Abstract
It has been reported that the particulate matter under 10 µm (PM10) has deleterious effects on respiratory health. The purpose of this study was to assess the influence of PM10 upon normal children's lung function. The subjects were 368 middle school students in two areas of Incheon Metropolitan City. One (Incheon) is in the central city and the other (Ganghwa) is in the suburbs. Air pollution data in the vicinities of two participating schools were obtained from monthly report of air quality from Korean Ministry of Environment in 2000. Pulmonary function testing (PFT) was done two times, the first one in March and the second one in December with the same students. We analyzed the relationship between the PM10 levels and pulmonary functions (FEV1, FVC) of the children. The monthly average of the PM10 level between the two areas showed no significant difference (55.3 vs. 52.3 µg/m3). In both regions, the difference of the PM10 level between March and December was statistically significant (64 vs. 56 µg/m3 in Incheon, 64 vs. 54 µg/m3 in Ganghwa). The findings of the PFT values in March were significantly lower than those values found in December for both regions. In conclusion, we suggest that PM10 has some adverse effect on the pulmonary function of normal children.
Air pollution has been of great concern since the major industrial events associated with air pollution happened in Europe and the United States between the thirties and the fifties (1). Many studies have shown that air pollution is strongly associated with the human health, and the results of air pollution include an increased mortality rate (2-7), an increased number of patients with respiratory or cardiovascular diseases at outpatient departments or emergency rooms (8, 9), the aggravation of asthma (10-15), the increase of respiratory symptoms (16, 17) or the decrease of pulmonary function (18).
Particulate matter of a diameter under 10 µm (PM10) is a mixture of solid and liquid particles in the air, and major sources of these fine particles are diesel engine exhaust, food cooking operations, and dust from wood burning (19). Particles derived from mobiles and stationary combustion sources are more likely to be in the respirable range. The decrease of peak expiratory flow (PEF) in children with asthma has been noted in those places where the density of traffic is heavy (13). Prior studies have found significant associations between concentrations of PM10 and decrements in pulmonary function test (PFT) values for in children with and without asthma (20, 21).
Recently, the number of traffic cars has been continuously increasing in Korea, and not surprisingly, the prevalence of asthma has also been increasing (22). We hypothesized that PM10, which is mainly generated from automobiles, would have deleterious effects on the respiratory tract for even normal children. We also wanted to evaluate the effects of PM10 from the yellow dust storms on the lung function of children. This study was conducted to evaluate the effect of PM10 on the pulmonary function of normal Korean middle school children.
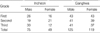
We assumed that middle-school students are more apt to undergo the pulmonary function test and present accurate results, therefore we randomly selected middle school students from two areas of Incheon Metropolitan City; one area is in the central city (Incheon) where the traffic is heavy and the other area is in a suburb (Ganghwa). We randomly selected a few classes in each grade in a school, and the number of students was 124 (male; 75, female; 49) from Incheon and 244 (male; 125, female; 119) from Ganghwa (Table 1). The student subjects were excluded if they had respiratory symptoms within one week before the test and if they had a history of chronic respiratory disease including bronchial asthma and if their growth measurements (height and weight) were over the 97th percentile or below the 3th percentile of Korean standard for their ages.
Pulmonary function testing was done using a portable electric mini-spirometer, in which forced expiratory volume per second (FEV1) and forced vital capacity (FVC) were measured. Prior to pulmonary function testing, a detailed explanation was given to the subjects by the trained examiners. After the test was performed five times, the minimum and maximum values were discarded and the three remaining values were averaged. In March and December of 2000, pulmonary function testing was done repeatedly with the same students. We selected March as the month when the yellow dust storms mainly occurred to evaluate the effects of PM10 on the lung function of healthy children. In addition, we also wanted to evaluate the effects of PM10 generated mainly from automobiles, so we chose December, when the effects of both the yellow dust storms and ozone were minimal.
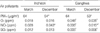
According to the data from the Korean Ministry of Environment in 2000 (23, 24), the mean values of monthly levels of PM10 were 52.3 µg/m3 in Incheon and 55.8 µg/m3 in Ganghwa, and there was no significant difference between the two areas. In March, the mean values of PM10 were the same as 64 µg/m3 in both areas. In December, the mean concentrations of PM10 were 56 µg/m3 and 53 µg/m3 in Incheon and in Ganghwa, respectively, and no statistical significance was noted between the two areas. In both regions, however, the levels of PM10 were higher in March than in December (Table 2). The mean levels of NO2 and SO2 were higher in Incheon than in Ganghwa, but the mean levels of O3 were higher in Ganghwa than in Incheon (Fig. 1, Table 3).
In both regions, the higher academic year was, the greater the FEV1 and FVC values were. Moreover, the FEV1 and FVC values were greater in male students than in female students during the same academic year. The FEV1 and FVC value were greater in December than in March for the same academic year in both areas (Table 4, 5).
The prevalence of asthma has increased worldwide and this has been most strikingly observed in the industrialized countries during the last decade. Epidemiologic studies suggest that environmental factors including air pollution play an important role for the increasing prevalence of asthma. The major air pollutants are CO, NOX, O3, SO2 and particulate matters. Among these pollutants, PM10 can have easily access to the lung via the respiratory tract, and this matter can deposit within the lung (25). According to the study in Utah, U.S.A., during the winter when the level of PM10 was high, the number of patients with respiratory diseases was three times higher than that measured during the winter, when the level of PM10 was low since the steel factory workers went on a strike (26). Moreover, several investigators reported that not only have the number of patients at outpatient department or an emergency room increased, but also the hospitalized or expired patients increased on the days when atmospheric dust was prevalent (8, 9, 27). In Korea, the highest daily level of total suspended particles (TSP) was reported to be correlated with the number of hospitalization for asthma among the patients who were over 40 yr of age (15).
We thought that the levels of PM10 were higher in Incheon than in Ganghwa because the density of traffic is more serious in Incheon. Contrary to our expectations, the levels of PM10 were not statistically different between the two areas, although the levels of NO2 and SO2 were higher in Incheon than in Ganghwa. The pulmonary functions of the students in two areas were not different either. Yet in both areas, the levels of PM10 were higher in March than in December.
The levels of PM10 often exceeded a 24-hr mean level of 150 µm/m3 for Korean environment air quality standards in March. These findings would be due to the yellow dust storms which refers to the wind-blown dust generated from northern China and Mongolia during the spring season. In Korea, yellow dust storms are usually observed in March and May every year, when the level of PM10 exceeds the level of environmental standard by two or three times (28). The size of particulate matter from the yellow dust is mainly 3 µm (29). This range of particulate matter is easily respirable. So it is expected that this kind of particulate matter would have deleterious effects on respiratory system of normal children. Yellow dust storms occurred 4 times during March 2000 in Incheon and Ganghwa (30).
The present study showed that the values of FEV1 and FVC were greater in December than in March for both male and female students at all academic years. Even when taking into consideration the increase of the children's height and weight during the nine months period, the results of pulmonary function test in December were higher than those for the grades one year older, who were checked in March, for almost all grades. Because only the level of PM10 was significantly higher for March than for December in both areas, we suggest that the decrements of pulmonary function in March for both areas are associated with the increased level of PM10 and yellow dust. This particulate matter may have some important role for decrement of pulmonary function.
There are several limitations in this study including the lack of personal exposure data, the possibility of other air pollutant's effects, and lack of exact data of air pollutants on the day when the pulmonary function testing was performed. The levels of NO2 and SO2 were two times higher in Incheon than in Ganghwa and the levels O3 were higher in Ganghwa than in Incheon both for March and for December (Table 3). However, the levels of SO2 and O3 were similar in both May and December in each areas. The levels of NO2 were higher for December than for March in both areas. Therefore, we believe that the decrements of the value of pulmonary function in March were caused by particulate matter.
In conclusion, we can suggest that PM10, especially the particulate matter generated from yellow dust storms may have significant negative effects on the FVC and FEV1 values in normal children.
Figures and Tables
 | Fig. 1Annual mean concentration of major pollutants for Incheon and Ganghwa during the study period. *Reference (30). |
References
2. Schwartz J. Air pollution and daily mortality: a reviews and meta analysis. Environ Res. 1994. 64:36–52.
3. Xu X, Gao J, Dockery DW, Chen Y. Air pollution and daily mortality in residential areas of Beijing, China. Arch Environ Health. 1994. 49:216–222.

4. Touloumi G, Pocock SJ, Katsouyanni K, Trichopoulos D. Short-term effects of air pollution on daliy mortality in Athens: a time-series analysis. Int J Epidemiol. 1994. 23:957–967.
5. Hong YC, Leem JH, Ha EH. Air pollution and daily mortality in Incheon, Korea. J Korean Med Sci. 1999. 14:239–244.
6. Ostro B, Sauchez JM, Aranda C, Eckeland GS. Air pollution and mortality: result from a study of Santiago, Chile. J Expo Anal Environ Epidemiol. 1996. 6:97–114.
7. Lee JT, Lee SI, Shin D, Chung Y. Air particulate matters and daily mortality in Ulsan, Korea. Korean J Prev Med. 1998. 31:82–90.
8. Choi H, Lim DH, Kim JH, Son BK, Lim JW. Study on the interrelationship of air pollution and respiratory disease in Incheon City via children who visited the emergency room of Inha University Hospital. J Korean Pediatr Soc. 2000. 43:1372–1379.
9. Leem JH, Lee JT, Kim DG, Shin DC, Roh JH. Short-term effects of air pollution on hospital visits for respiratory diseases in Seoul. Korean J Occup Environ Med. 1998. 10:333–342.

10. Whittemore AS, Korn EL. Asthma and air pollution in the Los Angeles area. Am J Public Health. 1980. 70:687–696.

11. Vedal S, Petkau J, White R, Blair J. Acute effects of ambient inhalable particles in asthmatic and nonasthmatic children. Am J Respir Crit Care Med. 1998. 157:1034–1043.

12. Timonen KL, Pekkanen J. Air pollution and respiratory health among children with asthmatic or cough symptoms. Am J Respir Crit Care Med. 1997. 156:546–552.

13. Pekkanen J, Timonen KL, Runskanen J, Reponen A, Mirme A. Effects of ultrafine and fine particles in urban air on peak expiratory flow among children with asthmatic symptoms. Environ Res. 1997. 74:24–33.

14. Lipsett M, Hurley S, Ostro B. Air pollution and emergency room visits for asthma in Santa Clara County, California. Environ Health Perspect. 1997. 105:216–222.

15. Choi KW. The association of asthma patients with air pollution [dissertation]. 1994. Seoul: Seoul National University.
16. Pope CA 3rd, Dockery DW. Acute health effects of PM10 pollution on symptomatic and asymptomatic children. Am Rev Respir Dis. 1992. 145:1123–1128.
17. Vigotti MA, Rossi G, Bisanti L, Zanobetti A, Schwartz J. Short term effects of urban air pollution on respiratory health in Milan Italy, 1980-89. J Epidemiol Community Health. 1996. 50:Supp 1. S71–S75.

18. Bedi JF, Folinsbee LJ, Horvath SM. Pulmonary function effects of 1.0 and 2.0 ppm sulfur dioxide exposure in active young male non-smokers. J Air Pollut Control Assoc. 1984. 34:1117–1121.

19. Zheng M, Cass GR, Schauer JJ, Edgerton ES. Source apportionment of PM2.5 in the Southeastern United States using solvent-extractable organic compounds as tracers. Environ Sci Technol. 2002. 36:2361–2371.

20. Koenig JQ, Larson TV, Henley QS, Rebolledo V, Dumler K, Checkoway H, Wang SZ, Lin D, Pierson WE. Pulmonary function changes in children associated with fine particulate matter. Environ Res. 1993. 63:26–38.

21. van der Zee AC, Hoek G, Boezen HM, Schouten JP, van Wijnen JH, Brunekreef B. Acute effects of urban air pollution on respiratory health with and without chronic respiratory symptoms. Occup Environ Med. 1999. 56:802–813.
22. Seo WH, Chang KY, Kim YH, Park SH, Choung JT, Shin YK. The trend for diagnosis and treatment of childhood asthma in Korean pediatricians. Pediatr Allergy Respir Dis. 2002. 12:211–221.
23. Monthly report of air quality. 2000. 03. cited 6 Feb 2004. availabe from URL: http://lib.me.go.kr/imgview_detail.asp.
24. Monthly report of air quality. 2000. 12. cited 6 Feb 2004. availabe from URL: http://lib.me.go.kr/imgview_detail.asp.
25. Subramaniam RP, Asgharian B, Freijer JI, Miller FJ, Anjilvel S. Analysis of lobar differences in particle deposition in the human lung. Inhal Toxicol. 2003. 15:1–21.

26. Gross J, Goldsmith JR, Zangwill L, Lerman S. Monitoring of hospital emergency room visits as a method for detecting health effects of environmental exposures. Sci Total Environ. 1984. 32:289–302.

27. Sunyer J, Anto JM, Murillo C, Saez M. Effects of urban air pollution on emergency room admission for chronic obstructive pulmonary disease. Am J Epidemiol. 1991. 134:277–286.
28. A Report on Yellow Sand. 2000. Ministry of Environment.
29. Kim YH, Kim KS, Kwak NJ, Lee KH, Kweon SA, Lim Y. Cytotoxicity of yellow sand in lung epithelial cells. J Biosci. 2003. 28:77–81.

30. Annual report of ambient air quality in Korea. 2000. cited 6 Feb 2004. available from URL : http://lib.me.go.kr/imgview.asp.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download