Abstract
Kawasaki disease (KD) is a major cause of acquired coronary artery diseases in childhood. The serum levels of matrix metalloproteinase (MMP)-3 and MMP-9 in KD have been reported to be significantly higher than other diseases. Several studies have demonstrated that MMP-3 5A/6A polymorphism and MMP-9 C-1562T polymorphism modify each transcriptional activity in allele specific manner. We hypothesized that these polymorphisms may play a role as a risk factor for development of coronary artery lesions (CAL) in KD. Eighty-three patients, diagnosed with KD in Cheju National University Hospital from January 2000 to February 2004, were divided into two groups according to the presence of CAL. Genotyping of MMP-3 and MMP-9 gene polymorphisms were determined by restriction fragment length polymorphism. With regard to MMP-3 gene polymorphism, the KD with CAL group had a higher frequency of 6A/6A genotype than control group (p=0.0127) and the KD without CAL group (p=0.0036). However, no significant differences in the allele and genotype distributions of the MMP-9 polymorphism were observed. These findings suggest that MMP-3 6A/6A genotype may be an independent risk factor for CAL formation in KD.
Kawasaki disease (KD) is a multi-systemic type of vasculitis including coronary involvement (1). It is an acute, febrile, and exanthematous illness that primarily affects infants and young children characterized by wide spread vascular inflammation of coronary arteries and other medium sized arteries (2). Coronary artery lesions (CAL), coronary artery dilatation or aneurysms, are the most important complications and develop in approximately 15-25% of affected patients with KD (3). Immunological abnormalities during the acute phase of KD are characterized by the activation of immunoregulatory cells and an excess production of inflammatory mediators (4). The activated neutrophils and monocytes, producing a large amount of matrix metalloproteinases (MMPs), migrate into vascular lesions, and newly produced MMPs are thought to be related with coronary artery complications in KD (5).
Polymorphisms of MMP-3 and MMP-9 genes have been reported to be associated with disease susceptibility, severity and progression of atherosclerosis and aneurysms (6-9). The polymorphism in the promoter region of MMP-3 gene on chromosome 11q 22 has been identified (6) and it is bi-allelic with one variant containing a run of 6 adenosines (6A) while the other has five (5A). This MMP-3 5A allele has higher transcriptional activity than 6A allele (10). Two types of polymorphisms in the MMP-9 gene on chromosome 20q 12.2-13.1 have been shown to be functionally important (7). These are a (CA)n microsatellites polymorphism at position -90 (11) and a single nucleotide polymorphism at position -1562 of the translation start site. The cytosine to thymidine transition at position -1562 of the MMP-9 gene is associated with approximately 50% greater promoter activity than that of C-allele (9).
These findings led to us to hypothesize that these polymorphisms, which modify the transcriptional activities of MMPs, could be genetic risk factors for CAL in KD.
One hundred controls with no history of Kawasaki disease (KD), autoimmune disease, or allergic diseases (50 males and 50 females, range 1 to 77 yr olds) were recruited for genotyping of MMP-3 and MMP-9 promoter gene polymorphism. Adult healthy controls were enrolled from subjects attending routine medical check-ups and child controls were admitted for elective surgery or transient acute infection. We retrospectively reviewed the medical records of 121 KD patients at the Cheju National University Hospital, Jeju, Korea, from January 2000 to February 2004. KD was diagnosed according to the criteria proposed by the Japanese Kawasaki Disease Research Committee (12). Echocardiography was obtained within 2 weeks of the onset or before intravenous immunoglobulin administration. Forty-two patients (34.7%) had CALs on echocardiography. The CAL was defined as the criteria proposed by Nakano et al. (13); the largest diameter of coronary artery was greater than 2.5 mm in children with a body surface area (BSA) of less than 0.5 m2, greater than 3 mm in those of BSA between 0.5 and 1 m2 and more than 4 mm in those of BSA more than 1 m2. Among patients diagnosed KD, 83 patients, available for genotyping of MMP gene polymorphism, were enrolled. Of the 83 patients, 34 patients had coronary artery lesion. Patients were divided into two groups according to the presence of CAL: 34 patients with CAL and 49 patients without CAL.
The following laboratory data were analyzed for elucidating of its association with the development of CAL: white blood cell (WBC) counts, platelet counts, erythrocyte sedimentation rate (ESR), alanine aminotransferase (ALT), aspartate aminotransferase (AST), and C-reactive protein (CRP). Data from the patient's first visit to the hospital were obtained.
All controls and parents, whose children were involved in this study, gave written consent to participation and genotyping. This study was approved by the Clinical Research Committee in Cheju National University Hospital.
Genomic DNA was extracted from the peripheral blood using a genomic DNA purification kit (Wizard®; Promega, Madison, WI, U.S.A.) according to the provided protocol. Genotyping of MMP-3 and MMP-9 promoter gene polymorphism were determined by restriction fragment length polymorphism, as previously described (14, 15).
Genotyping of MMP-3 promoter polymorphism was examined with a modification of the method described by Dunleavey et al. (14). In brief, PCR amplification was conducted with the primer (5'-GAT TACAGA CAT GGG TCA CA-3'and 5'-TTT CAA TCA GGA CAA GAC GAA GTT T-3'), annealed to the proximity of the 5A/6A polymorphism. Genomic DNA was amplified in 50 µL of reaction mixture containing 10 pM of each primer, 0.2 mM dNTPs, 2 mM MgCl2, and 2.0 U Taq polymerase (Promega, Madison, WI). The amplification conditions were as follow: 94℃ for 30 sec, 55℃ for 30 sec, and 72℃ for 30 sec, for a total 35 cycles with an extension at 72℃ for 7 min. The resulting 120 bp PCR product was digested Xmn I restriction endonuclease (Promega). The 5A allele, possessing a recognition sequence 5'-GAA (N)4 TTC-3'for Xmn I, cleaved the PCR product to 97 bp and 23 bp fragments. The PCR product deriving from the 6A allele, contains 5'-GAA (N)5 TTC-3'did not digested by Xmn I. Undigested PCR product was sequenced (ABI Prism 377 automatic sequencer) to confirm the 6A allele.
Genomic DNA were PCR-amplified in a 50 µL reaction mixture containing 10 pM of each primers (5'-GCC TGG CAC ATA GTA GGC CC-3'and 5'-CTT CCT AGC CAG CCG GCA TC-3'), 0.2 mM dNTPs, 100 mM Tris-HCl, pH 8.3, 1.5 mM MgCl2, and 2.0 U Taq polymerase (Promega). The amplification conditions were as follow: 95℃ for 1 min, 63℃ for 1 min, and 72℃ for 1 min, for a total 35 cycles with an extension at 72℃ for 5 min. PCR products were digested with 2U of Sph I restriction endonuclease (Promega) over 1 hr at 37℃. The final products were electrophoresed on 2% agarose gel and visualized directly with ethidium-bromide staining. The T allele at Sph I site gives rise to a 435 bp fragment rather than one of 247 bp or 188 bp fragments for C allele.
The SPSS package (SPSS 10.0 for Windows) was used for statistical analysis. Allele frequencies were deduced from genotype frequencies, and differences in the distribution of genotypes were determined by the chi-square test. In order to analyze the comparison of the frequencies of combined genotype between the KD with CAL group and the KD without CAL group, the chi-square test from 2×4 contingency table was applied. Clinical parameters between the KD with CAL group and the KD without CAL group were expressed as mean±standard deviation and were compared by using the Student's t-test. P less than 0.05 were accepted as statistically significant.
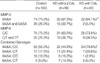
The distributions of the MMP-3 and MMP-9 genotype are shown in Table 1. The observed distributions of the MMP-3 and MMP-9 genotype were in Hardy-Weinberg equilibrium. No significant differences in the distribution of MMP-3 and MMP-9 genotype and allelic frequency were observed between control and patient groups (Table 1). There was no significant difference between the KD with CAL group and KD without CAL group with respect to sex, age at diagnosis, duration of fever, WBC and platelet count, ESR, serum levels of aspartate aminotransferase (AST), and C-reactive protein (CRP) (Table 2). The KD with CAL group demonstrated significantly higher serum levels of alanine aminotransferase (ALT) in acute phase than the KD without CAL group (56.07±66.93 IU/L versus 98.43±113.41 IU/L, p<0.05, Table 2).
We assessed the association of MMP-3 and 9 gene polymorphisms with development of CAL in KD patients. For MMP-9 C-1562T polymorphism, no significant association was observed between control group and the KD with CAL group or the KD without CAL group and the KD with CAL group (Table 3). T allele carriers were more frequently observed in patients without CAL compared with patients with CAD or control group, but these differences were not statistically significant. For MMP-3 gene polymorphism, the KD with CAL group had a higher frequency of 6A/6A genotype than control group (p=0.0127, OR=0.18 (0.03 to 0.84)) and the KD without CAL group p=0.0036, OR=0.13 (0.02 to 0.66), Table 3). For the combination of MMP-3 and MMP-9 gene polymorphism, 4 major combined genotypes in the study groups were 6A/6A C/C, 6A/6A C/T, 6A/5A C/C, and 6A/5A C/T. Combined 6A/5A C/T genotype was not observed in the KD with CAL group (Table 3). The frequency of the 6A/6A C/C genotype was greater in the KD with CAL group than in the KD without CAL group, and the KD with CAL group had less often the 6A/5A C/C genotype than the KD without CAL group (p=0.0169, Table 3).
In KD, CAL appeared within the first 4 weeks of illness, and more than half of CALs were gradually regressed within 1 yr after onset. However, some might be progressed into completely obstructive or markedly stenotic coronary lesions (3). Fujiwara et al. (16) documented four stages in the pathology of the coronary arteries under KD. Acute inflammatory changes are seen in the first 6-9 days in the intima and adventitia, and become panvascular lesions by 12-25 days. Subsequently, aneurysms are seen mostly within the first 2 weeks of the early phase of the disease. During the acute stage, large thrombi are frequently noted, and then marked fibrosis, intimal thickening with recanalization, thrombi, and severe stenosis are seen after 40 days.
MMP-3, an important member of metalloproteinase family, is produced by various types of cells; fibroblasts, smooth muscle cells, and macrophages. MMP-3 potentially contributes to the development of structural alterations in the vessel wall by degradation of extracellular matrix proteins such as proteoglycans, laminin, fibronectin and collagen type III, IV, V and IX (10). MMP-9 is also thought to play an important role in facilitating the extravasation and migration of neutrophils by breaking down the basement membrane (17). Senzaki et al. (5) reported that MMP-9 level in pre-intravenous immunoglobulin (IVIG) therapy and MMP3 level in the post-IVIG therapy were significantly higher in KD patients with CAL than in control group or KD patients without CAL. They also reported that the mean levels of serum MMPs (MMP-2, 3, and 9) were significantly higher in KD patients before IVIG therapy than afebrile control subjects or other febrile disease subjects (18). Cho et al. (19) reported in the study with Korean patients that MMP9 levels were significantly higher before IVIG therapy, and decreased through the convalescent stage. The serum MMP9 levels showed significantly positive correlation with the circulating leukocyte counts. Therefore, we hypothesized that genetic association of MMP activity may play a role as a susceptibility factor for development of CAL in patients with KD.
The MMP-3 5A/6A polymorphism had been analyzed in the association with atherosclerosis and aortic aneurysms. 5A allele, higher promoter activity than 6A allele, was more frequent in patients with abdominal aortic aneurysms, intracranial aneurysms (8) and coronary aneurysms (20). Conversely, 6A allele had been found to be associated with angiographic progression of coronary atherosclerosis (6, 10), restenosis after balloon angioplasty (21) and accelerated growth of coronary atheroma (6). In our study, the KD with CAL group had a higher frequency of 6A/6A genotype than control group or the KD without CAL group. The 6A/6A genotype is a potential susceptibility factor for CAL in our study. This result is paradoxical, given that 6A allele has been associated with lower transcriptional activity and known to insufficient MMP-3 expression (22).
The T allele of C-1562 T MMP-9 polymorphism is associated with approximately 50% greater promoter activity than that of C allele. Jones et al. (23) found that genotypes carrying the T allele of this polymorphism were significantly more common in patients with abdominal aortic aneurysm compared with controls or patients with peripheral vascular disease. They concluded that C-1562T MMP-9 promoter polymorphism is a strong independent risk factor for abdominal aortic aneurysms. In our study, no significant differences in the allele and genotype distributions of the MMP-9 polymorphism were observed. However, T allele carriers were more observed in patients without CAL compared with patients with CAL.
For the combination of MMP-3 and MMP-9 gene polymorphism, the frequency of the 6A/6A C/C genotype was greater in the KD with CAL group than in the KD without CAL group, and the KD with CAL group had less often the 6A/5A C/C genotype than the KD without CAL group. The present results might suggest that development of CAL in patients with KD is more dependent on genotypes of MMP-3 than that of MMP-9.
The serum level of ALT is one of the indices of liver damage and a common test item at the initial examination of patients with KD. The advantage to examine the data obtained at the initial examination is that the ALT in KD patient at the acute stage has not been affected by the salicylate treatment. Uehara et al. (24) reported that the ALT of 50 IU/L or more was noted in 49% of the patients with transient cardiac conditions and 52% of those with persistent cardiac disorders. The elevation of the serum ALT at the initial examination was related to the complications of both transient and persistent cardiac disorders. In our study, the ALT levels in initial examination showed significantly higher in the KD with CAL patients than the KD without CAL patients. However, the changes in ALT level within an individual could not be demonstrated because only the data on the ALT measured at the initial examination were available. Comparing the serum ALT levels for a large number of patients will clarify more effectively the role of ALT in patients with KD.
However, the association of the MMP gene polymorphism with CAL in KD does not necessarily imply that the genetic variation is responsible for the increased risk of CAL. The increased levels of MMPs may be related with increased infiltration of MMPs producing cells in the coronary artery. Moreover, the association of MMP gene polymorphism with CAL in KD may arise from racial differences of the study populations. The frequency of MMP-3 6A allele has been reported to 65% in Finnish (8), 55% in French (20) and 85% in Korean (15). In our study, the prevalence of MMP-3 6A allele was 85.5% in controls and 88.6% in KD patients. The prevalence of MMP-9 T allele was reported to 22.9% in North American, 30% in Swedish and 6% in Korean population (25-27). The frequency of this allele was 13.5% in controls and 17.5% in KD patients in this study.
In conclusion, polymorphism in the MMP promoter gene may be contributed to inter-individual differences of the susceptibility for CAL in KD. This is the first study to evaluate the association of MMP-3 and MMP-9 gene polymorphism with CAL in KD. However, to firmly establish the relationship between MMP-3 and MMP-9 gene polymorphism and CAL in KD, further large-scale studies are required in other populations.
Figures and Tables
ACKNOWLEDGEMENTS
We thank Ji-Eun Park, Department of Pediatrics, Cheju National University College of Medicine, for the excellent technical assistance. This study would not have been possible without the cooperation of the patients and controls.
References
1. Kawasaki T. Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children: Clinical observation of 50 cases. Jpn J Allergy. 1967. 16:178–222.
2. Yanagihara R, Todd JK. Acute febrile mucocutaneous lymph node syndrome. Am J Dis Child. 1980. 134:603–614.

3. Kato H, Ichinose E, Yoshioka F, Takechi T, Matsunaga S, Suzuki K, Rikitake N. Fate of coronary aneu-rysms in Kawasaki disease: serial coronary angiography and long-term follow-up study. Am J Cardiol. 1982. 49:1758–1766.

4. Matsubara T, Furukawa S, Yabuta K. Serum levels of tumor necrosis factor, interleukin 2 receptor, and interferon-gamma in Kawasaki disease involved coronary-artery lesions. Clin Immunol Immunopathol. 1990. 56:29–36.
5. Senzaki H, Masutani S, Kobayashi J, Kobayashi T, Nakano H, Nagasaka H, Sasaki N, Asano H, Kyo S, Yokote Y. Circulating matrix metalloproteinase and their inhibitors in patients with Kawasaki disease. Circulation. 2001. 104:860–863.
6. Ye S, Watts GF, Mandalia S, Humphries SE, Henney AM. Preliminary report: genetic variation in human stromelysin gene promoter is associated with progression of atherosclerosis. Br Heart J. 1995. 73:209–215.
7. Zhang B, Henney A, Eriksson P, Hamsten A, Watkins H, Ye S. Genetic variation at the matrix metalloproteinase-9 locus on chromosome 20q12.2-13.1. Hum Genet. 1999. 105:418–423.

8. Yoon S, Tromp G, Vongpunsawad S, Ronkainen A, Juvonen T, Kuivaniemi H. Genetic analysis of MMP3, MMP9, and PAI-1 in Finnish patients with abdominal aortic or intracranial aneurysms. Biochem Biophys Res Commun. 1999. 265:563–568.

9. Zhang B, Ye S, Herrmann SM, Eriksson P, de Maat M, Evans A, Arveiler D, Luc G, Cambien F, Hamsten A, Watkins H, Henney AM. Functional polymorphism in the regulatory region of gelatinase B gene in relation to severity of coronary atherosclerosis. Circulation. 1999. 99:1788–1794.

10. Ye S, Eriksson P, Hamsten A, Kurkinen M, Humphries SE, Henney AM. Progression of coronary atherosclerosis is associated with a common genetic variant of the human stromelysin-1 promoter which results in reduced gene expression. J Biol Chem. 1996. 271:13055–13060.

11. Shimajiri S, Arima N, Tanimoto A, Murata Y, Hamada T, Wang KY, Sasaguri Y. Shortened microsatellite d(CA) 21 sequence down-regulates promoter activity of matrix metalloproteinase 9 gene. FEBS Lett. 1999. 455:70–74.
12. Japanese Kawasaki Disease Research Committee. Diagnostic guidelines of Kawasaki disease. 1984. 4th ed. Tokyo: Japan Kawasaki Disease Research Committee.
13. Nakano H, Ueda K, Saito A, Nojima K. Repeated quantitative angiograms in coronary arterial aneurysm in Kawasaki disease. Am J Cardiol. 1985. 56:846–851.

14. Dunleavey L, Beyzade S, Ye S. Rapid genotype analysis of the stromelysin gene 5A/6A polymorphism. Atherosclerosis. 2000. 151:587–589.

15. Kim JS, Park HY, Kwon JH, Im EK, Choi DH, Jang YS, Cho SY. The roles of stromelysin-1 and the gelatinase B gene polymorphism in stable angina. Yonsei Med J. 2002. 43:473–481.

16. Fujiwara T, Fujiwara H, Hamashima Y. Frequency and size of coronary arterial aneurysm at necropsy in Kawasaki disease. Am J Cardiol. 1987. 59:808–811.

17. Delclaux C, Delacourt C, D'ortho MP, Boyer V, Lafuma C, Harf A. Role of gelatinase B and elastase in human polymorphonuclear neutrophil migration across the basement membrane. Am J Respir Cell Mol Biol. 1996. 14:288–295.
18. Senzaki H, Kobayashi T, Nagasaka H, Nakano H, Kyo S, Yokote Y, Sasaki N. Plasminogen activator inhibitor-1 in patients with Kawasaki disease: diagnostic value for the prediction of coronary artery lesion and implication for a new mode of therapy. Pediatr Res. 2003. 53:983–988.

19. Cho AR, Hong YM. Matrix metalloproteinase, tissue inhibitors and cytokines in patients with Kawasaki disease. Korean J Pediatr. 2004. 47:656–664.
20. Lamblin N, Bauters C, Hermant X, Lablanche JM, Helbecque N, Amouyel P. Polymorphisms in the promoter regions of MMP-2, MMP-3, MMP-9 and MMP-12 genes as determinants of aneurysmal coronary artery disease. J Am Coll Cardiol. 2002. 40:43–48.

21. Humphries S, Bauters C, Meirhaeghe A, Luong L, Bertrand M, Amouyel P. The 5A/6A polymorphism in the promoter of the stromelysin-1 (MMP3) gene as a risk factor for restenosis. Eur Heart J. 2002. 23:721–725.

22. Ye S. Polymorphism in matrix metalloproteinase gene promoters: implication in regulation of gene expression and susceptibility of various diseases. Matrix Biology. 2000. 19:623–629.

23. Jones GT, Phillips VL, Harris EL, Rossaak JI, van Rij AM. Functional matrix metalloproteinase-9 polymorphism (c-1562T) associated with abdominal aortic aneurysm. J Vasc Surg. 2003. 38:1363–1367.

24. Uehara R, Yashiro M, Hayasaka S, Oki I, Nakamura Y, Muta H, Ishii M, Matsuishi T, Sonobe T, Yanagawa H. Serum alanine aminotransferase concentrations in patients with Kawasaki disease. Pediatr Infect Dis J. 2003. 22:839–842.

25. Wang J, Warzecha D, Wilcken D, Wang XL. Polymorphism in the gelatinase B gene and the severity of coronary arterial stenosis. Clin Sci. 2001. 101:87–92.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download