Abstract
The current phase II study was conducted to evaluate the response rate and safety of a combination regimen of biweekly irinotecan plus cisplatin in pretreated patients with advanced gastric cancer. Patients with previously treated metastatic or recurrent gastric cancer received intravenous irinotecan 70 mg/m2 and cisplatin 30 mg/m2 on day 1 and 15 every 4-week cycle. Thirty-two patients were enrolled in the current study. Of these, 31 patients were assessable for efficacy and all for toxicity. No complete response and 5 partial responses were confirmed, giving an overall response rate of 15.6% (95% CI; 2.3-28.9%). The median time to progression and median overall survival for all patients was 113 days and 184 days, respectively. Grade 3/4 neutropenia occurred in 6 patients (18.8%), yet no febrile neutropenia was observed. In addition, grade 3 anorexia was observed in 4 patients (12.5%) and grade 3 diarrhea occurred in 2 patients (6.2%). The combination chemotherapy of biweekly irinotecan and cisplatin was found to be moderately effective and well tolerated in pretreated patients with advanced gastric cancer. Accordingly, this regimen can be regarded as an important second-line treatment option for advanced gastric cancer.
Despite a declining incidence in many developed countries, gastric cancer remains the second most common cause of cancer-related deaths in the world (1) and the most common cancer in Korea (2, 3). Although the prognosis for advanced gastric cancer is poor, combination chemotherapy has improved the quality of life and overall survival compared with the best supportive care in several randomized studies (4-6).
In general, 5-fluorouracil (5-FU)-based or cisplatin-based combination regimens are widely accepted as potential standard therapies with a response rate of around 25-40% and median overall survival of 7-9 months (7). Although a larger proportion of patients with metastatic or recurrent gastric cancer initially respond to chemotherapy, they ultimately progress. In addition, a significant proportion of patients have primary refractory diseases. For these patients, there is no currently established second-line treatment option.
Irinotecan is a hemi-synthetic, water-soluble derivative of the plant alkaloid camptothecin. After conversion to its active metabolite, SN-38, irinotecan acts by inhibiting the eukaryotic enzyme DNA-topoisomerase I (8, 9). As such, irinotecan has shown promising activity in advanced gastric cancer as a single agent or combined with different doses and schedules of cisplatin (10-13). Boku et al. (12) reported a high response rate using a combination of irinotecan and cisplatin against advanced gastric cancer, with an overall response rate of 59% in chemotherapy-naive patients. Ajani et al. (13) also reported a good response rate for irinotecan and cisplatin against advanced gastric or gastro-esophageal junction carcinoma, with an overall response rate of 51%. However, there is very little data evaluating the efficacy of irinotecan in pretreated patients with advanced gastric cancer.
Accordingly, the current phase II trial evaluated the response rate, safety, and time to progression of biweekly irinotecan and cisplatin as a second-line chemotherapy in pretreated patients with advanced gastric cancer.
The current multi-center phase II study included patients who had histologically confirmed metastatic or recurrent gastric adenocarcinoma with at least one unidimensionally measurable lesion, and who had previously received at least one palliative chemotherapy regimen that did not include a topoisomerase I inhibitor. The patients were 18-75 yr of age with a performance status of 0-2 on the Eastern Cooperative Oncology Group (ECOG) scale. In addition, adequate hematological (WBC count ≥4×109/L, platelet count ≥100×109/L, hemoglobin ≥9 g/dL), renal (serum creatinine ≤1.5 mg/dL and creatinine clearance ≥50 mL/min), and hepatic (total bilirubin ≤2.0 mg/dL and serum transaminase level ≤3 times the upper limit of the normal range) levels were also required. Patients were ineligible if they had other severe medical illnesses, CNS metastasis, another active malignancy, or history of anaphylaxis to drugs. Written informed consent was obtained from all patients before enrollment.
The irinotecan and cisplatin were administered on days 1 and 15 every 4 weeks. The irinotecan (70 mg/m2) was dissolved in 500 mL 5% glucose and was infused intravenously over 90 min, and the cisplatin (30 mg/m2) was dissolved in 150 mL saline and was infused intravenously over 60 min. To maintain hydration, a total of 2,000-3,000 mL intravenous fluid was administered. All patients were premedicated with steroids and 5-HT3 inhibitors to prevent emesis. Treatment was continued until disease progression, patient refusal, or an unacceptable toxicity up to 6 cycles.
Treatment was continued at the same dose if patients experienced grade 1 toxicities or other toxicities considered by the investigator unlikely to become serious or life threatening (e.g., alopecia). For all other treatment-related adverse events with a grade 2 intensity or higher, the dose modification scheme described below was implemented. No dose reduction was applied after the first appearance of a grade 2 toxicity, although treatment was interrupted until the toxicity was resolved to grade 0 to 1 and symptomatic treatment initiated where possible. The dose of irinotecan was reduced by 25% in patients who experienced a second occurrence of a given grade 2 toxicity or any grade 3 toxicity. The irinotecan and cisplatin therapy was discontinued if the toxicities did not resolve to grade 0 or 1 within 2 weeks. If patients experienced a third occurrence of a given grade 2 toxicity, a second occurrence of a given grade 3 toxicity, or any grade 4 toxicity, the irinotecan dose was reduced by 50%. The irinotecan and cisplatin were both discontinued if, despite a dose reduction, a given toxicity occurred for a fourth time at grade 2, a third time at grade 3, or a second time at grade 4. Patients were required to meet all the following criteria to begin the next cycle of treatment: platelet count ≥75×109/L; neutrophil count ≥1.5×109/L; resolution or improvement of clinically significant non-hematological adverse events (including diarrhea and mucositis) to grade 0 or 1. If treatment was delayed for 3 weeks, patients were excluded from the study.
A screening assessment, including a medical history, physical examination, ECG, chest radiography, and tumor assessment, was conducted within 2 weeks before starting treatment. Further assessments were also conducted within 7 days before starting treatment, including vital signs, an ECOG performance status, and laboratory tests (hematology, blood chemistry, and urinalysis). Complete blood counts were performed weekly during the first cycle and biweekly during every cycle thereafter, and biochemical tests performed before each cycle. Tumors were measured every two cycles until the tumor progressed. The tumor responses were classified according to the response evaluation criteria in solid tumors (RECIST) guidelines (14); complete response (CR), the disappearance of all target lesions; partial response (PR), a decrease of at least 30% in the sum of the longest diameters of the target lesions; progressive disease (PD), an increase of at least 20% in the sum of the longest diameters of the target lesions or the appearance of one or more new lesions; stable disease (SD), neither sufficient shrinkage to qualify for PR nor sufficient increase to qualify for PD. Patients with a CR or PR required a confirmatory disease assessment at least 4 weeks later. Adverse events were graded according to National Cancer Institute Common Toxicity Criteria (NCI-CTC) version 2.0.
This trial was designed to detect a response rate of 20% as compared to a minimal, clinically meaningful response rate of 5%. A two-stage optimal design proposed by Simon was used for this trial, with 80% power to accept the hypothesis and 5% significance to reject the hypothesis. Allowing for a follow-up loss rate of up to 10%, the total sample size was to be 32 patients with measurable disease. All enrolled patients were included in the intention-to-treat analysis of efficacy. The time to progression and survival analyses were all estimated using the Kaplan-Meier method. The time to progression was calculated from the initiation of second-line chemotherapy to the date of disease progression, and overall survival was measured from the initiation of second-line chemotherapy to the date of the last follow-up or death. The statistical data were obtained using an SPSS software package (SPSS 11.5 Inc. Chicago, IL, U.S.A.).
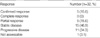
A total of 32 patients were enrolled from 5 medical centers in Korea. The characteristics of the patients are summarized in Table 1. The median age was 54 (range, 27-69) yr, and there were 27 males and 5 females. Many patients (71.9%) had a good performance status (ECOG 0 or 1). Twenty-four (75.0%) patients had a metastatic disease, while 8 patients had a recurrent disease after surgical resection (total or subtotal gastrectomy) of the primary tumor. Distal lymph nodes and the liver were the most common sites of the metastases or recurrences.
The prior treatments are summarized in Table 2. Sixteen patients had previously undergone surgery, one patient had received palliative radiation, and four patients had received 5-FU-based adjuvant chemotherapy. The prior palliative chemotherapies were paclitaxel-based chemotheraoy (62.5%) or docetaxel-based chemotherapy (37.5%), where cisplatin was combined in 10 (31.3%) patients. The responses included 1 CR (3.1%), 10 PR (31.3%), 7 SD (21.9%), and 14 PD (43.8%).
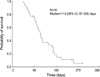
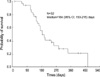
Thirty-one (96.9%) of the 32 patients were assessable for response due to one loss of follow-up. All efficacy data are reported using the intention-to-treat patient population. No CR and 5 PR were confirmed, giving an overall response rate of 15.6% (95% CI; 2.3-28.9%). The response characteristics are shown in Table 3. The median time to progression for all patients was 113 (95% CI; 97-129) days (Fig. 1) with a median follow-up duration of 177 days. Ten patients (31.3%) received third-line chemotherapy after irinotecan and cisplatin failure, and most (90.0%) of these third-line chemotherapy regimens were capecitabine monotherapy. Twenty-two patients had died at the time of the present evaluation. The median overall survival was 184 (95% CI; 153-215) days with an estimated 1-yr survival rate of 21.0% (Fig. 2).
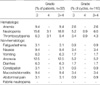
The hematological and non-hematological toxicities are summarized in Table 4. A total of 116 cycles (median 3, range 1-6 cycles) were administrated to 32 patients assessable for toxicity. The most severe hematological adverse event was neutropenia, which occurred with a grade 3/4 intensity in 6 patients (18.8%) and in 7 cycles (6.0%). Yet, no febrile neutropenia was observed. Anorexia was the most common nonhematological toxicity. Grade 3/4 anorexia was observed in 4 patients (12.5%) and in 6 cycles (5.2%). Yet, no grade 4 nonhematologic toxicity was observed. There were no treatment-related deaths during this study. The dose was reduced in 37 cycles and treatment delayed in 11 cycles. The treatment doses were modified for the following reasons: hematological toxicity (43.2%), anorexia (21.6%), nausea (18.9%), and diarrhea (16.2%).
Although systemic chemotherapy is effective in newly diagnosed advanced gastric cancer, second-line chemotherapy for patients where first-line chemotherapy has failed remains a challenge. As such, the current study assessed the clinical efficacy and toxicity of a combination chemotherapy of biweekly irinotecan and cisplatin, which could be administered on an outpatient basis to pretreated patients with advanced gastric cancer. As a result, 5 of 32 (15.6%) enrolled patients achieved an objective response and 15 (46.9%) showed a stable disease, plus the median time to progression and median overall survival was 113 days and 184 days, respectively. Although the response rate was slightly low, the survival time was comparable with previous studies using irinotecan or other agents, including oxaliplatin, paclitaxel, or docetaxel, as second-line treatment in patients with pretreated advanced gastric cancer (15-20).
The major toxicities related to irinotecan are diarrhea and myelosuppression, which are known to be dose dependent. Chemotherapy-induced severe diarrhea or neutropenia can also result in treatment-related hospitalization or mortality, thereby compromising the quality of life and increasing medical expenditure. Thus, in consideration of the second-line treatment setting, we chose a tolerable dose and schedule of the inrinotecan plus cisplatin combination among available regimens showing efficacy against advanced gastric cancer. Ajani et al. reported that the administration of irinotecan (50 mg/m2) and cisplatin (30 mg/m2) weekly for 4 consecutive weeks with 2 weeks rest showed a response rate of 31%, a time to progression of 7 weeks, and median overall survival of 5 months in pretreated patients with advanced adenocarcinoma of the stomach or gastroesophageal junction (15). However, due to the high incidence of toxicities, they also suggested that dose and schedule modifications were warranted to increase the tolerability of the regimen. Recently, Chun et al. reported the phase II study of weekly irinotecan (125 mg/m2 for 4 weeks followed by 2-week rest) in patients with metastatic gastric cancer failing cisplatin-based chemotherapy (18). In their study, the objective response rate was 20% and median overall survival was 5.2 months, yet 67.6% of patients experienced grade 3/4 neutropenia and 18.9% experienced grade 3 diarrhea. However, in the current study, only 18.8% and 6.3% of patients experienced grade 3/4 neutropenia and diarrhea, respectively. Furthermore, there was no febrile neutropenia, treatment-related hospitalization, or grade 4 non-hematologic adverse reaction.
In conclusion, the combination of biweekly irinotecan and cisplatin was found to be moderately effective and well tolerated in pretreated patients with advanced gastric cancer. Accordingly, this regimen can be regarded as an important second-line treatment option for advanced gastric cancer.
Figures and Tables
References
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005. 55:74–108.

2. Korea Gastric Cancer Association. Nationwide gastric cancer report in Korea. J Korean Gastric Cancer Assoc. 2002. 2:105–114.
3. Choi NK, Youn KE, Heo DS, Lee SM, Kim Y, Park BJ. Stomach cancer incidence, mortality and survival rate in Korean Elderly Pharmacoepidemiologic Cohort (KEPEC) in 1994-1998. Cancer Res Treat. 2003. 35:383–390.

4. Murad AM, Santiago FF, Petroianu A, Rocha PR, Rodrigues MA, Rausch M. Modified therapy with 5-fluorouracil, doxorubicin, and methotrexate in advanced gastric cancer. Cancer. 1993. 72:37–41.

5. Glimelius B, Hoffman K, Haglund U, Nyren O, Sjoden PO. Initial or delayed chemotherapy with best supportive care in advanced gastric cancer. Ann Oncol. 1994. 5:189–190.

6. Pyrhonen S, Kuitunen T, Nyandoto P, Kouri M. Randomised comparison of fluorouracil, epidoxorubicin and methotrexate (FEMTX) plus supportive care with supportive care alone in patients with nonresectable gastric cancer. Br J Cancer. 1995. 71:587–591.

7. Wilke HJ, Van Cutsem E. Current treatments and future perspectives in colorectal and gastric cancer. Ann Oncol. 2003. 14:ii49–ii55.

8. Hsiang YH, Lihou MG, Liu LF. Arrest of replication forks by drug-stabilized topoisomerase I-DNA cleavable complexes as a mechanism of cell killing by camptothecin. Cancer Res. 1989. 49:5077–5082.
9. Tanizawa A, Fujimori A, Fujimori Y, Pommier Y. Comparison of topoisomerase I inhibition, DNA damage, and cytotoxicity of camptothecin derivatives presently in clinical trials. J Natl Cancer Inst. 1994. 86:836–842.

10. Futatsuki K, Wakui A, Nakao I, Sakata Y, Kambe M, Shimada Y, Yoshino M, Taguchi T, Ogawa N. Late phase II study of irinotecan hydrochloride (CPT-11) in advanced gastric cancer. Jpn J Cancer Chemother. 1994. 21:1033–1038.
11. Sato A, Kurihara M, Matsukawa M, Shimada K, Yamazaki T, Nakamachi M, Koda T. Preliminary study of fortnightly irinotecan hydrochloride plus cisplatin therapy in patients with advanced gastric and colorectal cancer. Cancer Chemother Pharmacol. 2001. 47:380–384.

12. Boku N, Ohtsu A, Shimada Y, Shirao K, Seki S, Saito H, Sakata Y, Hyodo I. Phase II study of a combination of irinotecan and cisplatin against metastatic gastric cancer. J Clin Oncol. 1999. 17:319–323.

13. Ajani JA, Baker J, Pisters PW, Ho L, Feig B, Mansfield PF. Irinotecan plus cisplatin in advanced gastric or gastroesophageal junction carcinoma. Oncology (Huntingt). 2001. 15:52–54.
14. Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000. 92:205–216.
15. Ajani JA, Baker J, Pisters PW, Ho L, Mansfield PF, Feig BW, Charnsangavej C. Irinotecan/cisplatin in advanced, treated gastric or gastroesophageal junction carcinoma. Oncology (Huntingt). 2002. 16:16–18.
16. Kim DY, Kim JH, Lee SH, Kim TY, Heo DS, Bang YJ, Kim NK. Phase II study of oxaliplatin, 5-fluorouracil and leucovorin in previously platinum-treated patients with advanced gastric cancer. Ann Oncol. 2003. 14:383–387.

17. Assersohn L, Brown G, Cunningham D, Ward C, Oates J, Waters JS, Hill ME, Norman AR. Phase II study of irinotecan and 5-fluorouracil/leucovorin in patients with primary refractory or relapsed advanced oesophageal and gastric carcinoma. Ann Oncol. 2004. 15:64–69.

18. Chun JH, Kim HK, Lee JS, Choi JY, Lee HG, Yoon SM, Choi IJ, Ryu KW, Kim YW, Bae JM. Weekly irinotecan in patients with metastatic gastric cancer failing cisplatin-based chemotherapy. Jpn J Clin Oncol. 2004. 34:8–13.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download