Abstract
Hyponatremia and increased urine output after calvarial remodeling have been noted in pediatric patients with craniosynostosis. If not treated properly, patients develop hypoosmotic conditions that can lead to cerebral edema, increased intracranial pressure, and collapsed circulation. Postoperative hyponatremia after central nervous system surgery is considered as the syndrome of inappropriate antidiuretic hormone (SIADH) secretion. Recently, however, cerebral salt wasting syndrome (CSWS) instead of SIADH has been reported frequently. CSWS is associated with a decreased serum sodium level, increased urinary sodium level, increased urine output, decreased ECF volume, increased atrial natriuretic peptide (ANP) level, and increased brain natriuretic peptide (BNP) level. We experienced nine patients with craniosynostosis who underwent calvarial remodeling. By postoperative day 1, the ANP and BNP levels increased by 3-6 folds compared with the preoperative levels. They returned to the normal levels by postoperative day 5. The ADH level was within the normal range even after operation. The urinary sodium level increased in all patients by postoperative day 1 and 3. But the serum sodium level, and serum and urine osmolarity were normal due to appropriate replacement of sodium and fluid. After calvarial remodeling, the potential development of CSWS should be considered and distinguished from SIADH. The patients with CSWS require normal saline resuscitation and should prophylactically receive normal saline.
Hyponatremia and an increased production of urine are frequently observed after calvarial remodeling in patients with craniosynostosis. Hypoosmotic conditions result due to sodium loss in the body when these symptoms are not corrected appropriately, leading to dysfunctional cerebral blood flow, circulation problems, cerebral edema, or increased intracranial pressure. Peters et al. (1) described hyponatremia associated with cerebral disease for the first time in 1950. Initially, the loss of central nervous system control on renal sodium regulation was thought to be the cause so that hyponatremia was termed cerebral salt wasting (CSW). In 1957, however, Schwarz et al. (2) reported the syndrome of inappropriate antidiuretic hormone (SIADH) secretion as hyponatremia after brain disease or brain surgery, and the clinical entity of CSW was viewed as either an extremely rare disorder or a misnomer for what was truly SIADH. Only in recent years has CSW been thought of as a distinct entity, and this recognition has been particularly striking in the field of neurosurgery, where it is viewed as a more common disorder than SIADH (3-5). The clinical findings are more consistent with CSW than SIADH as the cause of postoperative and postinjury fluid and electrolyte changes. Berger et al. showed that the release of one or more natriuretic factors could also play a role in renal salt wasting seen in CSW, in addition to decreased neural input to the kidney (6). Atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP) are important factors in clinically diagnosing CSW.
CSW and SIADH are two conditions that show hyponatremia after central nervous system (CNS) injury. The causes and treatment principles of the two conditions are totally different, and thus the differential diagnosis is critical. Many authors reported the disorder of salt and water homeostasis in patients with brain lesions such as traumatic brain injury, subarachnoid hemorrhage, and brain tumor. However, not much data are available on transient hyponatremia and an increased urinary output after calvarial remodeling (7).
In this study, we evaluated pediatric patients with hyponatremia developing after calvarial remodeling due to premature fusion of cranial sutures to investigate the method of early differential diagnosis between CSWS and SIADH and appropriate treatment methods.
Calvarial remodeling was performed in 9 patients with craniosynostosis from February 2002 to October 2004 in the department of plastic surgery at St. Mary's Hospital. The average age of the patients was 34 months, with a range from 14 months to 6 yr. Total calvarial remodeling was performed in 2 patients with sagittal synostosis. Anterior 2/3 calvarial remodeling was performed in 5 cases of metopic synostosis, 1 case of bicoronal synostosis, and 1 case of frontonasal dysplasia. Although postoperative fluid therapy, intensive care unit stay, and total hospital stay were slightly different the basic method of surgery and treatment protocol after surgery were the same in all patients.
Central vein catheter was inserted in all patients. Immediately after surgery in intensive care unit, vital signs, urinary output per hour, oral intake, and fluid intake were measured. Urinary sodium concentration, urine osmolarity, urine specific gravity, RBC, WBC, prothrombin time (PT), activated partial thrombin time (aPTT), BUN, levels of creatine, albumin, serum sodium and potassium, weight change, and chest radiography were checked every day. The levels of antidiuretic hormone, ANP, and BNP were monitored by postoperative days 1, 3, and 5. After surgery 0.9% normal saline was administered in 9 patients under the strict monitoring of the volume of saline input and amount of urine output.
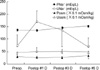
No remarkable event occurred after calvarial remodeling in all of 9 patients. The major parameters measured are shown in Table 1. Although transient hyponatremia was seen during the postoperative period, the serum sodium concentrations (139-141 mEq/L) were within the normal range (135-148 mEq/L) after postoperative day 1 due to normal saline resurscitation that had started immediately after surgery. Urine output was increased in all patients between postoperative 1 and 2 days (>1 mL/kg/hr). Urinary sodium concentration was increased significantly by postoperative 1 and 3 days at 164.89±67.34 mEq/L and 127.89±36.65 mEq/L, respectively, showing a two-fold increase compared with 60±52.59 mEq/L measured before the procedure (p<0.05). It returned to the preoperative level by postoperative day 5 at 53.22±33.98 mEq/L. No significant changes were observed in serum and urine osmolarity during the 5 days after surgery (Fig. 1).
The ANP level was increased significantly by postoperative days 1 and 3 at 108.11±46.01 pg/mL and 87±61.31 pg/mL, respectively (p<0.05). But it fell into the normal range (25-77 pg/mL) by postoperative day 5 at 29.56±18.24 pg/mL, recovering to the preoperative level at 29.57±21.32 pg/mL. The BNP level was also increased dramatically by postoperative day 1 at 149.66±80.49 pg/mL, but decreased to 36.76±21.63 pg/mL by postoperative day 3 and dropped further to 5.02±2.98 pg/mL by postoperative day 5. These figures all showed statistically significant differences (p<0.05). The level of antidiuretic hormone was normal in all patients (0.0-6.7 pg/mL) and showed no statistical significance (Fig. 2).
The length of stay at intensive care unit stay was 4-6 days. Calvarial remodeling was successful without apparent problems in all 9 patients, who recovered and discharged without serious complications.
Hyponatremia is frequently encountered in pediatric patients after calvarial remodeling surgery due to premature fusion of sutures. When this condition is not corrected in a timely manner, it leads to cerebral edema and an increased intracranial pressure as blood flow to CNS is decreased due to low osmolarity. In 1950 Peter et al. (1) coined the term cerebral salt wasting syndrome (CSWS) to describe a decreased volume of extracellular fluid resulting from a decreased serum sodium concentration in not only patients who underwent calvarial remodeling but also those with traumatic CNS injury and those with CNS lesions such as cerebral hemorrhage and brain lesion. It was misunderstood as hyponatremia due to the SIADH reported by Schwarz et al. in 1957 (2). Recently, however, many authors reported that these two metabolic changes are completely different entities having different mechanisms and treatment approaches (3-5).
SIADH is a condition where an increased ECF volume results from an excess production of ADH, which promotes renal water reabsorption. Thus, urine output decreases and urine osmolarity increases since water reabsorption is increased. As a result, weight gain and edema or engorged neck veins are observed, and hyponatremia is also seen due to the effect of dilution (2). However, most cases of SIADH do not typically show edema or engorged neck veins because only 1/3 of total body fluid is extracellular fluid. SIADH results in an increased intravascular volume so that it brings about not only increased renal flow and glomerular filtration rate but also decreased proximal sodium reabsorption and urinary sodium excretion (8). The gold standard protocol for treating SIADH, which show increased body fluid, decreased BUN/creatine ratio, and lower osmolarity, is to restrict water intake.
On the other hand, CSWS is defined as a condition presented with hyponatremia and decreased extracellular fluid volume due to renal loss of sodium in the presence of a disorder of CNS (5) Although the mechanism of CSWS development is poorly understood, the possible mechanisms involve the disruption of neural input into the kidney and/or central elaboration of circulating natriuretic factors. Decreased sympathetic input by disruption of neural input to the kidney could be an explanation for impaired proximal reabsorption because the sympathetic nervous system (SNS) has been shown to alter salt and water handling in the kidney (4). The release of one or more natriuretic factors such as ANP and BNP increases urinary sodium excretion without causing hypokalemia, and ANP and BNP can also directly decrease the autonomic outflow through effects at the brain stem level (6, 8). Either or both of these mechanisms increase urinary sodium excretion, eventually decreasing the effective arterial blood volume and inducing CSWS (8). Berger et al. thought that ADH, ANP, and BNP are the common controlling factors of SIADH and CSWS, which maintain the equilibrium in most cases. However, hyponatremia is induced when these controlling factors lose the equilibrium in pathologic states (6). In SIADH, the ADH secretion is increased, whereas the plasma concentrations of ANP and BNP are normal. However, a normal plasma ADH concentration, markedly increased plasma level of natriuretic peptides, and particularly BNP are observed in CSWS. The patients in this study showed significantly increased levels of ANP and BNP after surgery, with BNP showing a larger increase. On the other hand, ADH showed no significant change after surgery.
The major features of CSWS include a decreased plasma sodium concentration, increased urinary sodium concentration, increased urine output, decreased extracellular fluid, increased levels of ANP and BNP, and increased osmolarity; thus, volume-for-volume fluid and sodium replacement is essential for the treatment of CSWS (4). Our patients also showed these features, confirming the diagnosis of CSWS.
The appropriate treatment for CSWS is maintaining the body fluid volume and balancing the electrolyte concentrations. When CSWS is misdiagnosed as SIADH and treated with fluid restriction, which is the initial method of treatment for SIADH, decreased cerebral perfusion is induced with the development of hemoconcentration, vasospasm and hypotension. Furthermore, if postoperative hyponatremia is not corrected early, it may induce decreased CNS blood flow, cerebral edema, and increased intracranial pressure due to low osmolarity (3). Oral intake of sodium drink is ideal but fluid therapy is needed when oral intake is not possible. When the water and sodium are supplied through intravenous injection, 0.9% normal saline solution or 3% salt solution is the choice. Here, the correction of hyponatremia needs to be done to the levels to prevent the occurrence of central pontine myelinolysis. In addition, the rate of injection of saline solution should be at 1-2 mM/L per hour and should be monitored not to exceed 25 mEq/L per day. Occasionally, an injection of a normal saline solution with blood diuretics such as furosemide is considered (9). The use of corticosteroids (such as Fludrocortisone®) is also possible. Corticosteroids directly act on the distal tubule of the kidney, thereby directly increasing the sodium absorption and improving hyponatremia. However, the use of these drugs should be considered carefully since fatal side effects such as hypertension, hypocalcemia, and pulmonary edema could develop (10).
Many authors reported that CSWS developed in patients with brain lesions such as craniocerebral injuries, subarachnoid hemorrhage, and brain tumor and patients who under went neurosurgery (3-5). However, Levin et al. reported that it is also related with pediatric patients who underwent calvarial remodeling (7). These pediatric patients showed hyponatremia despite appropriate normal saline injection after surgery, natriuresis and increased level of ANP. They stated that the injection of usual pediatric fluid, i.e., 0.25% normal saline, worsened hyponatremia. The pediatric patients in this study showed similar findings after calvarial remodeling as those in the study by Levin et al. (7) and Lee et al. (11), but we could maintain the optimal sodium levels through strict monitoring and resuscitation. Thus, CSWS develops easily in not only patients with brain lesions such as craniocerebral injuries, subarachnoid hemorrhage, and brain tumor and patients who underwent neurosurgery but also pediatric patients who have underwent calvarial remodeling so that complications should be minimized through appropriate early intervention.
In conclusion, the possibility of CSWS should be considered initially in the patients who develop hyponatremia after calvarial remodeling due to craniosynostosis. Although the exact mechanism of the development of CSWS has not been elucidated, the disruption of neural input into the kidney and/or central elaboration of circulating natriuretic factors are considered to be the possible mechanisms. Unlike SIADH requiring fluid restriction, CSWS requires fluid and sodium replacement; thus, differential diagnosis between these two conditions is critical, and the serum ADH, ANP, and BNP levels and urinary sodium level are very important for the differential diagnosis.
Figures and Tables
Fig. 1
Changes of electrolyte values and osmolarity in the patients at preoperative and postoperative 1st-5th day. PNa+, Plasma level of Na+; UNa+, Urine level of Na+; Posm, Plasma osmolarity; Uosm, Urine osmolarity.
References
1. Peters JP, Welt LG, Sims EA, Orloff J, Needham J. A salt wasting syndrome associated with cerebral disease. Trans Assoc Am Physicians. 1950. 63:57–64.
2. Schwartz WB, Bennett W, Curelop S, Bartter FC. A syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med. 1957. 23:529–542.

3. Nelson PB, Seif SM, Maroon JC, Robinson AG. Hyponatremia in intracranial disease: Perhaps not the syndrome of inappropriate secretion of antidiuretic hormone (SIADH). J Neurosurg. 1981. 55:938–941.

5. Betjes MG. Hyponatremia in acute brain disease: the cerebral salt wasting syndrome. Eur J Intern Med. 2002. 13:9–14.

6. Berger TM, Kistler W, Berendes E, Raufhake C, Walter M. Hyponatremia in a pediatric stroke patient: Syndrome of inappropriate antidiuretic hormone secretion or cerebral salt wasting? Crit Care Med. 2002. 30:792–795.

7. Levin JP, Stelnicki E, Weiner HL, Bradley JP, McCarthy JG. Hyponatremia in the postoperative craniofacial pediatric patient population: a connection to cerebral salt wasting syndrome and management of the disorder. Plast Reconstr Surg. 2001. 108:1501–1508.
8. Palmer BF. Hyponatremia in patients with central nervous system disease: SIADH versus CSW. TRENDS in Endocrinology and Metabolism. 2003. 14:182–187.

9. Roca-Ribas F, Ninno JE, Gasperin A, Lucas M, Llubia C. Cerebral salt wasting syndrome as a postoperative complication after surgical resection of acoustic neuroma. Otol Neurotol. 2002. 23:992–995.

10. Albanese A, Hindmarsh P, Stanhope R. Management of hyponatremia in patients with acute cerebral insults. Arch Dis Child. 2001. 85:246–251.
11. Lee SJ, Huh EJ, Byeon JH. Two cases of cerebral salt wasting syndrome developing after cranial vault remodeling in craniosynostosis in children. J Korean Med Sci. 2004. 19:627–630.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download