Abstract
This study aimed to document current cervical cancer screening practices of physicians in Korea. Questionnaires were distributed to 852 Korean obstetricians and gynecologists, who attended the 91st Conference of the Korean Society of Obstetrics and Gynecology held during May, 2005. Questionnaires were returned by 30.6% (260/852) of the recipients and 254 of these were eligible for analysis. Sixty-seven percent started cervical cancer screening women at age 20, and 65% replied that they would continue annual screening in a 35-yr-old woman with three consecutive normal cytologic tests. Over 65% of respondents preferred conventional cytologic screening to liquid-based cytology. The cost was a major determinant for selecting screening method. Fifty-three percent used the human papillomavirus DNA test as a triage for atypical squamous cells of undetermined significance. Our findings suggest that majority of Korean obstetricians and gynecologists in hospital prefer annual conventional cytologic testing to liquid-based cytology for financial reason.
Uterine cervical cancer is the second most frequently diagnosed gynecologic malignancy in women worldwide (1) and the fifth most common cancer among women after breast, stomach, colon-rectum, and thyroid cancer in Korea (2). An annual average incidence cases was about 4,360 composing 9.8% of all cancers in Korean women during 1999-2001 (2). Cervical cancer was the most common female cancer in the 1980s, but subsequently, the proportion of cervical cancer cases among all cancer cases in the Korea Central Cancer Registry reduced slightly. Moreover, a marked reduction in the incidence of this tumor has been documented over the past 2 decades, and this has been largely attributed to widespread screening and the early treatment of pre-invasive lesions (3-5). However, no similar decreases have been reported in other developed countries (6, 7).
The International Federation of Gynecology and Obstetrics reported 5-yr recurrence and a 5-yr overall mortality rates for cervical cancer of 28% and 27.8% respectively (8). The widespread use of Papanicolaou (Pap) tests for cervical cancer screening has resulted in a dramatic decrease in cervical cancer incidence and mortality over the several decades (9). Screening tests for cervical cancer offer reliable methods of reducing death from cervical cancer, despite the many publications that have documented above the low sensitivity of these techniques. The Korean Society of Obstetrics and Gynecology and the National Cancer Center have developed screening recommendations, and suggest that annual screening start with sexual activity or at age 20 yr. The Korean Ministry of Health and Welfare also developed a cervical cancer screening program in 2001, in which they suggested biannual screening of women over 30 yr of age using the Pap. The American Cancer Society (ACS) has recently revised its screening recommendations, and now suggests that screening start within 3 yr of sexual activity or at age 21, and that it should be less frequent than annually in women over 30 yr of age with a history of 3 or more normal tests. In addition, co-testing with human papillomavirus (HPV) and the discontinuance of screening was endorsed in certain women (10). The American College of Obstetrics and Gynecologists (ACOG) has also issued similar recommendations (11). However, despite national screening guidelines, little is known about patterns of obstetrician and gynecologist practices in this field.
The purpose of the present study was to characterize the cervical cancer screening practices of obstetricians and gynecologists in Korea.
At May, 2005, about 900 obstetricians and gynecologists attended the 91st Conference of the Korean Society of Obstetrics and Gynecology. Questionnaires were distributed to 852 physicians during the conference. Each physician received a cover letter, a copy of questionnaire, and a return envelope with postage paid. Authors also sent questionnaires to all conference attendees absent from the conference two weeks after the original distribution. Physicians were asked to complete the survey and return them anonymously in a prepaid envelope, with a reminder sent after two weeks to non-respondents.
To perform this study, authors developed a questionnaire containing 17 categorical questions to determine the attitudes of Korean obstetricians and gynecologists regarding the cervical cancer screening. Respondents were asked to discuss major concerns and issues that they receive from patients about cervical cancer screening. The questions used either single- or multiple-choice responses. An introductory letter requesting participation was enclosed, and a survey that could be completed in 10 min or less was sought to encourage participation. The questions were structured as clinical vignettes on several subjects, including age to begin and end screening, screening frequency, screening post-hysterectomy, pregnancy screening, screening techniques being used, and concurrent HPV DNA testing.
The questionnaire was prepared in 3 stages. First, the questions were selected based on discussions with 9 gynecologists who perform gynecologic oncology service. The physicians then reviewed the questionnaire and the wording. Questions were revised for content and clarity. Finally, the survey questionnaire was field tested by 35 obstetricians and gynecologists who were either in the course of residency or fellowship in Seoul National University Hospital.
Surveys were returned to one investigator and data was abstracted and recorded by a research assistant. All questionnaires returned were given a sequential identification number. The questionnaires were hand-checked for completeness and coded before data entry. The data were examined by simple frequency counts because the primary aim of current study was to describe the attitudes and practices of physicians. Student t test was used to compare the differences of the variables. A p-value <0.05 was considered statistically significant.
Of the 852 questionnaires distributed, 260 (30.6%) were returned. After excluding questionnaires returned with more than 8 questions unanswered (n=6). Two hundred and fifty-four (29.8%) respondents were eligible; 158 (62.2%) were male, 78 (30.7%) were female, and 18 (7.1%) did not supply information on gender.
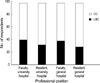
Table 1 and Fig. 1 show the characteristics of respondents. Their mean (standard deviation) age was 40.3 (10.8) yr. The majority of were male, and performed 1-15 Pap tests per week. Table 2 summarizes patient's age when respondents began screening. The majority of respondents would screen a 20-yr-old patient regardless of sexual activity (68.1% for sexually active and 66.9% for not active respectively), and 79.9% of respondents would screen a 20-yr-old patient at her first visit for antenatal care. Most respondents were reluctant to perform cervical cancer screening in woman without history of sexual intercourse, however, 27.2% of respondents replied that they would screen 35-yr-old woman despite absence of sexual intercourse.
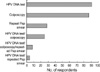
Most respondents replied that they would screen patients annually, and 57.1% that they would screen more frequently if requested by a patient. The respondents' answers on cervical cancer screening intervals after hysterectomy are portrayed in Fig. 2. Most respondents would extend the screening interval or cease screening in a woman with a history of hysterectomy for a non-preinvasive lesion. Most respondents in the current study preferred conventional cytologic screening method to liquid-based cystology (LBC) regardless of their professional position and practice setting, and the Fig. 3 summarizes the result. Fig. 4 shows that most (65.8%) respondents preferred conventional cervical cytologic testing to LBC, and the major determining factor was high cost. The reasons for selecting screening method were different in these two groups (p<0.001, Student t test). The attitudes of respondents toward the ACS cervical cancer screening guidelines are listed in Table 3. According to the table, the majority of respondents (58.7%) agreed 2-yr screening interval using liquidbased cytologic testing. However, if the option became available to combine screening with Pap and HPV DNA testing every 3 yr, 33.9% would adopt this strategy, but 65.7% of respondents would not adopt it despite negative results by both Pap and HPV DNA testing. The respondents' answers on the strategy adopted in those with an abnormal cytology, and on the preferred follow-up method are shown (Fig. 5). Most respondents (80.3%) replied that they use a HPV DNA test and Pap for follow-up after a loop electrosurgical excision procedure (LEEP) for preinvasive cervical lesions.
It is the first report on the screening preferences of Korean obstetricians and gynecologists. Most respondents began cervical cancer screening at age 20 yr, and screened annually despite the recommendations of the ACS and ACOG, which allow less frequent screening. This may be due to a higher incidence of cervical cancer in Korea (18.4 per 100,000 in Korea 1999-2001) (2) than in the United States (9.2 white women per 100,000 in the U.S.A. 1996-2000) (1).
Investigators have shown preference of continued-screening in the U.S.A., but the proportion of respondents that replied in this manner was a half of that of the present study. Sirovich et al. (12) reported that 69% of their patient study population would try to continue being screened annually even if their doctors recommended less frequent screening and advised them of comparable benefits. Women should be reassured about the low risk of developing cervical cancer within short periods of time after a normal cytology result (13). However, these women also should be aware of the risk of a false positive result and of unnecessary invasive intervention in low-risk women.
LBC has been said to be more sensitive and specific than conventional smears to diagnosis of cervical lesions (14-17). Although pathologists prefer using LBC for reasons of screening accuracy, most practitioners in Korea use conventional cytologic testing as a screening tool. In contrast, the majority of physicians in the U.S.A. use LBC for sample collection (18, 19). The most common reason for using LBC in the U.S.A. may be the 'third-party pays system', and the professional liability system in the U.S.A. and the increasing number of claims in the 1980s against pathologists for failure to diagnose cervical cancer on conventional Pap smears. However, in Korea, the cost of screening using LBC is charged to patient, and government cover half for annual screening using conventional cytology. Harkness et al. (20) reported that thinlayer cytology yielded significantly fewer unsatisfactory results and that is more sensitive at identifying cervical intraepithelial neoplasia. On the contrary, a recent randomized trial showed that the sensitivity of LBC is no greater than the sensitivity of conventional cytology, and proposed careful consideration on adopting LBC as a screening method cost especially in low resource settings because of the higher cost (21). A largescale study of the accuracies and cost-effectiveness of the two methods is warranted.
The ACS and ACOG recommend the discontinuation of screening after removal of cervix in women without a history of previous cervical disease (10, 11). Sirovich and Welch (22) reported that two thirds of U.S.A. women who have undergone hysterectomy reported having had a Pap smear within the past 3 yr despite 1996 recommendation from the U.S.A. Preventive Services Task Force that routine Pap smear screening is unnecessary in women who have undergone a hysterectomy for benign disease. However, the majority (74.2%) of ACOG fellows responded that they would continue screening such women indefinitely, and the most common reason given for this continuance concerning the adequate testing of women older than 65 yr with a negative history (18). Most respondents of current study are thought to be reluctant to stop screening because there is no consensus or guideline as to when to discontinue cervical cancer screening.
In the present study, about equal numbers of respondents chose HPV DNA testing or colposcopy as next steps in cases with ASCUS. However, Noller et al. (18) reported that most ACOG fellows in the U.S.A. perform colposcopy after an ASCUS result. Moreover, the ASCUS-LSIL Triage Study (ALTS) Group reported that HPV triage is at least as sensitive as immediate colposcopy for detecting cervical intraepithelial neoplasia (CIN) grade 3 among women with ASCUS (23). ALTS longitudinal data suggest that HPV triage is the most effective strategy for the management of women with ASCUS, as was previously suggested by a cost-utility analysis based on a model that closely approximated ALTS (24).
Authors did not include questions concerning the intentions of simultaneous screening with a Pap test and HPV DNA testing. Although cytologic screening programs using Pap smears have dramatically reduced cervical cancer incidence and mortality in developed nations, single Pap tests have suboptimal sensitivities, limited reproducibilities, and have produced many equivocal results (25, 26). Sherman et al. (27) investigated combined Pap and HPV DNA testing and concluded that both negative baseline tests were associated with a low risk of CIN3 or cancer during the following 45 months, largely because a negative HPV DNA test is associated with a reduced risk of cervical neoplasia. They proposed that negative combined testing would provide added reassurance and allow screening interval lengthening among lowrisk women. As more physicians are introducing HPV DNA testing in Korea, as case is being made to evaluate the efficacies of primary screening approaches with that of HPV DNA testing via randomized clinical trials.
Current study has a number of limitations. First, the majority of respondents worked at university hospitals, and their responses may not be applicable to the private practice setting, which are more commonly visited by women seeking screening. Second, those who completed and returned the questionnaire may not have been representative of Korean obstetricians and gynecologists. The survey was given to physicians attending a conference, and a large number of the respondents were undergoing residency training at university hospitals, and that this may have influenced results. Third, authors could not know the socioeconomic status of the patients being screened by the respondents in this study, which also may have influenced the method of screening. Fourth, the questionnaire contained no open questions, and thus rationales on debatable issues such as screening frequency and triage after an abnormal Pap results were not available.
In summary, the majority of Korean obstetricians and gynecologists in university or general hospital prefer annual cervical cancer screening by using conventional cervical cytologic testing for cost problem. A more systematic study to assess the general practice pattern would be valuable for establishing nationwide screening strategy.
Figures and Tables
 | Fig. 1Characteristics of respondents. The majority of the respondents worked in university hospitals (A) located in Seoul and metropolitan cities (B). |
 | Fig. 2Respondents' intention of cervical cancer screening according to reasons and duration after hysterectomy. Most respondents replied they would screen annually a 55-yr-old woman with history of cervical dysplasia, irrespective of the time of hysterectomy. |
 | Fig. 3Proportion of physicians using liquid-based cytology (LBC, black chart) and conventional cytology (CC, white chart) according to professional position. |
 | Fig. 4Reasons (white chart, cost; black chart, accuracy) for selecting screening method among respondents (p<0.001, Student t test). Over 90% of physicians who preferred liquid-based cytology replied that they selected it for screening method due to higher accuracy than conventional cytology. |
References
1. Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001. 94:153–156.

2. Ministry of Health and Welfare. 2002 Annual report of Korea Central Cancer Registry. 2003. Seoul:
3. Devesa SS, Young JL Jr, Brinton LA, Fraumeni JF Jr. Recent trends in cervix uteri cancer. Cancer. 1989. 64:2184–2190.

4. Eide TJ. Cancer of the uterine cervix in Norway by histologic type, 1970-84. J Natl Cancer Inst. 1987. 79:199–205.
5. Nieminen P, Kallio M, Hakama M. The effect of mass screening on incidence and mortality of squamous and adenocarcinoma of cervix uteri. Obstet Gynecol. 1995. 85:1017–1021.

6. Coleman MP, Esteve J, Damiecki P, Arslan A, Renard H. Trends in cancer incidence and mortality. IARC Sci Publ. 1993. (121):1–806.
7. Beral V, Hermon C, Munoz N, Devesa SS. Cervical cancer. Cancer Surv. 1994. 19-20:265–285.
8. Benedet JL, Odicino F, Maisonneuve P, Beller U, Creasman WT, Heintz AP, Ngan HY, Pecorelli S. Carcinoma of the cervix uteri. Int J Gynaecol Obstet. 2003. 83:Suppl 1. 41–78.

10. Saslow D, Runowicz CD, Solomon D, Moscicki AB, Smith RA, Eyre HJ, Cohen C. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002. 52:342–362.

11. ACOG Committee on Practice Bulletin: clinical management guidelines for obstetrician-gynecologists. Number 45, August 2003. Cervical cytology screening (replaces committee opinion 152, March 1995). Obstet Gynecol. 2003. 102:417–427.
12. Sirovich BE, Woloshin S, Schwartz LM. Screening for cervical cancer: will women accept less? Am J Med. 2005. 118:151–158.

13. Sawaya GF, McConnell KJ, Kulasingam SL, Lawson HW, Kerlikowske K, Melnikow J, Lee NC, Gildengorin G, Myers ER, Washington AE. Risk of cervical cancer associated with extending the interval between cervical-cancer screenings. N Engl J Med. 2003. 349:1501–1509.

14. Longatto Filho A, Pereira SM, Di Loreto C, Utagawa ML, Makabe S, Sakamoto Maeda MY, Marques JA, Santoro CL, Castelo A. DCS liquid-based system is more effective than conventional smears to diagnosis of cervical lesions: study in high-risk population with biopsy-based confirmation. Gynecol Oncol. 2005. 97:497–500.
15. Abulafia O, Pezzullo JC, Sherer DM. Performance of ThinPrep liquid-based cervical cytology in comparison with conventionally prepared Papanicolaou smears: a quantitative survey. Gynecol Oncol. 2003. 90:137–144.

16. Lim YK, Lim JC, Kim JH, Lee JP, Chang KH, Ju HJ, Ryu HS. Comparison of efficacy between MonoPrep(R) and Papanicolaou smear for cervical cancer screening. Korean J Obstet Gynecol. 2004. 47:109–117.
17. Lee KC, Choi HS, Kim HJ, Kim YS, Jeong KP, Park H, Rim SY, Kim SM, Byun JS, Nam JH, Park CS. The comparison of conventional Pap smear with ThinPrep Pap smear in detecting HSIL and cervix cancer. Korean J Obstet Gynecol. 2002. 45:753–758.
18. Noller KL, Bettes B, Zinberg S, Schulkin J. Cervical cytology screening practices among obstetrician-gynecologists. Obstet Gynecol. 2003. 102:259–265.

19. Saint M, Gildengorin G, Sawaya GF. Current cervical neoplasia screening practices of obstetrician/gynecologists in the US. Am J Obstet Gynecol. 2005. 192:414–421.

20. Harkness CB, Theofrastous JP, Ibrahim SN, Galvin SL, Lawrence HC. Papanicolaou and thin-layer cervical cytology with colposcopic biopsy control. A comparison. J Reprod Med. 2003. 48:681–686.
21. Taylor S, Kuhn L, Dupree W, Denny L, De Souza M, Wright TC Jr. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006. 118:957–962.

22. Sirovich BE, Welch HG. Cervical cancer screening among women without a cervix. JAMA. 2004. 291:2990–2993.

23. Group A-LTSA. Results of a randomized trial on the management of cytology interpretations of atypical squamous cells of undetermined significance. Am J Obstet Gynecol. 2003. 188:1383–1392.
24. Kim JJ, Wright TC, Goldie SJ. Cost-effectiveness of alternative triage strategies for atypical squamous cells of undetermined significance. JAMA. 2002. 287:2382–2390.

25. Solomon D, Schiffman M, Tarone R. Comparison of three management strategies for patients with atypical squamous cells of undetermined significance: baseline results from a randomized trial. J Natl Cancer Inst. 2001. 93:293–299.

26. Stoler MH, Schiffman M. Interobserver reproducibility of cervical cytologic and histologic interpretations: realistic estimates from the ASCUS-LSIL Triage Study. JAMA. 2001. 285:1500–1505.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download