Abstract
We report here a case with hypereosinophilia and peripheral artery occlusion. A 32-yr-old Korean woman presented to us with lower extremity swelling and pain. Angiography revealed that multiple lower extremity arteries were occlusive. The biopsy specimen showed perivascular and periadnexal dense eosinophilic infiltration in dermis and subcutaneous adipose tissue. Laboratory investigations revealed a persistent hypereosinophilia. She was prescribed prednisolone 60 mg daily. Her skin lesion and pain were improved and the eosinophil count was dramatically decreased. After discharge, eosinophil count gradually increased again. Cyanosis and pain of her fingers recurred. She had been treated with cyclophosphamide pulse therapy. Her eosinophilia was decreased, but the cyanosis and tingling sense were progressive. The extremity arterial stenoses were slightly progressed. Skin biopsy showed perivascular eosinophilic infiltration in the dermis and CD40 ligand (CD40L) positive eosinophilic infiltration. The serum TNF-α was markedly increased. These results suggest that CD40L (a member of TNF-α superfamily) could play a role in the inflammatory processes when eosinophil infiltration and activation are observed. We prescribed prednisolone, cyclophosphamide, clopidogrel, cilostazol, beraprost and nifedipine, and she was discharged.
Hypereosinophilia is an abnormal condition defined by the presence of more than 500 eosinophils per microliter of blood. Hypereosinophilia occurs in allergic reactions, helminthic infestation, collagen vascular disease and malignancies etc. (1, 2). The diagnosis of the idiopathic hypereosinophilic syndrome is based on exclusion of other causes of hypereosinophilia. That is a disease characterized by unexplained hypereosinophilia persisting for at least 6 months and leading to organ damage (3).
The most common cutaneous manifestations in idiopathic hypereosinophilic syndrome are either erythematous, pruritic papules and nodules or angio-edematous and urticarial plaques. In previous reports, cases with cutaneous vasculitis including eosinophilic infiltration involving small dermal vessel were described (4, 5). Eosinophilic vascular inflammation of those cases showed good response to glucocorticoid treatment.
We report here a case with hypereosinophilia and peripheral artery occlusion. It differs from cutaneous eosinophilic vasculitis and particularly has no internal organ involvement. This case has many differences from typical idiopathic hypereosinophilic syndrome.
A 32-yr-old Korean woman presented with lower extremity swelling and pain.
One year and three months ago, she developed swelling and itching sense in both lower extremities. She visited an orthopedic clinic and was prescribed antibiotics with the impression of having a cellulitis for 1 month. But, this swelling progressed to her both hands and pain was developed. Bluish discoloration then appeared at both hands and legs together with necrosis at some areas. Laboratory investigations revealed a persistent hypereosinophilia (9,374-16,358/µL). Lower extremity CT angiography showed that multiple lower extremity arteries were occlusive. A biopsy specimen from her foot showed perivascular and periadnexal dense eosinophilic infiltration in dermis and subcutaneous adipose tissue. Bone marrow finding showed reactive eosinophilia. We performed microscopic stool exam, ELISA for parasitic antibody, skin prick test for common allergens and bronchial provocation test. She had no evidence of parasitic, allergy, connective tissue disease or other known causes of eosinophilia. She was prescribed oral prednisolone 60 mg, aspirin 100 mg, clopidogrel 75 mg, and beraprost (PGI) 60 mg daily. Her skin lesion and pain were improved and the eosinophil count was dramatically decreased (12-92/µL). One month later after discharge, eosinophil count gradually increased up to 3,465/µL again. Six months later after her discharge, cyanosis and pain of her fingers recurred. A Doppler scan on the extremities was carried, which showed no significant interval change. She was treated with cyclophosphamide pulse therapy five times. Her eosinophilia was then decreased to about 1,000/µL, but the cyanosis and tingling sense were progressive. She received a sympathectomy procedure by the thoracoscopic approach in order to relieve her tingling sense.
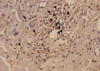
She then visited our hospital and received re-evaluation. Her fingertips were gangrenous (Fig. 1). CT angiography on the upper extremity and lower extremity was done. It showed that the lower extremity arterial stenosis slightly progressed compared with previous study and upper extremity arteries below the wrist level had multiple stenosis (Fig. 2, 3). The cerebral and carotid arteries were intact. Liver sonograpy, chest radiography and echocardiography showed no remarkable finding. Skin biopsy showed perivascular eosinophilic infiltration in the dermis and CD40 ligand (CD40L) positive eosinophilic infiltration (Fig. 4). The TNF-α was markedly increased more than that of several age-matched healthy persons and other hypereosinophilia patient without vasculitis (Fig. 5).
We judged that her disease had not remitted. We prescribed prednisolone 60 mg, cyclophosphamide 50 mg a day and other drugs such as clopidogrel, cilostazol, beraprost (PGI), and nifedipine, and she was discharged from the hospital. However, further follow-up is needed to evaluate whether symptoms and signs change.
This case has several important characteristics. In most other cases of eosinophilic vasculitis, they are characterized as a glucocorticoid-responsive disorder (4, 6). Yet in this case, although the eosinophil count was decreased after glucocorticoid therapy, vascular occlusion was recurrent and progressive. What is worse, it was persistent after cyclophosphamide therapy. This case involved the relatively medium-sized vessels (popliteal artery, tibia artery, peroneal artery, posterior tibia and proximal superior mesenteric artery). This is a unique feature distinctive from previous reported eosinophilic vasculitis (5, 7, 8). Also, there is no evidence of multi-organ involvement in this case, and this differs from typical idiopathic hypereosinophilic syndrome (9).
Takegawa et al. have described an idiopathic hypereosinophilic syndrome patient with fingertip necrosis and they suggested that tumor necrosis factor (TNF) might play a part in the mechanism (6). CD40 is the receptor for a CD40L, a 35-kDa glycoprotein and a member of the TNF-α superfamily. CD40L, which can be expressed by T cells, mast cells and basophils, has been shown to be involved in the control of B cell proliferation and immunoglobulin class switching, as well as in the activation of monocytes and T cells (10). Gauchat et al. have demonstrated that CD40L can also be expressed constitutively by eosinophils from hypereosinophilic patients (11). Eosinophils were able to induce, in conjunction with IL-4, CD40L-dependent B cell proliferation in vitro. In this case, immunohistochemistry for CD40L revealed that almost all the eosinophils were stained by anti-CD40L monoclonal antibody, and namely CD40L was elevated in tissue. TNF-α in the serum also was dramatically elevated.
The results in this case suggest that CD40L could play a role in the inflammatory processes when eosinophil infiltration and activation are observed, but fine mechanism is still unclear. Further study which elucidates a specific role of the interaction between CD40L and CD40 will be necessary. In clinician's view, factors which decide a steroid responsiveness and involving vessel should be clarified.
Figures and Tables
 | Fig. 2Lower extremity CT angiography; occlusions of right popliteal artery, right posterior tibial artery, right peroneal artery, left posterior tibial, left peroneal artery, left distal anterior tibial artery are seen. |
References
2. Mohri H, Motomura S, Okubo T. Unusual leukocytosis with eosinophilia by an allergic disease. Am J Hematol. 1998; 57:90–91.

3. Kim JC, Lee SK, Kim YG, Moon IS, Kim SN, Koh YB. Hypereosinophilic syndrome accompanied by digital necrosis. J Korean Surg Soc. 2000; 58:740–744.
4. Yomoda M, Inoue M, Nakama T, Mori O, Chen KR, Hashimoto T. Cutaneous eosinophilic vasculitis associated with rheumatoid arthritis. Br J Dermatol. 1999; 140:754–755.
5. Hachulla E, Hatron PY, Janin A, Robert Y, Devulder B. Digital arteritis, thrombosis and hypereosinophilic syndrome: an uncommon complication. Rev Med interne. 1995; 16:434–436.
6. Takekawa M, Imai K, Adachi M, Aoki S, Maeda K, Hinoda Y, Yachi A. Hypereosinophilic syndrome accompanied with necrosis of finger tips. Intern Med. 1992; 31:1262–1266.

7. Ferguson GT, Starkebaum G. Thromboangiitis obliterans associated with idiopathic hypereosinophilia. Arch Intern Med. 1985; 145:1726–1728.

8. Lee MW, Bae JY, Choi JH, Moon KC, Koh JK. Cutaneous eosinophilic vasculitis in a patient with Kimura's disease. J Dermatol. 2004; 31:139–141.

9. Roufosse F, Cogan E, Goldman M. Recent advances in pathogenesis and management of hypereosinophilic syndromes. Allergy. 2004; 59:673–689.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download