fares E, Levasseur P. Completion pneumonectomy: experience in eighty patients. J Thorac Cardiovasc Surg. 1999. 117:1095–1101.

9. Terzi A, Lonardoni A, Falezza G, Scanagatta P, Santo A, Furlan G, Calabro F. Completion pneumonectomy for non-small cell lung cancer: experience with 59 cases. Eur J Cardiothorac Surg. 2002. 22:30–34.

10. Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg. 1975. 70:606–612.

11. Westeel V, Choma D, Clement F, Woronoff-Lemsi MC, Pugin JF, Dubiez A, Depierre A. Relevance of the intensive postoperative follow-up after surgery for non-small cell lung cancer. Ann Thorac Surg. 2000. 70:1185–1190.
12. Haberkorn U. Positron emission tomography (PET) of non-small cell lung cancer. Lung Cancer. 2001. 34:S115–S121.

13. McGovern EM, Trastek VF, Pairolero PC, Payne WS. Completion pneumonectomy: indications, complications, and results. Ann Thorac Surg. 1988. 46:141–146.

14. Gregoire J, Deslauriers J, Guojin L, Rouleau J. Indications, risk, and results of completion pneumonectomy. J Thorac Cardiovasc Surg. 1993. 105:918–924.
15. Okada M, Tsubota N, Yoshimura M, Miyamoto Y. Operative approach for multiple primary lung carcinomas. J Thorac Cardiovasc Surg. 1998. 115:836–840.

16. Lung Cancer Study Group. Randomized trial of lobectomy versus limited resection for T1N0 non-small cell lung cancer. Ann Thorac Surg. 1995. 60:615–623.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download