Abstract
The goal of this study was to evaluate the cytomorphologic features of histologically confirmed uterine papillary serous carcinomas (UPSC) of the endometrium. We reviewed cervicovaginal smears from 12 patients with UPSC who had done their cervical smears at six months to a year earlier before the time of diagnosis; nine smears (75%) were diagnosed as positive for malignancy and three smears (25%) were diagnosed as negative. The cervical smears of patients with UPSC revealed frequent papillary clusters that were composed of large pleomorphic tumor cells with prominent nucleoli in a background of necrosis. Other findings revealed from the tests were relatively frequent single malignant cells and bare nuclei. Although the Pap smear is not a sensitive screening test for endometrial carcinoma, we could depend on it to reveal the cytologic features of UPSC which are fairly characteristic and reliable for a preoperative diagnosis of UPSC. Preoperative identification of this poor prognostic variant of endometrial carcinoma may influence the surgical management of these cases and the choice of adjuvant therapy.
Uterine papillary serous carcinoma (UPSC) of the endometrium has been recognized as an aggressive, high grade malignancy that morphologically resembles its ovarian counterpart (1-4). Like papillary serous carcinoma of the ovary, it has a propensity for vascular or lymphatic invasion and peritoneal dissemination as well as early, extensive myometrial invasion (2, 3). In contrast to typical endometrioid carcinoma (TEC) of the endometrium, UPSC is more likely to be identified in cervicovaginal smears (4). Identification of this variant of endometrial carcinoma is clinically valuable because of its aggressive course and poor prognosis. However, descriptions about the cytologic presentation of UPSC have been few and far between in literature. Here in our study, we have reviewed and described the cytologic features of UPSC.
Twenty five cases of UPSC, dating from 1986 to 2004, were retrieved from pathology files at Samsung Cheil Hospital. The histology slides of these cases were reviewed and it was found that twenty two of the cases were diagnosed with pure UPSC. The remaining three cases were diagnosed with a mixed UPSC and endometrioid adenocarcinoma. Twenty three cases had preoperative cervicovaginal smears submitted within one year of the time of the operation or at the time of the operation. Twelve other cases that had cervicovaginal smears with a diagnosis of UPSC were reviewed for this study. All of twelve cases had preoperative endometrial biopsy or curettage to histologically confirm the diagnosis and eight of the patients had hysterectomy.
Histologic samples were evaluated for histologic type, depth of invasion, lymph node and vascular involvement, involvement of the cervix, histologic metastasis and presence of malignant cells in the peritoneal washing fluid.
Cervicovaginal smears were assessed for the presence of excessive blood and acute inflammation, necrosis and psammoma bodies. Cellularity was recorded, as well as the presence of papillae and flat sheets of tumor cells. The occurrence of single cells with intact cytoplasm and bare nuclei were noted. The nuclei of abnormal cells were evaluated for their size, pleomorphism, location and chromatin features. Cytoplasm was evaluated for its amount, density and borders and for the presence of vacuolization and phagocytosis by neutrophils. The amount of cellularity as shown in the cellular smear was subjectively assessed as low, moderate or high, and the remainders of other architectural features were recorded as either present or absent. The presence of psammoma bodies was also noted.
Nine of twelve smears (75%) were originally diagnosed as positive for carcinoma: eight were diagnosed as positive for adenocarcinoma and one was diagnosed as positive for invasive squamous cell carcinoma. In the cytological review diagnosis, this case was confirmed as positive for adenocarcinoma as well as invasive squamous cell carcinoma. Three (25%) of the twelve smears were originally diagnosed as negative and one case revealed a few atypical cells on a cytological review diagnosis. The nine positive samples form the basis of the description of the cytologic features of UPSC (Table 1).
Smears showing malignant cells were distributed into three classifications of cellular smears: two smears were classified as highly cellular, three smears were classified as moderately cellular and four smears revealed a low cellular distribution. Cells were arranged in cellular aggregates, tight ball-like or short papillary clusters and on rare occasions, in flat sheets (Fig. 1). The malignant cells had large nuclei; they were at least two to four times the size of an intermediate cell nucleus. The nuclei were somewhat peripherally displaced and revealed irregular nuclear margins and generally finely clumped chromatin with prominent nucleoli (Fig. 2). Although most tumor cells revealed prominent nucleoli, macronucleoli were inconsistently present in the cervical smears rather than those of histologic sections. The cytoplasm was basophilic, with small vacuoles and indistinct borders. Phagocytosis by neutrophils was found to be less common (in 3 of the 9 cases). Malignant cells predominantly appeared as single cells or bare nuclei in the majority of cases. About 40-50% of the smears contained lysed blood and revealed tumor diathesis (Fig. 3). However, three smears revealed relatively clean backgrounds except for the presence of acute inflammation. Moderate acute inflammation was present in most samples. A few spheroid acellular structures suggestive of psammoma bodies were found in only one smear. Definite laminar concentrations were not found. One smear, which was originally diagnosed as an invasive squamous cell carcinoma, contained cells with a markedly increased nuclear to cytoplasmic ratio and overlapping, highly malignant-appearing nuclei arranged in sheet-like groups. Single cells with dense basophilic or eosinophilic cytoplasm resembling atypical squamous cells were frequently present. Histologically, this case revealed both UPSC and invasive squamous cell carcinoma in the endometrium and the cervix, respectively.
Each of the 12 cases was histologically diagnosed as papillary serous carcinoma. The tumors revealed many short and fibrotic or thin and delicate papillae. The cells covering the papillae and lining glands formed small papillary tufts or floating clusters (Fig. 4). These cells showed high-grade nuclear atypia and often contained a macronucleoli. Slides from hysterectomy specimens were available for review for eight of the patients; only two cases (25%) revealed that the carcinoma invaded less than one half of the myometrium, while six cases (75%) revealed a deep invasion of more than one half of the myometrium. Four (50%) cases revealed cervical involvement by the tumor. Three of the four patients with cervical involvement had positive cervicovaginal smears. Six of the eight cases (75%) revealed lymphovascular tumor invasion. Histologically documented metastases to regional lymph nodes were present in three cases (37.5%). Only a single case (12.5%) had malignant cells in the peritoneal washing fluid (Table 2).
UPSC is a histologically distinct variant of endometrial adenocarcinoma that accounts for approximately 10% of endometrial glandular tumors (5). UPSC is biologically aggressive and is associated with deep myometrial invasion, vascular invasion, lymph node metastases and peritoneal dissemination (2-4, 6).
Cervicovaginal smears are more likely to contain malignant cells in patients with UPSC than those with TEC. Kuebler et al. (4) have described that 65% (11 of 17) of the patients they studied with UPSC had positive cervicovaginal smears whereas only 35% (7 of 20) of the samples from patients with TEC showed malignant cells. Handrickson et al. (2) found that 23% (6 of 26) of patients they studied with UPSC had positive cervicovaginal smears, as compared to 5% of patients with TEC. In this study, we found that 75% (9 of 12) of the patients with UPSC had positive smears. The higher incidence of positive cervicovaginal smears in patients with UPSC may be due to several causes. The majority of UPSCs are moderately to poorly differentiated (2). It has been noted that poorly differentiated endometrial carcinomas are detected more readily on cervicovaginal smears than are their well-differentiated counterparts (7-10). Involvement of the endocervix by the tumor is also prevalent (7, 8, 10); 50% of our UPSC cases revealed endocervical invasion. The fragile nature of papillary fronds of the tumor that readily result in exfoliation may have contributed to the frequency of positive smears.
Differential diagnosis includes a squamous cell lesion (either an invasive carcinoma or high grade squamous intraepithelial lesion) because squamoid cells present both singly and as clusters in a background of tumor diathesis. The squamoid cells reveal hyperchromatic nuclei and dense cytoplasm. A case of histologically proven UPSC and invasive squamous cell carcinoma of the cervix in this study was diagnosed initially on the smear as squamous carcinoma.
Cytology of UPSC may be difficult to distinguish from that of endocervical carcinoma, especially for papillary serous carcinoma of the cervix (PSCC). This is because both UPSC and PSCC show tight balls of cells, small pseudopapillary groups, single cells and a tumor diathesis. However, cervical smears from patients with UPSC do not have the highly cellular smears encountered in PSCC. Furthermore, some of the cell balls in PSCC have some cytoplasm in the center of the ball ("daisy" clusters), whereas cell balls in the more common endometrial carcinoma do not show the absence of nuclei in their centers (11). It may not be possible to distinguish PSC of the endometrium from PSC of the endocervix by morphology alone (4).
Adenosquamous carcinoma of the endocervix may present another diagnostic pitfall. Adenosquamous carcinoma of the cervix is presented as syncytia, sheets and occasional glandular structures comprised of large pleomorphic cells with bulky dense cytoplasm and macronucleoli. Papillae and psammoma bodies are not a prominent feature of adenosquamous carcinoma (12). The recognition of these cellular smears containing pleomorphic cells in sheets and papillary formations with many bare nuclei in the background of the tumor diathesis is helpful.
Extrauterine carcinoma should be included in a differential diagnosis despite its rarity. If fractional curettage of the endometrium and endocervix fails to show carcinoma, an origin from adnexal malignancies should be considered. The prevalence of ovarian adenocarcinoma cells in cervicovaginal smears varies from 6% to 19% (13, 14). The cytologic picture of primary tubal carcinoma is a small number of round or cylindrical malignant cells. Malignant cells are overlapping as they are in papillary or globular formations. The tumor cells have lacy or finely vacuolated cytoplasm with obscuring cell borders (15, 16). Tumor cells of primary Fallopian tube adenocarcinoma found in cervicovaginal smears have been relatively similar to those of UPSC, but the background is clear (without a tumor diathesis) if the disease has not infiltrated into the endometrium (13, 15, 16).
When a cytologic specimen contains cells of adenocarcinoma, it most probably indicates the presence of endometrial carcinoma. The second most probable disease that is indicated is cervical adenocarcinoma/adenosquamous carcinoma (14). In addition, abnormal Pap smears in patients with endometrial carcinoma were significantly associated with prognostic factors such as advanced surgical stage, poor histologic grade, lymphovascular space invasion and cervical invasion (17). Cytologic diagnosis of UPSC should be considered when the cervicovaginal smear contains short, three-dimensional papillary clusters of large malignant cells with prominent nucleoli as well as single malignant cells or bare nuclei in the background of blood or necrosis. Identification of this poor prognostic variant of endometrial carcinoma could be clinically important and preoperative Pap smears could be useful screening method although it is not a sensitive screening test for endometrial carcinoma.
Figures and Tables
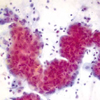 | Fig. 1Cervical smear of uterine papillary carcinoma shows papillary fragment of tumor cells with irregular outline and acute inflammatory cells in background (Papanicolaou stain, ×400). |
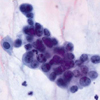 | Fig. 2Tumor cells of uterine papillary serous carcinoma have large nuclei with irregularly distributed chromatin, distinct nucleoli, irregular nuclear margins and indistinct cytoplasmic borders (Papanicolaou stain, ×1,000). |
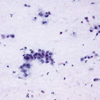 | Fig. 3Cervicovaginal smear of uterine papillary carcinoma shows a papillary cluster and single scattered malignant cells in background of tumor diathesis and lysed blood (Papanicolaou stain, ×400). |
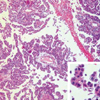 | Fig. 4Histology of uterine papillary serous carcinoma shows short and dense papillae. The cells covering the papillae and lining glands form small papillary tufts or floating clusters (H&E stain, ×100). Tumor cells reveal dense eosinophilic cytoplasm with high grade nulclear atypia (inset, H&E stain, ×400). |
References
1. Christopherson WM, Alberhasky RC, Connelly PJ. Carcinoma of the endometrium. II. Papillary adenocarcinoma: a clinical pathological study, 46 cases. Am J Clin Pathol. 1982. 77:534–540.

2. Hendrickson M, Ross J, Eifel P, Martinez A, Kempson R. Uterine papillary serous carcinoma: a highly malignant form of endometrial adenocarcinoma. Am J Surg Pathol. 1982. 6:93–108.
3. Walker AN, Mills SE. Serous papillary carcinoma of the endometrium. A clinicopathologic study of 11 cases. Diagn Gynecol Obstet. 1982. 4:261–267.
4. Kuebler DL, Nikrui N, Bell DA. Cytologic features of endometrial papillary serous carcinoma. Acta Cytol. 1989. 33:120–126.
5. Ronnett BM, Zaino RJ, Ellenson LH, Kurman RJ. Kurman RJ, editor. Endometrial carcinoma. Blaustein's Pathology of the Female Genital Tract. 2002. 5th ed. New York: Springer;528–533.
6. Slomovitz BM, Burke TW, Eifel PJ, Ramondetta LM, Silva EG, Jhingran A, Oh JC, Atkinson EN, Broaddus RR, Gershenson DM, Lu KH. Uterine papillary serous carcinoma (UPSC): a single institution review of 129 cases. Gynecol Oncol. 2003. 91:463–469.

7. Lozowski MS, Mishriki Y, Solitare GB. Factors determining the degree of endometrial exfoliation and their diagnostic implications in endometrial adenocarcinoma. Acta Cytol. 1986. 30:623–627.
8. Schneider ML, Wortmann M, Weigel A. Influence of the histologic and cytologic grade and the clinical and postsurgical stage on the rate of endometrial carcinoma detection by cervical cytology. Acta Cytol. 1986. 30:616–622.
9. Gu M, Shi W, Barakat RR, Thaler HT, Saigo PE. Pap smears in women with endometrial carcinoma. Acta Cytol. 2001. 45:555–560.

10. Hong SR, Kim HS, Park JS. Significance of cytologic detection of endometrial carcinoma in papanicolaou smear: The relevance of histologic type, grade and stage. Korean J Cytopathol. 1993. 4:81–86.
11. Zhou C, Matisic JP, Clement PB, Hayes MM. Cytologic features of papillary serous adenocarcinoma of the uterine cervix. Cancer. 1997. 81:98–104.

12. Wright CA, Leiman G, Burgess SM. The cytomorphology of papillary serous carcinoma of the endometrium in cervical smears. Cancer. 1999. 87:12–18.

13. Takashina T, Ono M, Kanda Y, Sagae S, Hayakawa O, Ito E. Cervicovaginal and endometrial cytology in ovarian cancer. Acta Cytol. 1988. 32:159–162.
14. Sasagawa M, Nishino K, Honma S, Kodama S, Takahashi T. Origin of adenocarcinoma cells observed on cervical cytology. Acta Cytol. 2003. 47:410–414.

15. Takashina T, Ito E, Kudo R. Cytologic diagnosis of primary tubal cancer. Acta Cytol. 1985. 29:367–372.
16. Hirai Y, Chen JT, Hamada T, Fujimoto I, Yamauchi K, Hasumi K, Masubuchi K, Sakamoto A. Clinical and cytologic aspects of primary fallopian tube carcinoma. A report of ten cases. Acta Cytol. 1987. 31:834–840.
17. Seong SJ, Kim TJ, Lim KT, Chung HW, Lee KH, Park IS, Sihm JU, Park CT, Kim HS. Preoperative pap smears in endometrial carcinoma: The clinicopathologic relevance. Korean J Obstet Gynecol. 2002. 45:1746–1751.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download