Abstract
To evaluate the expressions of cyclooxygenase-2 (COX-2) and inducible nitric oxide synthase (iNOS) in thyroid neoplasms in a Korean population, we studied a total of 154 cases: papillary carcinoma of classical type (PTC), 86; follicular adenoma (FA), 21; follicular carcinoma (FC), 35; medullary carcinoma (MC), 3; undifferentiated carcinoma (UC), 5; and Hurthle cell neoplasm (HN), 4. Using immunohistochemical staining, COX-2 expression was detected in 62 (72.1%) PTC specimens, 5 (23.8%) FA specimens, 10 (28.6%) FC specimens, 0 (0.0%) MC specimens, 1 (20.0%) UC specimen, and 3 (75%) HN specimens. iNOS expression was detected in 66 (76.7%) PTC specimens, 4 (19.0%) FA specimens, 13 (37.1%) FC specimens, 0 (0.0%) MC specimens, 3 (60.0%) UC specimens, and 4 (100%) HN specimens. The results showed that COX-2 and iNOS were frequently expressed in the PTC and HN specimens, and iNOS was more frequently overexpressed in the FC specimens than in the FA specimens. In PTC, COX-2 and iNOS were significantly overexpressed in patients over 45 yr of age (p=0.029, p=0.041), and iNOS expression was increased in patients with a large primary tumor (p=0.028). These results suggest that the upregulation of COX-2 and iNOS may contribute to the tumor progression of thyroid gland, particularly in PTC and HN, and iNOS may play an adjuvant role during the tumor progression of FC.
Cyclooxygenases (COXs) are the key enzymes in the conversion of arachidonic acid to prostaglandins. There are two COX isoforms-COX-1 and COX-2. COX-1 is constitutively expressed in most tissues and produces prostaglandins for homeostatic functions (1, 2). COX-2 is highly inducible at inflammation sites and is associated with various human tumors such as colonic carcinoma (3), gastric carcinoma (4), prostate carcinoma (5), malignant melanoma (6), or high-grade gliomas (7). COX-2 expression in tumor cell lines is also upregulated during increased proliferation (8), inhibition of apoptosis (9), and neoangiogenesis (10). Recent studies indicate that COX-2 is overexpressed in several thyroid carcinomas, particularly papillary carcinoma (11-14).
Nitric oxide is produced from L-arginine by nitric oxide synthase (NOS). NOS has one inducible isoform, iNOS, and two constitutively expressed isoforms; endothelial NOS and neuronal NOS (15). Among all the three NOS isoforms, iNOS synthesizes the largest amount of nitric oxide released by cells in response to cytokines or other agents (16). The overexpression of iNOS has been demonstrated in chronic inflammatory diseases as well as human tumors, including tumors of the breast, ovary, stomach, head and neck, and central nervous system (17-21). It has been reported that iNOS plays an important role in tumorigenesis as a mediator of carcinogenic nitrosamine formation, DNA damage, neovascularization (22), and apoptosis (23). A few studies have demonstrated that iNOS is overexpressed in several benign and malignant thyroid lesions (24, 25).
The aim of the present study was to examine the differences in the immunohistochemical expressions of the COX-2 and iNOS proteins in thyroid neoplasms. Further, we analyzed several clinicopathological findings, patient age, tumor size, thyroid capsular invasion, and lymph node metastasis, in papillary carcinoma cases.
Samples were selected from 154 patients at the Department of Pathology, Eulji University Hospital (Daejeon, Korea), and Chungnam National University Hospital (Daejeon, Korea) between 1994 and 2003. The diagnoses included papillary carcinoma with classical type (PTC) (n=86), follicular adenoma (FA) (n=21), follicular carcinoma (FC) (n=35), medullary carcinoma (MC) (n=3), undifferentiated carcinoma (UC) (n=5), and Hurthle cell neoplasm (HN) (Hurthle cell adenoma, n=2; Hurthle cell carcinoma, n=2). Each specimen was subjected to histological evaluation to confirm the diagnosis, while the relevant clinicopathological information was retrospectively abstracted from patient records. The histopathological slides were reviewed by three pathologists.
The specimens were formalin-fixed and paraffin-embedded blocks. The tissue blocks were freshly cut into 3 µm thick sections onto glass slides. Tissue sections were then deparaffinized in xylene and rehydrated through graded alcohol and deionized water. Afterwards the sections were heated in a microwave oven in 10 mM citrate buffer (pH 6.0) for 15 min at 100℃ for antigen unmasking. Endogenous peroxidase activity of the tissues was inactivated by 10 min incubation in 3% hydrogen peroxide. To block non-specific binding sites, the slides were then treated with 5% goat serum for 15 min at room temperature. The sections were incubated for one hour at room temperature with primary antibody to either COX-2 mouse antihuman monoclonal antibody at a dilution of 1:100 (Mouse anti-COX-2, Clone: COX 229; Zymed laboratories Inc., South San Francisco, CA, U.S.A.) or with iNOS epitope specific rabbit antibody at a dilution of 1:100 (Nitric oxide synthase, inducible: RB-9242-P; Lab vision, Fremont, CA, U.S.A.). After incubation with the primary antibody, the sections were processed using standard avidin-biotin immunohistochemistry, according to the manufacturer's recommendations (Vectastain ABC Elite kit; Vector Laboratories, Burlingame, CA, U.S.A.). Negative controls for the specificity of anti-COX-2 or anti-iNOS antibody were used by omitting the primary antibody, and these were prepared using mouse and rabbit immunoglobulins instead of using each primary antibody individually. Thirty paraffin blocks of normal thyroid tissue were used as negative controls.
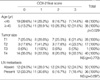
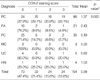
The intensity of the staining was scored 0-3 (absent, mild, moderate, strong) (Fig. 1, 2) and the area of positivity was estimated as the percentage of the total area of the tumor (<10%, 10-50%, and >50%). The final score was a combination of these two variables and was calculated as follows: score 0, negative staining or intensity 1+area <10%; score 1, intensity 1+area between 10% and 100% or intensity 2-3+area <10%; score 2, intensity 2+area >50% or intensity 3+area between 10% and 50%; score 3, intensity 3+area >50%. A final score of 1-3 was defined as positive immunoreactivity. The scoring was performed independently and in a blinded manner by three pathologists who had no knowledge of the clinical data. Discrepant scoring was determined by consensus.
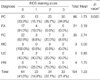
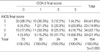
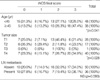
Cytoplasmic COX-2 expression (final scores 1-3) was detected in 62 (72.1%) PTC specimens, 5 (23.8%) FA specimens, 10 (28.6%) FC specimens, 0 (0.0%) MC specimen, 1 (20.0%) UC specimen, and 3 (75%) HN specimens. Cytoplasmic iNOS expression (final scores 1-3) was detected in 66 (76.7%) PTC specimens, 4 (19.0%) FA specimens, 13 (37.1%) FC specimens, 0 (0.0%) MC specimen, 3 (60.0%) UC specimens, and 4 (100%) HN specimens. The COX-2 and iNOS proteins were frequently expressed in the PTC and HN specimens. The mean of the COX-2 final scores was 1.37 in the PTC, 0.43 in the FA, 0.49 in the FC, 0.00 in the MC, 0.60 in the UC, and 1.50 in the HN specimens (Table 1). The mean of the iNOS final scores was 1.73 in the PTC, 0.19 in the FA, 0.74 in the FC, 0.00 in the MC, 0.80 in the UC, and 1.75 in the HN specimens. The mean value of the iNOS final scores in the FC specimens was greater than that in the FA specimens (Table 2). In the normal thyroid tissue, each final score with regard to COX-2 and iNOS expressions was zero. Significant positive correlations were detected between COX-2 and iNOS expressions (Table 3). In PTCs, COX-2 and iNOS expressions increased in the patients over 45 yr of age, and high iNOS expression correlated with the primary tumor size. However, COX-2 and iNOS expressions have not been shown to be associated lymph node metastasis at operation (Table 4, 5).
In this study, the final immunoreactive scores of COX-2 and iNOS expressions were significantly high in the PTC and HN specimens. In contrast, the FA, FC, MC, and UC specimens showed lower COX-2 and iNOS expressions. COX-2 overexpression was closely associated with iNOS expression. The positive correlation between COX-2 and iNOS expressions could be associated with a link between COX-2 and iNOS pathways because nitric oxide (the product of iNOS catalysis) is a regulator of COX-2 activity (26) and diverse prostaglandins (products of COX-2) may affect iNOS expression (26, 27). It has been observed that COX-2 plays important roles in tumor progression as mediators for the development of tumor vasculature (10), inhibition of apoptosis (9) and increasing tumor cell invasiveness (28, 29). Although the exact signaling pathways of COX-2-promoted tumorigenesis are yet unknown, several animal studies support a direct role of COX-2 in tumorigenesis since the genetic deletion of COX-2 suppresses tumor growth and multiplicity in mice (30).
Both COX-2 and iNOS overexpressions showed an age-associated increase in PTCs. Many authors have demonstrated an age-associated increase in COX-2 activity and prostaglandin E2 production in animal models (31), and Siironen et al. reported that COX-2 expression increased in older patients with PTC (11). They divided the patients into two groups; patients less than 35 yr of age and those older than 55 yr of age. Initially, Ito et al. had reported that COX-2 expression decreased with age in PTCs (32). They divided patients into those under and over 54 yr of age. But the Union Internationale Contre le Cancer TNM system classifies all PTC patients under 45 yr in a low-risk category, independent of tumor size, extent of tumor, lymph node metastasis, and distant metastasis (33). In our study, we divided PTC patients into two groups, namely, those under and over 45 yr of age and detected an age-associated increase in COX-2 and iNOS expressions. The results were in agreement with the report of Siironen et al. and demonstrated that the overexpression of COX-2 and iNOS could correlate with the more aggressive behavior of PTC.
Similar to the COX-2 expression, we detected iNOS overexpression in PTC and HN specimens and iNOS expression was increased in patients with a large primary tumor. The iNOS overexpression in the PTC specimens is in line with the previous reports (13, 25). Previous reports suggested that the nitric oxide released by iNOS might be involved in tumorigenesis as an inhibitor of epithelial cell apoptosis (23) and neoangiogenesis (34). With regard to the FA and FC specimens, iNOS overexpression was more frequently observed in the FC specimens than in the FA specimens. Among the FC specimens, there were 37.1% positive cases, whereas among the FA specimens, there were only 19.0% positive cases. Although this result is insufficient to arrive at a conclusion, we suggest that iNOS expression analysis could be helpful in understanding the tumor progression of FC.
Overexpression of the COX-2 protein in HN specimen has been reported previously (35), but the role played by COX-2 and iNOS in HN is unknown. A previous study has shown that COX-2 and iNOS are overexpressed in the swollen cytoplasm of the follicular cells in chronic lymphocytic thyroiditis (13). The swollen cytoplasm of the follicular cells in chronic lymphocytic thyroiditis and in our HN specimens may have a mitochondrial dysfunction that is related to COX-2 and iNOS.
We have not demonstrated COX-2 and iNOS expression in the three cases of MCs. However, Bell et al. reported COX-2 and iNOS expression in nine cases of MC along with immunohistochemical reactivity for COX-1 and COX-2 enzymes (36). Kim et al. reported that one of two MC cases showed immunohistochemical overexpression for COX-2 (35), and Choe et al. reported that all the five MC cases showed immunohistochemical overexpression for iNOS (24). The number of MC cases that we have reported here was too small for statistical analysis. The association of COX-2 and iNOS expressions with MC should be further investigated for better understanding of MC tumorigenesis.
In conclusion, the present immunohistochemical study has shown that overexpressions of the COX-2 and iNOS proteins were more frequently observed in PTC and HN specimens than other thyroid neoplasms. Further, FCs tended to show iNOS overexpression more frequently than FAs. The expressions of both COX-2 and iNOS increased in older PTC patients, and iNOS overexpression was correlated with the primary tumor size of PTC. These preliminary data suggest that COX-2 and iNOS expressions could be important molecular events for the tumor progression of PTC and HN, and iNOS expression could play a role in the tumor progression of FC.
Figures and Tables
Fig. 1
Immunohistochemical staining demonstrates the intensity of COX-2 expression in the cytoplasm of follicular carcinoma cases. (A) score 0; (B) score 1; (C) score 2; (D) score 3 (×400).
Fig. 2
Immunohistochemical staining demonstrates the intensity of iNOS expression in the cytoplasm of papillary carcinoma cases. (A) score 0; (B) score 1; (C) score 2; (D) score 3 (×400).
Table 4
Relationship between COX-2 final scores by immunohistochemical staining and clinicopathological features of papillary carcinoma of classical type
References
1. Dubois RN, Abramson SB, Crofford L, Gupta RA, Simon LS, van de Putte LB, Lipsky PE. Cyclooxygenase in biology and disease. FASEB J. 1998. 12:1063–1073.

2. Vane JR, Bakhle YS, Botting RM. Cyclooxygenases 1 and 2. Annu Rev Pharmacol Toxicol. 1998. 38:97–120.

3. Eberhart CE, Coffey RJ, Radhika A, Giardiello FM, Ferrenbach S, DuBois RN. Up-regulation of cyclooxygenase 2 gene expression in human colorectal adenomas and adenocarcinomas. Gastroenterology. 1994. 107:1183–1188.

4. van Rees BP, Saukkonen K, Ristimaki A, Polkowski W, Tytgat GN, Drillenburg P, Offerhaus GJ. Cyclooxygenase-2 expression during carcinogenesis in the human stomach. J Pathol. 2002. 196:171–179.

5. Madaan S, Abel PD, Chaudhary KS, Hewitt R, Stott MA, Stamp GW, Lalani EN. Cytoplasmic induction and over-expression of cyclooxygenase-2 in human prostate cancer: implications for prevention and treatment. BJU Int. 2000. 86:736–741.

6. Denkert C, Kobel M, Berger S, Siegert A, Leclere A, Trefzer U, Hauptmann S. Expression of cyclooxygenase 2 in human malignant melanoma. Cancer Res. 2001. 61:303–308.
7. Joki T, Heese O, Nikas DC, Bello L, Zhang J, Kraeft SK, Seyfried NT, Abe T, Chen LB, Carroll RS, Black PM. Expression of cyclooxygenase 2 (COX-2) in human glioma and in vitro inhibition by a specific COX-2 inhibitor, NS-398. Cancer Res. 2000. 60:4926–4931.
8. Fujita H, Koshida K, Keller ET, Takahashi Y, Yoshimito T, Namiki M, Mizokami A. Cyclooxygenase-2 promotes prostate cancer progression. Prostate. 2002. 53:232–240.

9. Kamijo T, Sato T, Nagatomi Y, Kitamura T. Induction of apoptosis by cyclooxygenase-2 inhibitors in prostate cancer cell lines. Int J Urol. 2001. 8:S35–S39.

10. Fosslien E. Review: molecular pathology of cyclooxygenase-2 in cancer-induced angiogenesis. Ann Clin Lab Sci. 2001. 31:325–348.
11. Siironen P, Ristimaki A, Nordling S, Louhimo J, Haapiainen R, Haglund C. Expression of COX-2 is increased with age in papillary thyroid cancer. Histopathology. 2004. 44:490–497.

12. Cornetta AJ, Russell JP, Cunnane M, Keane WM, Rothstein JL. Cyclooxygenase-2 expression in human thyroid carcinoma and Hashimoto's thyroiditis. Laryngoscope. 2002. 112:238–242.

13. Nose F, Ichikawa T, Fujiwara M, Okayasu I. Up-regulation of cyclooxygenase-2 expression in lymphocytic thyroiditis and thyroid tumors: significant correlation with inducible nitric oxide synthase. Am J Clin Pathol. 2002. 117:546–551.
14. Specht MC, Tucker ON, Hocever M, Gonzalez D, Teng L, Fahey TJ 3rd. Cyclooxygenase-2 expression in thyroid nodules. J Clin Endocrinol Metab. 2002. 87:358–363.

16. Assurey J, Canha FQ, Lew FY, Moncada S. Feedback inhibition of nitric oxide synthase activity by nitric oxide. Br J Pharmacol. 1993. 108:833–837.
17. Duenas-Gonzalez A, Isales CM, del Mar Abad-Hernandez M, Gonzalez-Sarmiento R, Sangueza O, Rodriguez-Commes J. Expression of inducible nitric oxide synthase in breast cancer correlates with metastatic disease. Mod Pathol. 1997. 10:645–649.
18. Thomsen LL, Lawton FG, Knowles RG, Beesley JE, Riveros-Moreno V, Moncada S. Nitric oxide synthase activity in human gynecological cancer. Cancer Res. 1994. 54:1352–1354.
19. Son HJ, Kim YH, Park DI, Kim JJ, Rhee PL, Paik SW, Choi KW, Song SY, Rhee JC. Interaction between cyclooxygenase-2 and inducible nitric oxide synthase in gastric cancer. J Clin Gastroenterol. 2001. 33:383–388.

20. Gavilanes J, Moro MA, Lizasoain I, Lorenzo P, Perez A, Leza JC, Alvarez-Vicent JJ. Nitric oxide synthase activity in human squamous cell carcinoma of the head and neck. Laryngoscope. 1999. 109:148–152.

21. Cobbs CS, Brenman JE, Aldape KD, Bredt DS, Israel MA. Expression of nitric oxide synthase in human central nervous system tumors. Cancer Res. 1995. 55:727–730.
22. Thomsen LL, Miles DW. Role of nitric oxide in tumor progression: lessons from human tumors. Cancer Metastasis Rev. 1998. 17:107–118.
23. Kim YM, Talanian RV, Billiar TR. Nitric oxide inhibits apoptosis by preventing increases in caspase-3-like activity via two distinct mechenisms. J Biol Chem. 1997. 272:31138–31148.
24. Choe W, Kim S, Hwang TS, Lee SS. Expression of inducible nitric oxide synthase in thyroid neoplasms: immunohistochemical and molecular analysis. Pathol Int. 2003. 53:434–439.

25. Kitano H, Kitanishi T, Nakanishi Y, Suzuki M, Takeuchi E, Yazawa Y, Kitajima K, Kimura H, Tooyama I. Expression of inducible nitric oxide synthase in human thyroid papillary carcinomas. Thyroid. 1999. 9:113–117.

26. Perez-Sala D, Lamas S. Regulation of cyclooxygenase-2 expression by nitric oxide in cells. Antioxid Redox Signal. 2001. 3:231–248.
27. Kobayashi O, Miwa H, Watanabe S, Tsujii M, Dubois RN, Sato N. Cyclooxygenase-2 downregulates inducible nitric oxide synthase in rat intestinal epithelial cells. Am J Physiol Gastrointest Liver Physiol. 2001. 281:G688–G696.

28. Ermert L, Dierkes C, Ermert M. Immunohistochemical expression of cyclooxygenase isoenzymes and downstream enzymes in human lung tumors. Clin Cancer Res. 2003. 9:1604–1610.
29. Sharma S, Stolina M, Yang SC, Baratelli F, Lin JF, Atianzar K, Luo J, Zhu L, Lin Y, Huang M, Dohadwala M, Batra RK, Dubinett SM. Tumor cyclooxygenase 2-dependent suppression of dendritic cell function. Clin Cancer Res. 2003. 9:961–968.
30. Oshima M, Dinchuk JE, Kargman SL, Oshima H, Hancock B, Kwong E, Trzaskos JM, Evans JF, Taketo MM. Suppression of intestinal polyposis in Apc delta716 knockout mice by inhibition of cyclooxygenase 2 (COX-2). Cell. 1996. 87:803–809.
31. Hayek MG, Mura C, Wu D, Beharka AA, Han SN, Paulson KE, Hwang D, Meydani SN. Enhanced expression of inducible cyclooxygenase with age in murine macrophages. J Immunol. 1997. 159:2445–2451.
32. Ito Y, Yoshida H, Nakano K, Takamura Y, Miya A, Kobayashi K, Yokozawa T, Matsuzuka F, Matsuura N, Kuma K, Miyauchi A. Cyclooxygenase-2 expression in thyroid neoplasms. Histopathology. 2003. 42:492–497.

33. Sobin L, Wittekind C, editors. TNM classification of malignant tumors. 1997. 5th edn. New York: Wiley-Liss, Inc.
34. Ziche M, Morbidelli L, Choudhuri R, Zhang HT, Donnini S, Granger HJ, Bicknell R. Nitric oxide synthase lies downstream from vascular endothelial growth factor induced but not basic fibroblast growth factor-induced angiogenesis. J Clin Invest. 1997. 99:2625–2634.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download