Abstract
The purpose of this study was to investigate the operative results and the clinical outcomes for octogenarians who underwent cardiac surgery. Twenty consecutive octogenarians who had cardiac operations at Samsung Medical Center from October 1994 through December 2004 were included in the study. The medical records were retrospectively reviewed and the follow-up results were obtained by the interview. The patients were 15 men and 5 women, and their mean age was 83.1 yr (range: 80-89 yr). The surgical priority was urgent for 5 patients and it was elective for 15 patients. Coronary artery bypass grafting (CABG) was performed in 14 patients, valve surgery was performed in 4 patients and CABG plus valve surgery was performed in 2 patients. There was one hospital death on day one after urgent CABG in an 80-yr-old man who had left main coronary artery occlusion. There were three deaths during the follow-up. Sudden death occurred in one patient at 2 months after valve surgery, and there were two non-cardiac deaths at 12 and 14 months, respectively, after CABG. Non-fatal postoperative complications occurred in 2 of 5 urgent patients and in 3 of 15 electives. The survival rate for the 19 hospital survivors at 24 months after surgery was 80% and the mean follow-up period was 22.5 months (range: 1-58 months). In conclusion, cardiac surgery could be performed within acceptable limits of the risk and its long-term results could be expected to be favorable for the octogenarians.
As aging of the population is a current global phenomenon, the need for cardiac surgery is increasing for patients who are aged 80 yr or older. Although several studies have shown that cardiac surgery can be performed safely on octogenarians (1-8), very little information is available on the Korean octogenarians. The purpose of this study is to assess the clinical features and outcomes of the cardiac surgery performed on Korean octogenarians.
Twenty consecutive patients in their 80th year of life or older who underwent cardiac operations at Samsung Medical Center from October 1994 through December 2004 were included in this study. Their medical records were retrospectively reviewed and follow-up information was obtained from these patients during their visits to the outpatient clinic or by telephone interview. Follow-up data were available for all hospital survivors and the mean follow-up period was 22.5±4.0 months (range: 1-58 months). The postoperative complications included myocardial infarction, stroke, congestive heart failure, respiratory failure, renal failure, any rhythm disturbance requiring pacemaker insertion and infections such as pneumonia or wound infection. Myocardial infarction (MI) was diagnosed if there was a new Q wave on the ECG or if there was elevation of the cardiac specific enzymes (CK-MB or cTn-I) in association with persistent ST segment changes. Stroke was defined as any central neurologic deficit lasting for more than 24 hr along with the consistent radiographic findings. Congestive heart failure was diagnosed if pulmonary congestion was found on the physical examination or on the chest radiography films. Respiratory failure was defined as any pulmonary insufficiency requiring mechanical ventilator support for more than 48 hr or if reintubation was necessary. Renal failure was defined as the progressive deterioration of renal function requiring hemodialysis. Pneumonia was defined by the clinical diagnosis with positive cultures of sputum and blood, or if there were radiographic findings consistent with pneumonia. Wound infection was defined as the incision site infection related to the operative procedures with a positive culture or if the infection required antibiotics treatment. The preoperative left ventricular function was assessed by echocardiographic examination. Operative mortality was defined as death within 30 days of the initial operation. The priority of the operation was classified as urgent or elective according to its evaluated clinical condition (elective vs. urgent). Urgent operations were defined as operative procedures performed in those patients whose accelerated symptoms and hemodynamic instability prompted urgent hospitalization and surgical intervention. Statistical analysis was conducted with SPSS version 11.5 software (SPSS, Chicago, IL, U.S.A.). All continuous data are expressed as medians with ranges, and the length of hospital stay was compared by the Mann-Whitney test. The results were considered significant at a level of p<0.05. Survival was determined by the Kaplan-Meier method.
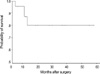
The preoperative clinical characteristics of the patients are listed in Table 1. The associated risk factors included systemic hypertension in 8 patients, diabetes mellitus in 4, previous stroke in 1, previous myocardial infarction in 5, chronic renal failure in 1, and current smoking in 4. Symptomatic peripheral arterial occlusive disease or severe chronic obstructive pulmonary disease was not found in any patient. Nine of 20 patients (45%) presented with congestive heart failure, and 6 of them had pulmonary edema. Six patients had significant anemia with a hemoglobin level<10 g/dL. All surgery procedures were performed through a median sternotomy, and intermittent cold blood cardioplegia (antegrade or retrograde according to surgeon's choice) was used for myocardial protection. The clinical characteristics of operations are summarized in Table 2. In 16 patients with coronary artery bypass grafting (CABG), cardiopulmonary bypass (CPB) was not done in 11 patients (69%) during the operation. For anastomosis of the left anterior descending artery, the left internal thoracic artery (ITA) was used in 13 patients, and the right ITA was used in the remained 3 patients. Additionally, saphenous vein was used in 4 patients, radial artery was used in 2, and a right gastroepiploic artery was used in 1. Among the 6 cases of valve surgery, there was one redo case. An 87-yr-old woman had a repeated mitral valve replacement (MVR) with a 29 mm Carpentier-Edwards porcine bioprosthesis because of perivalvular leakage of the previous 31 mm ATS valve at 94 months after MVR. A preoperative intra-aortic balloon pump (IABP) support was required due to hemodynamic instability in 2 of 5 patients that underwent urgent operations. Besides those 2 patients with IABP, 17 patients received temporary preoperative intravenous inotropic support. For the 15 elective operations, postoperative complications occurred in 3 patients (MI, renal failure and respiratory failure combined with transient complete AV block that required temporary pacing, respectively). For the urgent operations, 2 cases of postoperative complications developed (one incurred respiratory failure, and one had a combined morbidity with MI, leg infection, pneumonia and respiratory failure). The postoperative complications are shown in Table 3. The length of the total hospital stay and the postoperative hospital stay were longer for the patients with postoperative complications (p=0.041 and p=0.018, respectively), and the intensive care unit (ICU) stay was prolonged for patients with urgent operations (p=0.020). The length of the hospital stay is summarized in Table 4. There was one case of operative mortality. An 80-yr-old man with acute myocardial infarction had urgent CABG because of cardiogenic shock with left main coronary artery occlusion. He died one day after the operation due to the cardiogenic shock. The mean duration of follow-up for the 19 hospital survivors was 22.5 months (range: 1-58 months). There were three deaths during the follow-up (Table 5). One male patient died suddenly 2 months after double valve replacement surgery of the mitral valve and aortic valve. He had no preoperative risk factors except smoking and he was discharged from the hospital without complication. A second patient died of pancreatic cancer 12 months after CABG and the patient experienced no further angina after discharge. The third patient died 14 months after CABG due to complications from a traumatic subdural hematoma. The third patient was also free of cardiac symptoms during the follow-up. For the 3 late deaths, the causes of death were not related to cardiac problems in at least 2 cases. The survival rate at 24 months was 80% (Fig. 1).
With the progressively increasing population of the elderly, the need for cardiac surgery in elderly patients is rising. However, the clinical results of cardiac surgery for octogenarians are still under investigation (7-11). In 1985, Rich et al. reported the results of cardiac surgery in 25 consecutive octogenarians with a mortality rate of 4% (1). Since then, many studies have reported various results; yet most of these studies were based on western populations (2-8, 11-18). Although a few studies have reported the results of cardiac surgery in elderly Asians, most of the studies were about septuagenarians (19-22). Mukai et al. reported an operative mortality of 27% in Japanese octogenarians who underwent CABG (23). However, the total number of patients was small and the operative mortality in that study was higher than those rates that were reported in previous studies. Kawachi et al. have recently reported good early and late results for cardiac and thoracic surgery in 40 Japanese octogenarians, of which 9 cases (23%) were surgeries on the thoracic aorta (9). In our study, the operative mortality was 5% (1/20), which was a rate comparable with that observed in previous studies, and the cardiac long term survival of our study was excellent. Long term clinical outcomes have been reported as being excellent in several previous studies (3, 12, 14-18). Freeman et al. have reported that long term survival of the octogenarian patients with cardiac surgery was even better than that observed for the age and gender matched control groups (13). Our study showed that the actuarial survival rates at 1 and 2 yr for the 19 hospital survivors were 88% and 80%, respectively, and these rates correspond with the results of other previous studies.
For the postoperative complication, previous studies have reported that increasing age was a risk factor for not only operative mortality but also for postoperative complications (5, 11, 18). Barnett et al. reported that an age greater than 80 yr was the most significant predictor of postoperative complications (7). The postoperative complication rate in our study was 25% (5/20), which was lower than those of most other studies. There are several possible explanations for this. First, it may have come about because we tried to limit the use of CPB during the surgery. Only 9 patients (45%) underwent cardiac operations with CPB, and CPB increases the risk of the substantial morbidity and mortality, especially in the elderly (24-26), although there has been some controversy about this (27). In our current study, 3 out of the 5 patients that suffered postoperative complications underwent cardiac surgery with CPB. Second, the definition of postoperative complications in our study was more constricted. For example, worsening azotemia that did not require dialysis or any transient arrhythmia that did not require pacemaker insertion was not regarded as a complication. Finally, there may have been a selection bias when choosing the candidates for cardiac surgery. The patients having a better physical condition preoperatively might have been selected more often for surgery. It is well known that urgent operative procedures result in an overall higher risk of morbidity and mortality in octogenarians (3, 12, 13). Ishikawa et al. reported a 4-fold increase in operative mortality in the urgent or emergency operation group compared to the elective cases (10). In our study, there was no operative mortality for the 15 elective operation cases, and one operative death was observed in the 5 urgent cases. The postoperative complication rate for the urgent group (40%, 2/5) tended to be higher than that for elective group (20%, 3/15), although there was no statistically significant difference because of the small number of cases.
Postoperative complications occur more frequently in older patients and this may result in longer hospital stays (18, 28). In our study, the total hospital stay and the postoperative hospital stay were longer for patients with postoperative complications than for those patients without complications. On the other hand, there were no significant differences in the length of the total hospital stay and the postoperative hospital stay between the urgent and elective operation patients. However, the length of ICU stay was longer for the urgent operation patients compared to that of the elective operation patients. These differences suggest that patients who developed postoperative complications need to be hospitalized longer for their treatment, but longer ICU stays were not necessarily needed because those complications were not so serious. For the patients with urgent operations, their hemodynamic status was likely to be more unstable, so intensive care was required more than for those patients with elective operations.
This study is retrospective in nature, and the number of study subjects is relatively small. Yet cardiac surgery performed in octogenarians is still not a widely accepted procedure in Korea, and the current study enrolled all the octogenarian patients who had undergone cardiac surgery in our hospital for the previous 10 yr.
In conclusion, cardiac surgery could be performed with acceptable morbidity and mortality, and favorable long term clinical outcomes could be expected for the octogenarians. Therefore, cardiac surgery should be given more consideration when treating the octogenarians, if such treatment is indicated and necessary.
Figures and Tables
References
1. Rich MW, Sandza JG, Kleiger RE, Connors JP. Cardiac operations in patients over 80 years of age. J Thorac Cardiovasc Surg. 1985. 90:56–60.

2. Edmunds LH Jr, Stephenson LW, Edie RN, Ratcliffe MB. Open-heart surgery in octogenarians. N Engl J Med. 1988. 319:131–136.

3. Mullany CJ, Darling GE, Pluth JR, Orszulak TA, Schaff HV, Ilstrup DM, Gersh BJ. Early and late results after isolated coronary artery bypass surgery in 159 patients aged 80 years and older. Circulation. 1990. 82:IV229–IV236.
4. Cane ME, Chen C, Bailey BM, Fernandez J, Laub GW, Anderson WA, McGrath LB. CABG in octogenarians: early and late events and actuarial survival in comparison with a matched population. Ann Thorac Surg. 1995. 60:1033–1037.

5. Craver JM, Puskas JD, Weintraub WW, Shen Y, Guyton RA, Gott JP, Jones EL. 601 octogenarians undergoing cardiac surgery: outcome and comparison with younger age groups. Ann Thorac Surg. 1999. 67:1104–1110.

6. Alexander KP, Anstrom KJ, Muhlbaier LH, Grosswald RD, Smith PK, Jones RH, Peterson ED. Outcomes of cardiac surgery in patients >or=80 years: results from the National Cardiovascular Network. J Am Coll Cardiol. 2000. 35:731–738.
7. Barnett SD, Halpin LS, Speir AM, Albus RA, Akl BF, Massimiano PS, Burton NA, Collazo LR, Lefrak EA. Postoperative complications among octogenarians after cardiovascular surgery. Ann Thorac Surg. 2003. 76:726–731.

8. Bridges CR, Edwards FH, Peterson ED, Coombs LP, Ferguson TB. Cardiac surgery in nonagenarians and centenarians. J Am Coll Surg. 2003. 197:347–356.

9. Kawachi Y, Nakashima A, Kosuga T, Tomoeda H, Nishimura Y, Toshima Y. Early and late results of cardiac and thoracic aortic surgery in octogenarians: comparison with high-risk younger patients. Circ J. 2003. 67:539–544.
10. Ishikawa S, Buxton BF, Manson N, Hadj A, Seevanayagam S, Raman JS, Rosalion A, Morishita Y. Cardiac surgery in octogenarians. ANZ J Surg. 2004. 74:983–985.

11. Rady MY, Johnson DJ. Cardiac surgery for octogenarians: is it an informed decision? Am Heart J. 2004. 147:347–353.

12. Kolh P, Lahaye L, Gerard P, Limet R. Aortic valve replacement in the octogenarians: perioperative outcome and clinical follow-up. Eur J Cardiothorac Surg. 1999. 16:68–73.

13. Freeman WK, Schaff HV, O'Brien PC, Orszulak TA, Naessens JM, Tajik AJ. Cardiac surgery in the octogenarian: perioperative outcome and clinical follow-up. J Am Coll Cardiol. 1991. 18:29–35.

14. Naunheim KS, Dean PA, Fiore AC, McBride LR, Pennington DG, Kaiser GC, Willman VL, Barner HB. Cardiac surgery in the octogenarian. Eur J Cardiothorac Surg. 1990. 4:130–135.

15. Levinson JR, Akins CW, Buckley MJ, Newell JB, Palacios IF, Block PC, Fifer MA. Octogenarians with aortic stenosis. Outcome after aortic valve replacement. Circulation. 1989. 80:I49–I56.
16. Culliford AT, Galloway AC, Colvin SB, Grossi EA, Baumann FG, Esposito R, Ribakove GH, Spencer FC. Aortic valve replacement for aortic stenosis in persons aged 80 years and over. Am J Cardiol. 1991. 67:1256–1260.

17. Naunheim KS, Kern MJ, McBride LR, Pennington DG, Barner HB, Kanter KR, Fiore AC, Willman VL, Kaiser GC. Coronary artery bypass surgery in patients aged 80 years or older. Am J Cardiol. 1987. 59:804–807.

18. Peterson ED, Cowper PA, Jollis JG, Bebchuk JD, DeLong ER, Muhlbaier LH, Mark DB, Pryor DB. Outcomes of coronary artery bypass graft surgery in 24,461 patients aged 80 years or older. Circulation. 1995. 92:II85–II91.
19. Kosuga K, Aoyagi S, Hara H, Isomura T, Oryoji A, Yamana K, Oishi K. [Cardiovascular surgery in patients seventy years of age and older]. Nippon Geka Gakkai Zasshi. 1991. 92:1111–1114.
20. Nakano S, Takano H, Taniguchi K, Kaneko M, Miyamoto Y, Takahashi T, Matsuda H. [Evaluation of early and late results of open heart surgery in 74 patients 70 years of age and older]. Nippon Geka Gakkai Zasshi. 1991. 92:1139–1142.
21. Shomura T, Okada Y, Nasu M, Sono J, Miyamoto S, Nishiuchi S, Tatemichi K. [Results and problems of open heart surgery in patients seventy years of age and older]. Nippon Geka Gakkai Zasshi. 1991. 92:1131–1134.
22. Ogino H, Ueda Y, Sugita T, Sakakibara Y, Matsuyama K, Matsubayashi K, Nomoto T. Early and mid-term outcomes of cardiac and thoracic aortic surgery in over-75-years-olds with postoperative quality of life assessment. Jpn J Thorac Cardiovasc Surg. 1999. 47:57–62.
23. Mukai S, Murata H, Ueda T, Kita K, Lee S. [Coronary artery bypass grafting in patients aged 80 years or older]. Kyobu Geka. 1997. 50:653–655.

24. Amano A, Hirose H, Takahashi A, Nagano N. Off-pump coronary artery bypass. Mid-term results. Jpn J Thorac Cardiovasc Surg. 2001. 49:67–78.
25. Cleveland JC Jr, Shroyer AL, Chen AY, Peterson E, Grover FL. Off-pump coronary artery bypass grafting decreases risk-adjusted mortality and morbidity. Ann Thorac Surg. 2001. 72:1282–1288.

26. Mack MJ, Pfister A, Bachand D, Emery R, Magee MJ, Connolly M, Subramanian V. Comparison of coronary bypass surgery with and without cardiopulmonary bypass in patients with multivessel disease. J Thorac Cardiovasc Surg. 2004. 127:167–173.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download