Abstract
Serum carcinoembryonic antigen (s-CEA) is used to detect recurrence and predict prognosis in colorectal cancer. However, the cutoff values of s-CEA for prognosis have not been determined. We therefore tried to determine the preoperative s-CEA levels predictive of survivals in colorectal cancer patients. We retrospectively analyzed the medical records of 989 patients who underwent curative resection for colorectal cancer between July 1990 and December 1997, with a mean follow-up of 46 months (range, 3-129 months). When patients were divided into four subgroups with the cutoff values of s-CEA at 3,6, and 17 ng/mL, their 5-yr disease-free survival rates were 85.3% (<3.0 ng/mL), 70.0% (3-6 ng/mL), 64.2% (6-17 ng/mL), and 55.2% (>17 ng/mL) (p<0.001). Multivariate analysis showed that factors predictive of survival included age (p=0.028), tumor stage (p<0.001), cell differentiation (p=0.016), and gross type (p=0.007), location (p=0.003) and preoperative s-CEA (p<0.001). Using the above-described cutoff levels, a significant difference in survival was observed only in patients with stage III tumors (p=0.007) when analyses were performed by stage. We can suggest the new cutoff values of s-CEA used in the present study.
Since its initial description in 1965 (1), carcinoembryonic antigen (CEA) has remained the most thoroughly investigated tumor marker. CEA is an intracellular protein normally found in low concentrations in embryonic and fetal gut, pancreas, and liver cells, as well as in several adult tissues. It may be elevated in smokers and in several malignant and benign conditions of the gastrointestinal tract (2). CEA expressed in large quantities in approximately 95% of colorectal carcinomas, and the relationship between serum CEA (s-CEA) level and colorectal cancer has been studied extensively. It has been shown that preoperative s-CEA levels increases with tumor stage (3), and elevated preoperative s-CEA levels have been found to predict a higher incidence of recurrence (4) in patients with colorectal cancer. In addition, the relationship between preoperative s-CEA level and survival has suggested a predictive value of the former for metastasis or recurrence in colorectal cancer patients (5, 6). At present, s-CEA is measured primarily during follow-up of colorectal cancer patients, so that patients with high s-CEA levels receive more intensive treatment (7).
The prognostic value of preoperative s-CEA has been studied, but no practical cutoff value has been determined. We therefore tried to reassess whether preoperative s-CEA level can be used as a prognostic factor in colorectal cancer patients. In addition, we sought to determine the cutoff values of s-CEA for predicting outcome.
One thousand eighty-three patients had curative resections for stages I, II, and III colorectal cancer at Asan Medical Center between July 1990 and December 1997. Patients in whom preoperative s-CEA level was measured were considered eligible for the study. Patients initially presenting with metastatic disease and those who underwent palliative resection were excluded, leaving a total of 989 patients. Their mean age was 57 yr (range, 21-89 yr); 527 were males, and 462 were females. Median follow-up was 46 months (range, 3-129 months). Of the 989 patients, 164 (16.6%) had stage I, 374 (37.8%) had stage II, and 451 (46%) had stage III tumors.
Serum CEA was measured by enzyme immunoassay (ELISA-2-CEA kit®; CIS Biointernational, Marcule, France). The normal range of s-CEA in our laboratory was set as <6 ng/mL, as determined by measurements in 313 Korean healthy persons using the same kit. The s-CEA levels varied between 0.1 and 6.4 ng/mL, with a mean (±S.D.) of 2.25±1.25 ng/mL (8).
To determine the s-CEA cutoff values that may discriminate between patients with good and those with poor prognosis, we performed a multi-step analysis of survival curve. First, we constructed survival curves according to their preoperative CEA levels, and compared them. Then, we constructed survival curves for patients with levels beginning from 1 ng/mL and increasing by 1 ng/mL increments, and we compared the curves for each s-CEA level independently. If we found several levels, which showed different survivals, they were compared after the group was divided according to all level. We repeated these steps for levels showing a difference in survival. We chose cutoff levels that most clearly divided patients into subgroups with regard to survival rate by the Kaplan-Meier method with a log rank test. Multivariate analysis was calculated by the Cox proportional hazard model. Statistical significance was defined as p<0.05.
When we set the cutoff values of s-CEA at 3, 6, and 17 ng/mL, the patients were divided into four subgroups with significantly different 5-yr disease-free survival rates (p<0.001). Of the 989 patients, 288 (29.1%) had s-CEA below 3 ng/mL, 401 (40.5%) had s-CEA of 3-6 ng/mL, 176 (17.8%) had s-CEA of 6-17 ng/mL, and 124 (12.5%) had s-CEA over 17 ng/mL. The survival rates in these four subgroups were 85.3%, 70.0%, 64.2%, and 55.2%, respectively (Fig. 1). The four subgroups did not differ significantly with respect to age, sex, location of primary tumor or cellular differentiation. We found, however, that, as s-CEA level increased, the gross pattern of diffuse type (p=0.007) and stage III (p<0.001) also increased (Table 1).
Mean preoperative s-CEA levels with respect to AJCC stage were 4.01 ng/mL (range, 1.0-37.5 ng/mL) in stage I, 11.07 ng/mL (range, 0.7-556.0 ng/mL) in stage II and 23.10 ng/mL (rage, 0.7-2510.0 ng/mL) in stage III, but these differences did not achieve statistical significance (p=0.07). When we determined s-CEA levels relative to T and N categories, we found that mean s-CEA level increased progressively by N category (p<0.001), but there was no correlation between mean s-CEA level and T category.
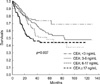
Using the above-described cutoff levels, a significant difference in survival was observed only in patients with stage III tumors (p=0.007), not in those with stages I and II (Fig. 2). By multivariate analysis, preoperative s-CEA level using these new cutoff values was an independent prognostic factor of survival (p<0.001), as were age (p=0.028), tumor stage (p< 0.001), differentiation (p=0.016), and gross type (p=0.007), location (p=0.003) and preoperative s-CEA (p<0.001) (Table 2).
Since its first description, the clinical importance of s-CEA in the management of colorectal cancer patients has been investigated extensively, and it has been reported to predict recurrence or metastasis of this disease (3-6, 9-11). There were several drawbacks to these previous studies, however, including the use of arbitrary cutoff levels. In most studies, survival and recurrence rates were compared between patients with normal s-CEA level and those with elevated s-CEA (9-11), but these groups were not further stratified. In addition, the normal level of s-CEA was set arbitrarily, leading to insufficient determination of the prognostic function of s-CEA level. To correct these possible errors, we stratified s-CEA levels by comparing survival curves of patients below and above each s-CEA level, starting at 1 ng/mL and increasing by increments of 1 ng/mL.
We selected 3, 6, and 17 ng/mL s-CEA as practical cutoff points, which highly discriminate between higher and lower risk groups with respect to survival. In contrast, our evaluation did not attribute any discriminatory function to any other s-CEA level. It is interesting result considering we did not consider the importance of serum CEA, which confined within the normal range usually. Thus, regardless of pathologic stage, these patients could be stratified into subgroups with different prognoses based on their preoperative s-CEA levels, with patients having the highest preoperative s-CEA levels (i.e., >17 ng/mL) having the highest risk of metastasis or recurrence.
CEA is expressed throughout life in normal adult tissues, including the colon, stomach, tongue, cervix, and prostate (1, 12). In the normal colon, CEA may be associated with cellular differentiation, and the degree of expression may be related to differentiation status (13). In colon cancer, CEA appears to provide a variety of cellular functions, including adhesion, in both intracellular and CEA-matrix interactions (14-17), signal transduction, and cellular migration (18-20), suggesting that CEA has a role as a facilitator of tumor invasion and metastasis. On the molecular level, there appears to be no difference between normal colonic CEA and tumor CEA, although the possibility that subtle posttranslational modifications may create differences cannot be excluded (13). Our clinical data suggest that CEA may act in a dose-dependent manner. Thus, enhanced expression of CEA may confer on cancer cells the ability to invade adjacent tissues and to metastasize to lymph nodes or distant organs. Even normal serum levels of CEA may enhance cancer cell invasiveness, giving rise to more aggressive tumor cells.
Tumor stage is the most important predictor of survival in colorectal cancer (5, 6), and s-CEA levels tended to increase progressively with the stage of disease (3). In the present study, preoperative s-CEA level could be correlated with survival only in patients with stage III tumors, not those with stages I and II. This result conflicts with an earlier report (4), in which disease-free survival of patients with Dukes B and C lesions was related to preoperative s-CEA level. Our finding, however, is in agreement with a study showing no such correlation in patients with Dukes B lesions (21). It is not clear whether these differences are due to selection factors, different pathologic staging, small sample sizes, or a combination of these factors. Moreover, when we attempted to coordinate T and N categories of AJCC stage with preoperative s-CEA levels, we found that N, but not T, category was correlated with s-CEA, suggesting a connection of the latter with nodal metastasis.
Our findings suggest that preoperative s-CEA levels could be used as a stratification parameter for identifying subsets of colorectal cancer patients with different prognoses. Especially, patients with preoperative s-CEA above 3.0 ng/mL should be considered at higher risk compared with those with below 3.0 ng/mL, although this value is within the normal range, especially in patients with stage III tumors. In addition, a prospective study is needed to determine the clinical usefulness of these cut-off values.
Figures and Tables
Fig. 1
Disease-free survival curves of colorectal cancer patients relative to preoperative s-CEA levels. Survival is significantly related to preoperative s-CEA levels.
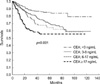
Fig. 2
Preoperative s-CEA levels and disease-free survival rate of stage III colorectal cancer patients.
References
1. Gold P, Freedman SO. Specific carcinoembryonic antigens of the human digestive system. J Exp Med. 1965. 122:467–481.

2. Bendardaf R, Lamlum H, Pyrhonen S. Prognostic and predictive molecular markers in colorectal carcinoma. Anticancer Res. 2004. 24:2519–2530.
3. Palmqvist R, Engaras B, Lindmark G, Hallmans G, Tavelin B, Nilsson O, Hammarstrom S, Hafstrom L. Prediagnostic levels of carcinoembryonic antigen and CA 242 in colorectal cacner: a matched case-control study. Dis Colon Rectum. 2003. 46:1538–1544.
4. Wanebo HJ, Rao B, Pinsky CM, Hoffman RG, Stearns M, Schwartz MK, Oettgen HF. Preoperative carcinoembryonic antigen level as a prognostic indicator in colorectal cancer. N Engl J Med. 1978. 299:448–451.

5. Moertel CG, O'Fallon JR, Go VL, O'Connell MJ, Thynne GS. The preoperative carcinoembryonic antigen test in the diagnosis, staging, and prognosis of colorectal cancer. Cancer. 1986. 58:603–610.

6. Carriquiry LA, Pineyro A. Should carcinoembryonic antigen be used in the management of patients with colorectal cancer? Dis Colon Rectum. 1999. 42:921–929.

7. Wiratkapun S, Karemer M, Sheow-Choen F, Ho YH, Eu KW. High preoperative serum carcinoembryonic antigen predicts metastatic recurrence in potentially curative colonic cancer: results of a five-year study. Dis Colon Rectum. 2001. 44:231–235.
8. Kim JC, Hwang DY, Kim BS, Min YL, Lee MH, Park KC. Changes of serum Careinoembryonic antigen in patients with colorectal cancer. J Korean Cancer Assoc. 1992. 24:880–884.
9. Wolmark N, Fisher B, Wieand HS, Henry RS, Lerner H, Legault-Poisson S, Deckers PJ, Dimitrov N, Gordon PH, Jochimsen P. The prognostic significance of preoperative carcinoembryonic antigen levels in colorectal cancer. Results from NSABP (National Surgical Adjuvant Breast and Bowel Project) clinical trials. Ann Surg. 1984. 199:375–382.
10. Kim DW, Ryu MH, Kim TY, Heo DS, Bang YJ, Park JK, Kim NK. A multivariate analysis of prognostic factors in colorectal cancer. J Korean Med Assoc. 2003. 46:268–274.
11. Harrison LE, Guillem JG, Paty P, Cohen AM. Preoperative carcinoembryonic antigen predicts outcomes in node-negative colon cancer patients: a multivariate analysis of 572 patients. J Am Coll Surg. 1997. 185:55–59.

12. Prall F, Nollau P, Neumaier M, Haubeck HD, Drzeniek Z, Helmchen U, Loning T, Wagener C. CD66a (BGP) an adhesion molecule of the carcinoembryonic antigen family, is expressed in epithelium, endothelium, and myeloid cells in a wide range of normal human tissues. J Histochem Cytochem. 1996. 44:35–41.

13. Bjerner J, Lebedin Y, Bellanger L, Kuroki M, Shively JE, Varaas T, Nustad K, Hammarstrom S, Bormer OP. Protein epitopes in carcinoembryonic antigen. Report of the ISOBM TD8 Workshop. Tumour Biol. 2002. 23:249–262.
14. Benchimol S, Fuks A, Jothy S, Beauchemin N, Shirota K, Stanners CP. Carcinoembryonic antigen, a human tumor marker, functions as an intercellular adhesion molecule. Cell. 1989. 57:327–334.

15. Pignatelli M, Durbin H, Bodmer WF. Carcinoembryonic antigen functions as an accessory adhesion molecule mediating colon epithelial cell-collagen interactions. Proc Natl Acad Sci USA. 1990. 87:1541–1545.

16. Obrink B. CEA adhesion molecules: Multifunctional proteins with signal regulatory properties. Curr Opin Cell Biol. 1997. 9:616–626.
17. Prado IB, Laudanna AA, Carneiro CR. Susceptibility of colorectal-carcinoma cells to natural-killer-mediated lysis: relationship to CEA expression and degree of differentiation. Int J Cancer. 1995. 61:854–860.

18. Kim JC, Rho SA, Park KC. Adhesive function of carcinoembryonic antigen in the liver metastasis of KM-12c colon carcinoma cell line. Dis Colon Rectum. 1997. 40:946–953.

19. Stanners CP, DeMarte L, Rojas M, Gold P, Fuks A. Opposite functions for two classes of genes of the human carcinoembryonic antigen family. Tumour Biol. 1995. 16:23–31.

20. von Kleist S, Miguel I, Halla B. Possible function of CEA as cell-contact inhibitory molecule. Anticancer Res. 1995. 15:1889–1894.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download