Abstract
Primary hypothyroidism and type 2 diabetes are both typically associated with the increased level of triglycerides. To date, there have been only a few case reports of type 2 diabetes patients with both type V hyperlipoproteinemia and eruptive xanthomas, but there have been no reports of hypothyroidism patients associated with eruptive xanthomas. We report here on a case of a 48-yr old female patient who was diagnosed with type 2 diabetes and primary hypothyroidism associated with both type V hyperlipoproteinemia and eruptive xanthomas. We found rouleaux formation of RBCs in peripheral blood smear, elevated TSH, and low free T4 level, and dyslipidemia (total cholesterol 18.1 mM/L, triglyceride 61.64 mM/L, HDL 3.0 mM/L, and LDL 2.54 mM/L). She has taken fenofibrate, levothyroxine, and oral hypoglycemic agent for 4 months. After treatment, both TSH level and lipid concentration returned to normal range, and her yellowish skin nodules have also disappeared.
Both diabetes mellitus and primary hypothyroidism are major endocrine disorders leading to secondary hyperlipoproteinemia. In many cases of primary hypothyroidism, the levels of both total cholesterol and low density lipoprotein (LDL) are increased and some cases have a high concentration of triglycerides (1-3). About half of the type 2 diabetes patients were associated with type IV hyperlipoproteinemia, in which the very low density lipoprotein (VLDL) level was usually elevated (4). These type 2 diabetes patients also frequently have type V hyperlipoproteinemia. To date, there have been only a few case reports of type 2 diabetes patients with both type V hyperlipoproteinemia and eruptive xanthomas (5-8), but there has been no report of patients with diabetes mellitus and hypothyroidism associated with eruptive xanthomas.
We report here on a case of a 48-yr old female patient who was diagnosed with type 2 diabetes and primary hypothyroidism associated with both type V hyperlipoproteinemia and eruptive xanthomas.
A 48-yr old female patient was admitted to our hospital because of generalized weakness and right flank pain for several months. She was diagnosed with hypercholesterolemia by biochemical tests, and had rouleaux formations on the peripheral blood smear analysis that was done at a local private clinic (Fig. 1). In order to continue her further evaluation and management, she was transferred to the department of internal medicine of Gyeongsang National University Hospital. She did not complain of any other abdominal pain or tingling sensation on her extremities. According to her past medical history, she was diagnosed as autoimmune thyroiditis and primary hypothyroidism in 1992 and began to take levothyroxine 100 µg daily. However, she took the medicine irregularly and then was lost to follow-up. In 1998, she revisited the of endocrinology and metabolism outpatient department with complaints of generalized weakness and fatigue. She still had hypothyroidism as well as uncontrolled diabetes mellitus and dyslipidemia. Thereafter, she took levothyroxine 100-150 µg daily in combination with a low fat diet and regular exercise therapy. After one month, her thyroid function test revealed the following results; TSH 61.13 mU/L, total T4 61 nM/L, total T3 1.4 nM/L, total cholesterol 8.0 mM/L, triglyceride 9.6 mM/L, HDL cholesterol 0.83 mM/L, and HbA1c 6.6%. After this, she started taking simvastatin and gemfibrozil, but not oral hypoglycemic agents because at this time the fasting blood glucose level was 8.7 mM/L. Thereafter, she did not keep scheduled visit. We could not find any skin symptoms or signs from her medical record. She denied smoking or alcohol intake and took no drugs except levothyroxine irregularly. One sister among the 5 siblings in her family was diagnosed with dyslipidemia (her lipid profiles performed on December 2002 were total cholesterol 8.30 mM/L, LDL cholesterol 4.32 mM/L, HDL cholesterol 1.37 mM/L and, triglyceride 3.7 mM/L). In addition, one of the patients brother has type 2 diabetes mellitus, but he did not have the dyslipidemia.
On the physical examination, her waist circumference and hip circumference was 33 inch and 37 inch (W/H ratio, 0.87) respectively, and the body mass index (BMI) was 26.2 kg/m2. Diffuse goiter with firm consistency was palpated on her anterior neck. Her breathing was clear, and hepatosplenomegaly or tenderness was not found upon abdomen palpation. Several yellowish skin nodules were observed on both her elbows and thighs (Fig. 2A).
On admission, her laboratory findings were as follows; hemoglobin 12.2 g/dL, RBC volume 32%, WBC 5,100/µL, platelet 210,000/µL, postprandial 2 hr blood glucose 14 mM/L, total protein 99 g/L, albumin 44 g/L, total bilirubin 13.6 µM/L, ALP 61 IU/L, AST 24 IU/L, ALT 28 IU/L, BUN 3.7 µM/L and, creatinine 97.5 µM/L. Her serum electrolytes were sodium 124.1 mM/L, potassium 3.5 mM/L, chloride 90 mM/L, calcium 2.5 mM/L, and phosphorus 0.9 mM/L. The urinalysis was normal. Lipid profiles were as follows; total cholesterol 18.1 mM/L, triglyceride 61.64 mM/L, HDL 3.0 mM/L, and LDL 2.54 mM/L. Amylase and lipase levels were normal. The thyroid function tests, determined by a radioimmunoassay method (Immunotech, A Beckman coulter company, France), revealed that she has chronic autoimmune thyroiditis and primary hypothyroidism; TSH 72.69 mU/L (normal range; 0.17-4.05 mU/L), free T4 0.22 ng/dL (normal range; 0.95-2.23 ng/dL), free T3 0.46 pg/mL (normal range; 1.60-3.80 pg/mL). Glycosylated hemoglobin A1c was 9.4%. The excreted protein amount in 24 hr collected urine was 413.7 mg/day. On the second day after admission, a creamy and clouded layer was found in her fasting whole blood that had been placed in the refrigerator for 30 min. The concentration of lipoprotein (a) measured by a rate rephelometry method (Beckman, CA, U.S.A.) was 9 mg/dL. Lipoprotein electrophoresis findings indicated that the patient had type V hyperlipoproteinemia (Fig. 3). Apolipoproteins determined by a single radial immunodiffusion method (Hitachi 7050 chemistry analyser, Japan) were as follows; apolipoprotein C-II 42.0 mg/dL (normal range: 1.5-3.8 mg/dL), apolipoprotein C-III 100 mg/dL (normal range: 5.4-9.0 mg/dL), and apolipoprotein E 27.0 mg/dL (normal range: 2.8-4.6 mg/dL).
We carried out urinalysis and abdominal computed tomography to evaluate her right flank pain and tenderness. Although fatty liver was observed on the abdominal computed tomography, there was no abnormality noted that could be causing pain. Consultation with the rehabilitation department concluded that the patient had fibromyalgia.
The patient was diagnosed as hypothyroidism and type 2 diabetes that presented as hyperlipidemia, and she began to take glimepiride, voglibose, levothyroxine (100 µg daily), and fenofibrate (200 mg). Also, she began to visit the rehabilitation department to help releave her pain. She was then discharged when the blood glucose level and pain have been controlled. She has visited the outpatient department for regular check-ups. She has taken fenofibrate for two months. Currently, the level of both TSH and lipid concentration in blood have returned to the normal values (Table 1). Also, the patient's yellowish skin nodules have disappeared (Fig. 2B).
There are 2 types of hyperlipidemia; one is a primary form caused by genetic abnormalities, the other is the secondary hyperlipidemia resulting from other diseases or medications such as diabetes mellitus, hypothyroidism, nephrotic syndrome, estrogen treatment, and alcohol abuse (9).
Hypothyroidism is classically manifested with an elevation of the plasma LDL cholesterol, and it can also be associated with high plasma triglycerides (1, 2). The HDL cholesterol level is usually unchanged or slightly decreased (10, 11). The elevated plasma LDL cholesterol in hypothyroidism is typically associated with impaired clearance of LDL due to the decreased LDL receptor expression (12, 13). And the elevated triglycerides are induced by decrease of lipoprotein lipase activity (1).
Also, it is well known that dyslipidemia often developed in patients with poorly controlled diabetes mellitus. Type IV dyslipidemia, i.e. an increase of VLDL cholesterol, is the most common form seen in type 2 diabetes, and type IIb, type V, and type IIa dyslipidemia follow.
Xanthomas are the localized deposit of lipids in the skin and these occur rarely in the subcutaneous layer. It is classified as eruptive, tendinous, tuberous, and planar, by deposited anatomic distribution and mode of development (14). The eruptive xanthomas are typically found in patients with severe hypertriglyceridemia, increased chylomicron, and increased VLDL cholesterol. The lesions most commonly develop in type V hyperlipidemia, and they appear on pressure sites such as the extensor surface of the lower and upper extremities and the buttocks (15). Treatment of secondary eruptive xanthomas requires correction of the underlying diseases or removal of the causative agents, and there have been few cases of complete regression reported.
This patient was diagnosed with hypothyroidism and diabetes mellitus in 1998, but at the time plasma glucose and glycosylated hemoglobin A1c level of the patient were not elevated. Hypothyroidism in the patient might have resulted in type V hyperlipoproteinemia because of the increased level of LDL. In addition, this patient showed an elevated level of apolipoproteins in the serum. Typically, apolipoprotein C-II deficiency is associated with type V hyperlipoproteinemia. But, we cannot rule out genetic factors leading to her lipoprotein abnormalities because one of her sisters has hyperlipidemia. From these results, we have assumed that hypothyroidism and insulin resistance in this patient induced hyperlipidemia together with her genetic factors (16). Familial hypertriglyceridemia may be exacerbated by hypothyroidism, estrogen therapy, uncontrolled diabetes mellitus and alcohol. Therefore, determination of the lipid profiles among her family members will clear up the diagnosis. The recovery of her normal lipid profile and the coincidental disappearance of eruptive xanthomas after treatment with fenofibrate, levothyroxine, and oral hypoglycemic agents for two months also suggests that her derangement of lipid metabolism and skin signs are secondary results of the hypothyroidism and diabetes.
This patient also showed the rouleaux formation in her peripheral blood smear. The rouleaux formation, RBCs aggregation, commonly occurs with hypergammaglobulinemia such as multiple myeloma. Hypertriglyceridemia also increases the rouleaux formation rate (17). In many cases, lipemic retinalis and recurrent pancreatitis attacks were associated with hypertriglyceridemia (18), but these conditions did not develop in this case.
In conclusion, our patient who was initially diagnosed with type 2 diabetes and primary hypothyroidism had type V hyperlipoproteinemia as well as eruptive xanthomas. This case report might play an important role for not only showing how to correctly diagnose patients with type 2 diabetes and hypothyroidism that manifest with eruptive xanthomas and rouleaux formation in peripheral blood smear, but also serves as a clinical example for how to effectively treat them.
Figures and Tables
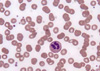 | Fig. 1Rouleaux formation of red blood cells. Peripheral blood smear shows the rouleaux formation of RBCs, a stack of coins (×1,000). |
 | Fig. 2Eruptive xanthoma. (A) Eruptive xanthoma appeared over the elbow of the patient before medication. (B) The lesion of eruptive xanthomas was completely regressed after medications. |
 | Fig. 3A profile of lipoproteins. A result of lipoprotein electrophoresis indicates that the patient has type V hyperlipoproteinemia. There are well defined bands of chylomicrons and grossly elevated pre-β lipoproteins. HDL (α-lipoprotein) and VLDL (pre-β lipoprotein) move with α1-globulins (the most left area) and α2-globulins (first peaks). LDL (β-lipoprotein) migrates with beta-globulins and chylomicron (second peak) remains at the origin. |
References
1. Valdemarsson S, Hansson P, Hedner P, Nilsson-Ehle P. Relations between thyroid function, hepatic and lipoprotein lipase activities, and plasma lipoprotein concentrations. Acta Endocrinol. 1983. 104:50–56.

2. Abrams JJ, Grundy SM. Cholesterol metabolism in hypothyroidism and hyperthyroidism in man. J Lipid Res. 1981. 22:323–338.

3. Mason RL, Hunt HM, Hurxthal L. Blood cholesterol values in hyperthyroidism and hypothyroidism: Their significance. N Engl J Med. 1980. 203:1273–1278.
4. Bierman EL. Insulin and hypertriglyceridemia. Ir J Med Sci. 1972. 8:303–308.
5. Mahley RW, Weisgraber KH, Farese RV Jr. Wilson JD, Foster DW, Kronenberg HM, Larsen PR, editors. Disorders of lipid metabolism. Williams textbook of endocrinology. 1998. 9th ed. Philadelphia: W.B. Saunders Co;1136–1137.
6. Chang JH, Lee SH, Lee SJ, Lee JB. A case of type V hyperlipoproteinemia and xanthoma eruptivum associated with diabetes mellitus. Korean J Dermatol. 2000. 38:561–563.
7. Lee SY, Lee WS, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. A case of type V hyperlipoproteinemia with xanthoma eruptivum. Korean J Dermatol. 2001. 39:935–937.
8. Sordi E, Fargnoli CM, Sordi O, Peris K. Eruptive xanthomas as revealing sign of type V hyperlipoproteinemia in a patient with a psychotic syndrome. Acta Dermatoven APA. 2002. 11.
9. Chait A, Brunzell JD. Acquired hyperlipidemia. Endocrinol Metab Clin North Am. 1990. 19:259–278.
10. Hansson P, Valdemarsson S, Nilsson-Ehle P. Experimental hyperthyroidism in man: effects on plasma lipoproteins, lipoprotein lipase and hepatic lipase. Horm Metab Res. 1983. 15:449–452.

11. Agdeppa D, Macaron C, Mallik T, Schnuda ND. Plasma high density lipoprotein cholesterol in thyroid disease. J Clin Endocrinol Metab. 1979. 49:726–729.

12. Heimberg M, Olubadew JO, Wilcox HG. Plasma lipoproteins and regulation of hepatic metabolism of fatty acids in altered thyroid states. Endocr Rev. 1985. 6:590–607.

13. Scarabottolo L, Trezzi E, Roma P, Catapano AL. Experimental hypothyroidism modulates the expression of the low density lipoprotein receptor by the liver. Atherosclerosis. 1986. 59:329–333.

15. Cruz PD, East C, Bergstresser PR. Dermal, subcutaneous, and tendon xanthomas: diagnostic markers for specific lipoprotein disorders. J Am Acad Dermatol. 1988. 19:95–111.

16. Brunzell JD, Hazzard WR, Motulsky AG, Bierman EL. Evidence for diabetes mellitus and genetic forms of hypertriglyceridemia as independent entities. Metabolism. 1975. 24:1115–1121.

17. Cicha I, Suzuki Y, Tateishi N, Maeda N. Enhancement of red blood cell aggregation by plasma triglycerides. Clin Hemorheol Microcirc. 2001. 24:247–255.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download