Abstract
We compared the effects of bladder training and/or tolterodine as first line treatment in female patients with overactive bladder (OAB). One hundred and thirty-nine female patients with OAB were randomized to treatment with bladder training (BT), tolterodine (To, 2 mg twice daily) or both (Co) for 12 weeks. Treatment efficacy was measured by micturition diary, urgency scores and patients' subjective assessment of their bladder condition. Mean frequency and nocturia significantly decreased in all treatment groups, declining 25.9% and 56.1%, respectively, in the BT group; 30.2% and 65.4%, respectively, in the To group; and 33.5% and 66.3%, respectively in the Co group (p<0.05 for each). The decrease in frequency was significantly greater in the Co group than in the BT group (p<0.05). Mean urgency score decreased by 44.8%, 62.2% and 60.2% in the BT, To, and Co groups, respectively, and the improvement was significantly greater in the To and Co groups than in the BT group (p<0.05 for each). Although BT, To and their combination were all effective in controlling OAB symptoms, combination therapy was more effective than either method alone. Tolterodine alone may be instituted as a first-line therapy, but may be more effective when combined with bladder training.
Overactive bladder (OAB), defined as increased frequency and urgency with or without urge incontinence, is a very common condition, especially in middle-aged women, with a reported incidence of approximately 17% of the general female population (1, 2). Since many women may consider OAB as a natural aging phenomenon and thus do not seek treatment, its actual prevalence may be even higher. Despite its common occurrence, however, our understanding (3-5) of the pathophysiology underlying the development of OAB has remained elementary. It is managed most commonly by drug therapy, followed by various behavioral interventions and, less frequently, by surgical methods. Each of these methods, however, has variable efficacy and adverse effects. Classically, urge incontinence has been considered most important, being the key index in treatment outcome assessments. However, since the new consensus by the International Continence Society on the diagnosis of OAB (6), the presence or absence of actual urine leakage was regarded as less important. With the adaptation of this new definition, the number of patients newly diagnosed with OAB is expected to increase, emphasizing the need to develop first-line interventions for their symptoms.
The three most commonly employed methods for treating newly-diagnosed OAB are bladder training, anticholinergic therapy and a combination of the two. Here we report a controlled, randomized study comparing the clinical efficacy of these three methods, for the purpose of determining the most appropriate first-line therapeutic modality.
Between May 2001 and April 2002, 139 women presenting with symptoms of urgency and frequency, with or without urge incontinence, were prospectively enrolled in this study. Inclusion criteria included being 18 yr of age or older, having a urination frequency of 8 or more times per day, the presence of urge symptoms that may or may not accompany incontinence, symptom duration of 3 months or longer and no prior history of treatment for OAB. We excluded patients with active urinary tract infection, clinically significant stress urinary incontinence, bladder outlet obstruction, interstitial cystitis, glaucoma or megacolon. Also excluded were patients with a maximal urine flow rate of less than 10 mL/sec or a postvoid residual urine amount that was more than 30% of the total amount voided on uroflowmetry.
Upon enrollment, patients were randomly assigned to bladder training (BT, n=46), tolterodine treatment (To, 2 mg twice daily, n=47) or a combination of the two (Co, n=46). Each patient received a physical examination and uroflowmetry with postvoid residual urine scan. In addition, each patient kept a record of urgency scores, with 0 indicating no symptoms, 1 rarely, 2 occasionally, 3 often, and 4 all the time, and a frequency-volume chart. At 12 weeks, satisfaction score was assessed, with 0 representing fully satisfied, 1 much improved, 2 slightly improved, 3 no improvement, and 4 worsened; a change of 2 points or more was considered symptom improvement. The frequency-volume chart and a survey of adverse effects of medication were repeated every 4 weeks.
Patients in the BT and Co groups were educated of the bladder drills by a nurse specialist. Gross and functional anatomy of the lower urinary tract and pelvis were demonstrated, with instructions on how bladder drills can increase functional bladder capacity and actual voiding habits. Each patient was instructed to examine her frequency-volume chart to determine the longest interval she could initially hold urination and sustain urge symptoms. Each patient was then taught to increase this interval by 15-min increments, with the aim of achieving a 3 to 4 hr interval and a voided volume of 300 to 400 mL. In addition, whenever urgency occurred, patients were educated to perform Kegel exercises for symptom alleviation. All bladder drill education was performed by one nurse specialist, who telephoned each patient every 2 weeks to make sure she was following the exact drill taught. In the Co group, the bladder drill was started at the same time as the start of medication.
Of the 139 patients, 89 (64.0%) completed the 12 week treatment regimen and were subjects of outcome analyses. Voiding frequency, nocturia, urgency score before and after the treatment, satisfaction score at 12 weeks and adverse events were measured in the three groups. Student's t-test was used for statistical analysis, and p<0.05 was defined as statistically significant.
Patient characteristics, including age, weight, symptom severity and duration, parity, pretreatment uroflowmetry profile, presence and degree of urge or stress incontinence, and urgency score, were similar among the three treatment groups (Table 1).
At 12 weeks, 26 patients (56.5%) in the BT group, 32 (68.1 %) in the To group, and 31 (67.4%) in the Co group had completed the protocol. Mean frequency in the three groups decreased significantly, from 10.9 to 8.1 (25.9%) in the BT group, from 11.6 to 8.1 (30.2%) in the To group, and from 11.9 to 7.9 (33.5%) in the Co group (p<0.05 each) (Fig. 1). Nocturia also decreased significantly in the three groups, from 1.5 to 0.6 per night (56.1%) in the BT group, from 1.7 to 0.6 (65.4%) in the To group, and from 2.0 to 0.6 (66.3%) in the Co group (p<0.05 each) (Fig. 2), as did urgency scores, from 2.6 to 1.4 (44.8%) in the BT group, from 2.8 to 1.1 (62.2%) in the To group, and from 3.0 to 1.2 (60.2%) in the Co group (p<0.05 each) (Fig. 3). When we compared these changes among the three groups, we found that patients in the Co group showed greater improvements in frequency and urgency scores than did patients in the BT group (p<0.05 each), and that urgency scores in the To and Co groups showed significantly greater improvement than in the BT group (p=0.017 and p=0.021, respectively). No difference was observed between the To and Co groups.
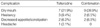
Satisfaction scores at 12 weeks did not differ among the three groups, being 1.5 in the BT group, with improvement in 53.9%; 1.4 in the To group, with improvement in 63.0%; and 1.3 in the Co group, with improvement in 71.0%. No adverse events were reported from the BT group, whereas 13 patients (40.6%) in the To group and 12 (38.7%) in the Co group reported one or more adverse events (Table 2). Most of the events were mild and well-tolerated, except that severe dry mouth occurred in 2 patients from each group, which led them to discontinue medication (withdrawal rates, 6.3% and 6.5%, respectively).
Despite extensive research on the complicated interactions involving the neural network of the cerebrum, sacral cord and the detrusor, little is known regarding the pathologic process that occurs during the development of OAB (4, 5, 7). Accordingly, therapeutic approaches for OAB have been diverse, consisting largely of medical therapy, but also including behavioral interventions such as bladder training, pelvic floor muscle exercises with or without biofeedback, and electrical stimulation. Other therapeutic approaches have included neuromodulation of the sacral nerves, intravesical instillations of antimuscarinics and bladder overdistention, with augmentation cystoplasty remaining as the last resort. Naturally, non-invasive methods, including medical therapy and behavioral intervention, have been the initial treatments of choice for OAB symptoms.
Although it is not known how bladder drills control and sustain OAB symptoms, it is believed that ill-trained voiding habits leading to decreased bladder compliance by frequent voiding are corrected by progressively increasing the voiding interval, thus increasing the voided volume and the functional bladder capacity. Retraining these patients to void at normal intervals would restore compliance when capacity increases and may contribute to symptom improvement (8-11). Observations on the electrical stimulation of the pelvic floor muscles (12) have shown that, during electrical stimulation, hyperactivity of the bladder was either diminished or completely abolished. This mechanism has been exploited as part of bladder training regimens.
Clinically, bladder training has been shown to be effective in the management of urgency and urge incontinence (8, 13-15). When bladder training was compared with medical therapy (200 mg flavoxate hydrochloride plus 25 mg imipramine three times daily for 4 weeks), urge incontinence was completely controlled in 84% of patients in the BT group, with symptom relief in 76%, compared with 56% and 48%, respectively, in the medication group (16). A larger study (17), however, found that addition of behavioral interventions did not seem to offer any additional benefit to medical therapy (tolterodine) after 6 months. Urgency episodes and daytime frequency decreased 83% and 27.3%, respectively, in the tolterodine group, compared with 78.7% and 23%, respectively, in the combination group. Improvements in patients' perception of urinary symptoms were reported by 85.9% of the tolterodine group and 81.7% of the combination group.
We found that all patients, a homogeneous group of female patients, regardless of treatment methodology, reported significant improvements in all voiding parameters examined, but that the addition of medication to BT resulted in additional improvements in urgency and frequency. Our finding of better outcomes in the Co than in the To group may be due to the bladder training program and design used here, which was a short-term intensive course of bladder drills. As many authors have emphasized, patients' understanding and compliance are the key factors in bladder training. Accordingly, the exercise program that we used did not simply require patients to contract and relax their pelvic floor muscles for certain periods of time. Instead, patients were given specific goals of 15 min each in sustaining contractions and were instructed how to increase these intervals. Having such a specific aim of what to accomplish with each exercise must have been enforcing and rewarding as well. In addition, repeated instructions, confirmation and reassurance were essential and constantly encouraged patients to stay on the right track for 12 weeks.
Similar results have been reported (18), in which patients were provided with written information sheets describing the aims and endpoints of therapy as well as specific instructions on bladder drills. Although there were no formal bladder training sessions or additional follow-up for those in the bladder training-only group, the self-explanatory information sheets the patients kept would have reinforced and encouraged patients while on bladder drills. Thus, patients on medication plus bladder training reported significantly better results after therapy than did patients on medication alone. In the previous study, in which the drills were simplified, it may have facilitated patient adherence to treatment, but without any further reinforcements, the therapeutic benefits of BT may have been compromised (17). In this study, we found that patient adherence to treatment was lowest and discontinuation rate highest in the BT group, although the treatment efficacy results were similar at the end of 12 weeks. This may be attributed to the longer duration of patient maneuvering required before experiencing significant improvement in this BT-only group. Thus, despite many efforts by the physician to make patients stay on the correct treatment regimen, it was evidently easier for patients to take medication twice a day than to repeat exercises many times a day for months.
We noted no adverse effects in the BT group, whereas, in the other 2 groups, the most common adverse effect was dry mouth. We found that 6.3% of patients in the BT group and 6.5% in the Co group had to discontinue medication due to severe dry mouth, percentages lower than those previously reported (19, 20). These results indicate that 4 mg/day tolterodine is safe and does not require dose adjustment.
From these results, we conclude that bladder training, tolterodine and the combination of the two are all effective in controlling OAB symptoms, with comparable patient satisfaction. Since a short-term intensive course of bladder drill is as effective as medical or combined therapy in all voiding symptoms, but does not have any adverse effects, bladder training can be safely and effectively employed as first line treatment for OAB. In patients who have predominantly symptoms of frequency or urgency, tolterodine may be more effective, especially when combined with bladder training.
Figures and Tables
Fig. 1
Changes in frequency after 12 weeks of treatment (*p<0.05). Improvement in the Co group was higher than BT group (†p=0.027).

Fig. 2
Changes in nocturia after 12 weeks of treatment (*p<0.05). Changes in nocturia did not differ among the groups.

References
1. Milsom I, Abrams P, Cardozo L, Roberts RG, Thuroff J, Wein AJ. How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int. 2001. 87:760–766.

2. Stewart WF, Van Rooyen JB, Cundiff GW, Abrams P, Herzog AR, Corey R, Hunt TL, Wein AJ. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003. 20:327–336.

3. Blok BF, Holstege G. The central control of micturition and continence: implications for urology. BJU Int. 1999. 83:1–6.

4. Igawa Y. Discussion: functional role of M1, M2, and M3 muscarinic receptors in overactive bladder. Urology. 2000. 55:47–50.

5. Fitzpatrick JM. Facts and future lines of research in lower urinary tract symptoms in men and women: an overview of the role of α1-adrenoreceptor antagonists. BJU Int. 2000. 85:1–5.
6. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A. Standardisation Subcommittee of the International Continence Society. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002. 21:167–178.

7. Artibani W. Diagnosis and significance of idiopathic overactive bladder. Urology. 1997. 50:25–32.

9. Elder DD, Stephenson TP. An assessment of the Frewen regime in the treatment of detrusor dysfunction in females. Br J Urol. 1980. 52:467–471.

10. Bo K, Berghmans LC. Nonpharmacologic treatments for overactive bladder-pelvic floor exercises. Urology. 2000. 55:7–11.

11. Burgio KL, Locher JL, Goode PS, Hardin JM, McDowell BJ, Dombrowski M, Candib D. Behavioral vs drug treatment for urge urinary incontinence in older women: a randomized controlled trial. JAMA. 1998. 280:1995–2000.

12. Godec C, Cass AS, Ayala GF. Bladder inhibition with functional electrical stimulation. Urology. 1975. 6:663–666.

13. Jeffcoate TN, Francis WJ. Urgency incontinence in the female. Am J Obstet Gynecol. 1966. 94:604–618.

14. Pengelly AW, Booth CM. A prospective trial of bladder training as treatment for detrusor instability. Br J Urol. 1980. 52:463–466.

15. Holmes DM, Stone AR, Bary PR, Richards CJ, Stephenson TP. Bladder training-3 years on. Br J Urol. 1983. 55:660–664.

16. Jarvis GJ. A controlled trial of bladder drill and drug therapy in the management of detrusor instability. Br J Urol. 1981. 53:565–566.

17. Millard RJ. Clinical efficacy of tolterodine with or without a simplified pelvic floor exercise regimen. Neurourol Urodyn. 2004. 23:48–53.

18. Mattiasson A, Blaakaer J, Hoye K, Wein AJ. Tolterodine Scandinavian Study Group. Simplified bladder training augments the effectiveness of tolterodine in patients with an overactive bladder. BJU Int. 2003. 91:54–60.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download